What is the deadliest bacteria in history

Throughout the annals of human history, the relentless battle against bacterial foes has left an indelible scar upon humanity. From the bubonic plague that decimated medieval Europe to the horrors of cholera and tuberculosis, these microscopic adversaries have wreaked havoc, claiming countless lives and leaving an enduring legacy of fear and devastation. Among this deadly pantheon, one bacterium stands apart as the undisputed champion of lethality—a microscopic killer that has left an unfathomable trail of suffering in its wake.
What is the Deadliest Bacteria in History? A Difficult Question to Answer
Determining the single "deadliest" bacteria in history is incredibly challenging. Death tolls are difficult to accurately track throughout history, especially for diseases that predate reliable record-keeping. Many bacterial infections are also often intertwined with other factors, making isolating the bacterial impact difficult. However, several bacteria have been responsible for immense suffering and loss of life throughout human history. We can look at those with the highest death tolls, or those with the highest mortality rates, to gain some insight.
The Plague (Yersinia pestis)
Yersinia pestis, the bacteria responsible for bubonic plague (also known as the Black Death), is a strong contender for the deadliest. The Black Death ravaged Eurasia and North Africa in the mid-14th century, wiping out an estimated 30-60% of Europe's population. Its high mortality rate and rapid spread made it devastatingly lethal. The bacterium is transmitted primarily through flea bites, and the pneumonic form can spread through respiratory droplets, leading to fast-spreading outbreaks. Modern antibiotics are effective in treating the plague, but without them, the fatality rate is incredibly high.
Tuberculosis (Mycobacterium tuberculosis)
Tuberculosis, caused by Mycobacterium tuberculosis, is another leading candidate. It has been a scourge of humanity for millennia, causing significant mortality throughout history. While not as immediately lethal as the plague in some outbreaks, its chronic nature and high prevalence mean it has cumulatively caused a vast number of deaths. TB infects the lungs, but can spread to other parts of the body. Drug-resistant strains pose a significant ongoing threat, highlighting the continuing danger of this bacterium.
Pneumonia (Various Bacteria)
Pneumonia, an infection of the lungs, can be caused by several bacteria, most notably Streptococcus pneumoniae. While not a single bacterium, the various bacterial causes of pneumonia have contributed to an enormous number of deaths throughout history. Pneumonia is particularly dangerous for vulnerable populations such as infants, the elderly, and those with weakened immune systems. Access to effective antibiotics is crucial in reducing pneumonia mortality.
Cholera (Vibrio cholerae)
Vibrio cholerae, the bacterium responsible for cholera, causes severe diarrhea and dehydration, leading to rapid death if left untreated. Cholera has historically caused devastating outbreaks, particularly in regions with poor sanitation and access to clean water. While treatment with rehydration therapy is effective, lack of access to clean water and medical care remain major challenges in controlling cholera outbreaks.
Typhoid Fever (Salmonella Typhi)
Salmonella Typhi, the cause of typhoid fever, is another bacterium with a significant historical death toll. Typhoid fever causes high fever, severe headache, stomach pain, and other symptoms. It is spread through contaminated food and water, making it a particular problem in areas with poor sanitation. Improved sanitation and hygiene practices are crucial in preventing typhoid fever outbreaks. While treatable with antibiotics, access to treatment is critical.
| Bacteria | Disease | Notable Feature |
|---|---|---|
| Yersinia pestis | Bubonic Plague | High mortality rate, rapid spread |
| Mycobacterium tuberculosis | Tuberculosis | Chronic infection, drug-resistant strains |
| Streptococcus pneumoniae (and others) | Pneumonia | High mortality in vulnerable populations |
| Vibrio cholerae | Cholera | Severe dehydration, requires rapid treatment |
| Salmonella Typhi | Typhoid Fever | Spread through contaminated food and water |
What is the most deadly bacteria in the world?
There is no single "most deadly" bacteria in the world. The lethality of a bacteria depends on a multitude of factors, including the virulence of the specific strain, the health of the infected individual, the availability of treatment, and the speed of diagnosis. However, several bacteