What are the top 20 diseases
In the realm of human existence, disease looms as a formidable adversary, casting its shadow on our lives and well-being. From the common cold to debilitating chronic conditions, diseases come in myriad forms, each posing unique challenges and leaving an enduring mark on our health. In this article, we embark on a journey to unveil the top 20 diseases that ravage our world, leaving an indelible imprint on humanity's physical, mental, and societal fabric.
What are the Top 20 Diseases Globally?
Cardiovascular Diseases
Cardiovascular diseases (CVDs) remain a leading cause of death worldwide. This broad category encompasses conditions affecting the heart and blood vessels, including coronary artery disease (CAD), stroke, heart failure, and rheumatic heart disease. Risk factors are numerous and interconnected, involving lifestyle choices (diet, physical activity, smoking), genetics, and age. Prevention focuses on healthy lifestyle modifications and early detection through regular checkups and screenings.
Infectious Diseases
Infectious diseases, caused by bacteria, viruses, parasites, or fungi, continue to pose significant global health challenges. The specific top infectious diseases vary by region and year, but common examples include lower respiratory infections (like pneumonia), HIV/AIDS, tuberculosis, and malaria. Effective prevention strategies include vaccination, sanitation improvements, access to clean water, and prompt treatment with appropriate antibiotics or antiviral medications.
Cancers
Cancer is a broad term for a large group of diseases involving the uncontrolled growth and spread of abnormal cells. Different types of cancer affect various organs and tissues, with varying risk factors and prognoses. Lung cancer, colorectal cancer, breast cancer, and prostate cancer are among the most prevalent globally. Early detection through screening, along with healthy lifestyle choices (avoiding tobacco, maintaining a healthy weight, and regular exercise) are crucial for prevention and improved outcomes.
Respiratory Diseases
Beyond infectious causes, respiratory diseases also include a range of chronic conditions like chronic obstructive pulmonary disease (COPD), which includes emphysema and chronic bronchitis, and asthma. These diseases often involve inflammation and narrowing of the airways, causing breathlessness and other symptoms. Risk factors include smoking, air pollution, and genetic predisposition. Treatment focuses on managing symptoms and preventing exacerbations.
Neurological Disorders
Neurological disorders affect the brain, spinal cord, and nerves, leading to a wide spectrum of impairments. Stroke (often categorized under CVDs as well), Alzheimer's disease, Parkinson's disease, and epilepsy are prominent examples. These conditions can result in cognitive decline, motor difficulties, and seizures. Research continues to explore effective prevention and treatment strategies, focusing on both lifestyle modifications and pharmacological interventions.
| Disease Category | Examples | Major Risk Factors |
|---|---|---|
| Cardiovascular Diseases | Coronary Artery Disease, Stroke, Heart Failure | High blood pressure, high cholesterol, smoking, diabetes |
| Infectious Diseases | Pneumonia, HIV/AIDS, Tuberculosis, Malaria | Poor sanitation, lack of access to healthcare, malnutrition |
| Cancers | Lung Cancer, Colorectal Cancer, Breast Cancer | Tobacco use, genetics, unhealthy diet, lack of physical activity |
| Respiratory Diseases | COPD, Asthma | Smoking, air pollution, genetic predisposition |
| Neurological Disorders | Stroke, Alzheimer's Disease, Parkinson's Disease | Age, genetics, lifestyle factors |
https://youtube.com/watch?v=OmgcOvCHUzI
What are the 20 common diseases?

20 Common Diseases
Infectious Diseases
Infectious diseases are caused by pathogens, such as bacteria, viruses, fungi, or parasites. They can spread from person to person or through contaminated food and water. Prevention often involves vaccination, good hygiene practices, and safe food handling.
- Influenza (Flu): A viral respiratory infection.
- Common Cold: Another viral respiratory infection, typically less severe than the flu.
- Strep Throat: A bacterial infection of the throat.
- Pneumonia: An infection of the lungs.
- Tuberculosis (TB): A bacterial infection that mainly affects the lungs.
Cardiovascular Diseases
Cardiovascular diseases affect the heart and blood vessels. Risk factors include high blood pressure, high cholesterol, smoking, and lack of physical activity. Management often involves lifestyle changes and medication.
- Coronary Artery Disease (CAD): Narrowing of the coronary arteries.
- Heart Failure: The heart's inability to pump enough blood to meet the body's needs.
- Stroke: Disruption of blood supply to the brain.
- High Blood Pressure (Hypertension): Persistently high blood pressure.
- Peripheral Artery Disease (PAD): Narrowing of the arteries in the limbs.
Respiratory Diseases
Respiratory diseases affect the lungs and airways. Many are caused by infections, but others are related to environmental factors or genetic predispositions. Symptoms often include coughing, shortness of breath, and wheezing.
- Asthma: A chronic respiratory condition characterized by inflammation and narrowing of the airways.
- Chronic Obstructive Pulmonary Disease (COPD): A group of lung diseases including emphysema and chronic bronchitis.
- Bronchitis: Inflammation of the bronchial tubes.
Cancers
Cancer is a disease in which cells grow out of control and can invade other parts of the body. Risk factors vary depending on the type of cancer, but can include genetics, lifestyle factors, and environmental exposures. Early detection and treatment are crucial.
- Breast Cancer: Cancer that starts in the breast tissue.
- Lung Cancer: Cancer that starts in the lungs.
- Colorectal Cancer: Cancer that starts in the colon or rectum.
Other Common Diseases
This category includes a range of diseases that don't neatly fit into the previous categories. These conditions can have diverse causes and treatments.
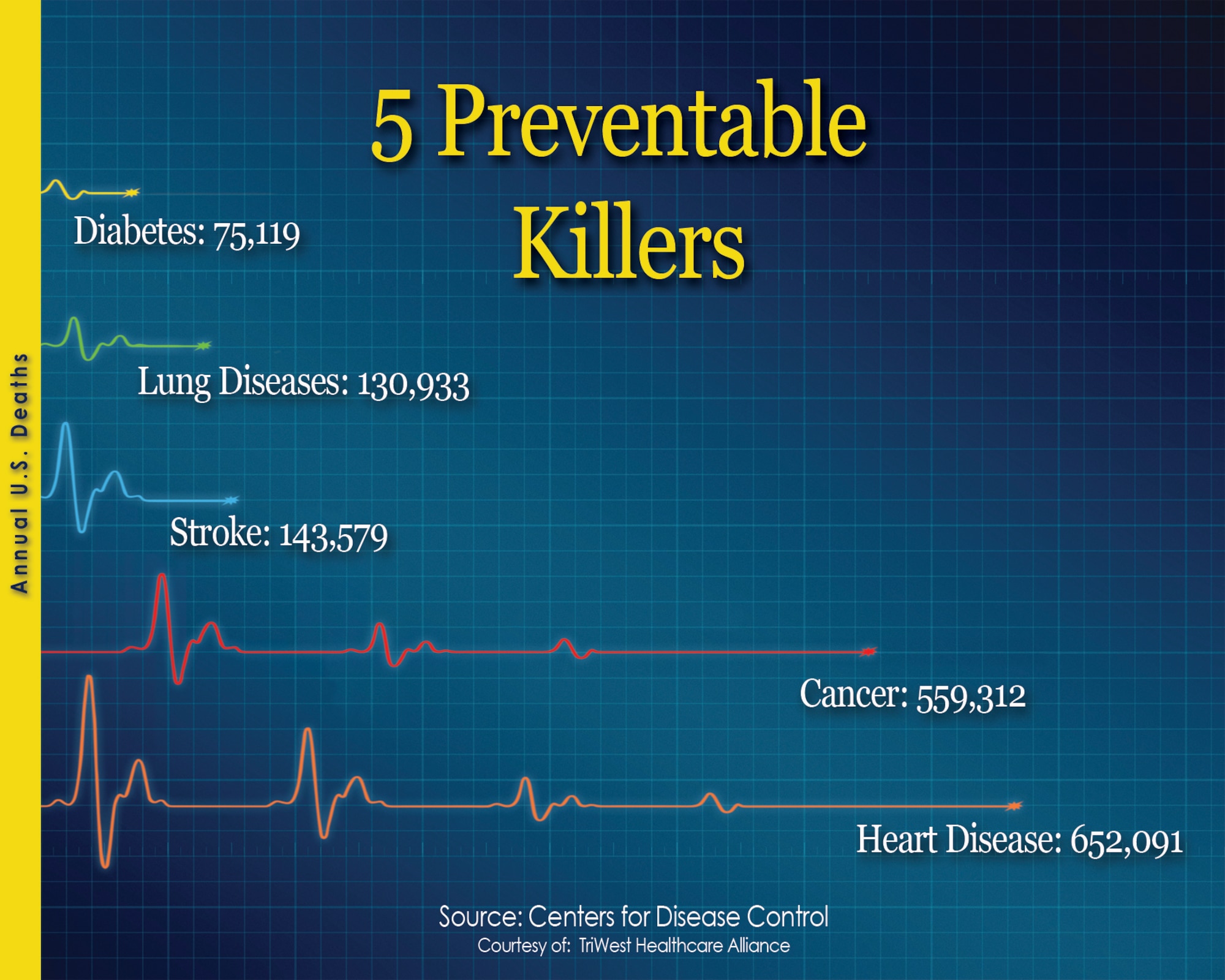
- Diabetes: A metabolic disorder characterized by high blood sugar levels.
- Alzheimer's Disease: A progressive neurodegenerative disease affecting memory and cognitive function.
- Osteoporosis: A disease characterized by low bone density, increasing the risk of fractures.
- Kidney Disease: Damage to the kidneys' ability to filter waste from the blood.
- Depression: A mood disorder characterized by persistent sadness and loss of interest.
- Arthritis: Inflammation of one or more joints.
What is the hardest chronic illness to live with?

There is no single answer to the question of what is the hardest chronic illness to live with. The experience of living with a chronic illness is profoundly personal and subjective. Its impact is shaped by a multitude of factors including the specific illness, its severity, the individual's personality, support system, access to resources, and coping mechanisms. What might be incredibly challenging for one person might be more manageable for another. Factors such as pain levels, functional limitations, emotional toll, and the unpredictable nature of some illnesses all contribute to the overall burden.
What Makes a Chronic Illness "Hard"?
The difficulty of living with a chronic illness isn't simply about the physical symptoms. It's a complex interplay of many factors. Pain management is often a significant struggle, but so is the emotional burden of living with an unpredictable condition. The impact on daily life, relationships, and financial stability can be overwhelming. The feeling of loss of control and the constant need to adapt to changing circumstances contribute greatly to the difficulty.
- Physical Limitations and Pain
- Emotional Toll and Mental Health Impacts
- Social Isolation and Relationship Challenges
Impact on Daily Life and Independence
Many chronic illnesses significantly impact daily life. Simple tasks that most people take for granted, such as bathing, dressing, or even walking, can become incredibly challenging. The need for constant medical care, medication adherence, and frequent doctor's appointments disrupt routines and limit spontaneity. This can lead to a significant loss of independence, affecting both personal and professional life. The unpredictability of symptoms can also make planning challenging and lead to feelings of anxiety and uncertainty.
- Difficulty Performing Activities of Daily Living (ADLs)
- Impact on Employment and Career
- Challenges with Social Participation and Leisure Activities
Financial Burden and Access to Healthcare
Chronic illnesses often come with substantial financial burdens. Medical expenses, including medications, therapies, and hospitalizations, can be exorbitant. Lost wages due to disability or reduced work capacity further exacerbate financial strain. Access to quality healthcare is crucial but not always guaranteed, and navigating the healthcare system can be a complex and frustrating process, adding to the stress and burden of living with a chronic illness.
- High Medical Costs and Insurance Challenges
- Lost Income and Financial Instability
- Difficulty Accessing Specialized Care and Treatment
The Emotional and Psychological Impact
Beyond the physical challenges, chronic illnesses take a significant toll on mental health. The constant struggle with pain, fatigue, and uncertainty can lead to anxiety, depression, and feelings of isolation. The unpredictability of symptoms and the fear of future health complications can create significant stress and impact emotional well-being. Maintaining a positive outlook and managing mental health is a vital aspect of living with a chronic illness.
- Increased Risk of Depression and Anxiety
- Challenges with Self-Esteem and Body Image
- Difficulty Maintaining Healthy Relationships
The Role of Support Systems and Coping Mechanisms
The experience of living with a chronic illness is profoundly influenced by the availability of support. A strong support network, including family, friends, and healthcare providers, can be instrumental in navigating the challenges and maintaining a good quality of life. Developing effective coping mechanisms, such as stress management techniques, mindfulness, and engaging in activities that bring joy, is also crucial. Accessing appropriate psychological support and therapy can provide valuable tools for managing emotional distress and improving overall well-being.
- Importance of Social Support and Community
- Effective Coping Strategies and Stress Management
- Access to Mental Health Services and Therapy
What are the top 10 fatal diseases?

What are the Top 10 Fatal Diseases?
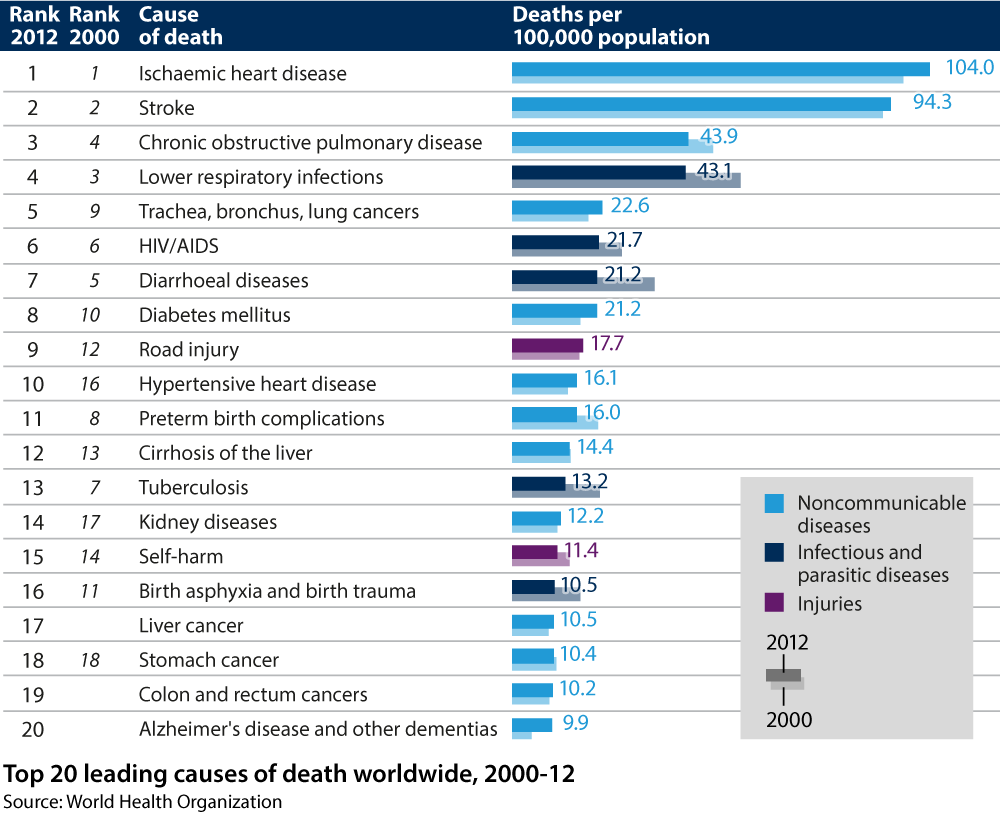
Defining the "top 10" fatal diseases is complex and depends heavily on factors like year, region, and how mortality is measured (e.g., cause of death vs. underlying cause). Global mortality data varies slightly between organizations like the World Health Organization (WHO) and others. However, consistently appearing among the leading causes of death worldwide are a group of infectious and non-communicable diseases. Precise ranking shifts annually, but the following diseases consistently contribute to a significant number of deaths globally.
Ischemic Heart Disease
Ischemic heart disease, encompassing conditions like coronary artery disease, is a leading cause of death worldwide. It occurs when the blood supply to the heart muscle is reduced, often due to atherosclerosis (plaque buildup in arteries). This leads to chest pain (angina), heart attacks (myocardial infarction), and ultimately, death if untreated. Prevention focuses on managing risk factors such as high blood pressure, high cholesterol, smoking, and diabetes.
- Risk Factors: High blood pressure, high cholesterol, smoking, diabetes, obesity, family history.
- Symptoms: Chest pain, shortness of breath, fatigue, sweating.
- Treatment: Lifestyle changes, medications (statins, blood pressure medications), angioplasty, bypass surgery.
Stroke
Stroke occurs when blood supply to part of the brain is interrupted, leading to brain cell damage. This can result in permanent disability or death. There are two main types: ischemic stroke (blocked artery) and hemorrhagic stroke (bleeding in the brain). Quick medical attention is crucial for optimal outcomes.
- Risk Factors: High blood pressure, atrial fibrillation, diabetes, smoking, high cholesterol, family history.
- Symptoms: Sudden weakness or numbness in the face, arm, or leg, confusion, trouble speaking, vision problems, severe headache.
- Treatment: Medications (blood thinners, clot-busters), surgery, rehabilitation.
Chronic Obstructive Pulmonary Disease (COPD)
COPD encompasses conditions like emphysema and chronic bronchitis, characterized by airflow limitation in the lungs. Smoking is the primary risk factor, leading to progressive lung damage and difficulty breathing. COPD often leads to respiratory failure and death.
- Risk Factors: Smoking, air pollution, genetic factors.
- Symptoms: Shortness of breath, chronic cough, wheezing, excess mucus production.
- Treatment: Medications (bronchodilators, inhalers), pulmonary rehabilitation, oxygen therapy.
Lower Respiratory Infections
Lower respiratory infections like pneumonia and bronchitis affect the lungs and airways, often caused by bacteria, viruses, or fungi. These infections can be particularly dangerous for young children, the elderly, and those with weakened immune systems. Pneumonia, in particular, is a major cause of death globally, especially in developing countries.
- Risk Factors: Weakened immune system, age, underlying lung conditions.
- Symptoms: Cough, fever, shortness of breath, chest pain.
- Treatment: Antibiotics (for bacterial infections), antiviral medications (for viral infections), supportive care.
Alzheimer's Disease
Alzheimer's disease is a progressive neurodegenerative disorder that causes memory loss, cognitive decline, and eventually, death. It's the most common cause of dementia worldwide, and there is currently no cure. Research continues to focus on developing effective treatments and prevention strategies.
- Risk Factors: Age, family history, genetics.
- Symptoms: Memory loss, confusion, difficulty with language and problem-solving, changes in personality and behavior.
- Treatment: Medications to slow progression, supportive care, assistance with daily living.
What is top 5 disease?
What is the Top 5 Disease?
Defining the "top 5" diseases is challenging because rankings vary depending on factors like mortality rate, morbidity (prevalence of illness), disability-adjusted life years (DALYs), and geographic location. However, based on global burden of disease studies, consistently appearing near the top are diseases impacting a significant portion of the global population and causing substantial mortality and morbidity. It's crucial to understand that these rankings are dynamic and subject to change based on ongoing research, advancements in healthcare, and evolving epidemiological patterns.
1. Ischemic Heart Disease
Ischemic heart disease (IHD), commonly known as coronary artery disease (CAD), is a condition where the blood flow to the heart is reduced, frequently due to atherosclerosis (the buildup of plaque in the arteries). This reduction in blood flow can lead to angina (chest pain), myocardial infarction (heart attack), and heart failure. It's a leading cause of death globally, particularly in high-income countries.
- Risk factors: High blood pressure, high cholesterol, smoking, diabetes, obesity, and family history.
- Symptoms: Chest pain or pressure, shortness of breath, sweating, nausea.
- Treatment: Lifestyle changes, medication (e.g., statins, beta-blockers), angioplasty, bypass surgery.
2. Stroke
A stroke occurs when the blood supply to part of the brain is interrupted, leading to brain cell death. This can result in a wide range of impairments, depending on the area of the brain affected. Strokes can be caused by a blood clot blocking an artery (ischemic stroke) or by bleeding in the brain (hemorrhagic stroke). Rapid medical attention is crucial for stroke treatment.
- Risk factors: High blood pressure, high cholesterol, smoking, atrial fibrillation, diabetes.
- Symptoms: Sudden weakness or numbness in the face, arm, or leg, confusion, difficulty speaking, vision problems.
- Treatment: Medications to dissolve blood clots (tPA), surgery, rehabilitation.
3. Chronic Obstructive Pulmonary Disease (COPD)
COPD encompasses lung diseases characterized by airflow limitation that's not fully reversible. The most common forms are chronic bronchitis (inflammation of the airways) and emphysema (damage to the air sacs in the lungs). COPD is largely preventable and associated with long-term exposure to noxious particles or gases, most notably cigarette smoke.
- Risk factors: Smoking (primary risk factor), air pollution, genetics.
- Symptoms: Shortness of breath, chronic cough, wheezing, increased mucus production.
- Treatment: Medications (e.g., bronchodilators, corticosteroids), oxygen therapy, pulmonary rehabilitation.
4. Lower Respiratory Infections
Lower respiratory infections (LRIs) affect the lower respiratory tract, including the bronchi and lungs. These infections can range from relatively mild conditions like bronchitis to severe ones like pneumonia. Pneumonia, in particular, can be life-threatening, especially among vulnerable populations like the elderly and young children.
- Causes: Viruses (e.g., influenza, RSV), bacteria (e.g., Streptococcus pneumoniae), fungi.
- Symptoms: Cough, fever, shortness of breath, chest pain.
- Treatment: Antibiotics for bacterial infections, antiviral medications for viral infections, supportive care.
5. Lung Cancer
Lung cancer is a leading cause of cancer deaths worldwide. Most cases are linked to cigarette smoking, but other risk factors include exposure to radon, asbestos, and air pollution. Early detection and treatment are crucial for improving survival rates.
- Risk factors: Smoking, exposure to carcinogens, family history.
- Symptoms: Cough, shortness of breath, chest pain, weight loss.
- Treatment: Surgery, chemotherapy, radiation therapy, targeted therapy.
What criteria are used to determine the "top" 20 diseases?
Defining the "top" 20 diseases is inherently complex and depends heavily on the chosen criteria. There isn't a single universally accepted ranking. Different organizations and studies employ various metrics, leading to varied results. Some common criteria include: global mortality rates (number of deaths attributed to a disease), years of life lost (YLL) due to premature death, disability-adjusted life years (DALYs) which combine mortality and morbidity (years lived with disability), incidence (number of new cases), prevalence (total number of existing cases), and economic burden (healthcare costs and lost productivity). The weight given to each criterion significantly impacts the final ranking. For instance, a disease with high prevalence but low mortality might rank differently than one with lower prevalence but high mortality. Furthermore, data availability and reliability vary across different regions and diseases, introducing further complexities and potential biases into any ranking. Therefore, any list of "top" 20 diseases should be interpreted within the context of the specific criteria used and the limitations of the data.
How often are these rankings updated, and why?
Rankings of the top diseases are not static; they are subject to change and are often updated periodically, usually annually or every few years. Several factors necessitate these updates. First, disease prevalence and mortality rates fluctuate due to various factors, such as improvements in sanitation, vaccination campaigns, the emergence of new diseases (e.g., pandemics), antibiotic resistance, changes in lifestyle and environmental conditions, and advancements in medical treatment. Second, data collection methods and the availability of reliable data improve over time. Better epidemiological surveillance systems and improved diagnostic techniques can lead to more accurate estimates of disease burden. Third, the understanding of disease etiology and pathogenesis evolves, leading to changes in how diseases are classified and counted. For instance, advancements in genetic research may reclassify certain diseases, impacting their prevalence estimates. Therefore, regular updates are crucial to reflect the current state of global health and to inform resource allocation and public health policies effectively.
Do these rankings consider diseases affecting specific populations or regions more than others?
The focus on global rankings often overshadows the disproportionate impact certain diseases have on specific populations or geographical regions. While some rankings attempt to account for regional variations, many primarily focus on global aggregate data, potentially masking significant disparities. For example, certain neglected tropical diseases may have a devastating impact on specific communities in developing countries but may have a relatively low global ranking due to their limited global prevalence. Similarly, diseases with high mortality in specific age groups (e.g., infant mortality) might not be fully captured by metrics focusing solely on overall mortality rates. Therefore, while global rankings offer a useful overview, it's crucial to supplement them with region-specific data and analyses to address the unique health challenges faced by diverse populations. Focusing solely on global top 20 lists risks neglecting significant public health issues affecting vulnerable communities.
What are the limitations of such "top 20" lists, and how should they be interpreted?
While "top 20" disease lists provide a helpful snapshot of global health challenges, it's essential to acknowledge their inherent limitations. Firstly, they are simplifications of a complex reality. Reducing the vast spectrum of human disease to a ranked list inevitably overlooks nuances and the interplay between various diseases and risk factors. Secondly, the selection of criteria and the data used significantly influence the results, as discussed previously. Thirdly, data quality and availability vary greatly across different regions and diseases, leading to potential biases and inaccuracies in the rankings. Finally, such lists should not be interpreted as implying that diseases outside the top 20 are unimportant. Many lesser-known diseases can have severe consequences for individuals and communities. Therefore, "top 20" lists are best viewed as a starting point for understanding global health priorities, rather than a definitive or exhaustive account of all significant health challenges. They should be used in conjunction with more detailed analyses of specific diseases and regions to inform comprehensive public health strategies.
Deja una respuesta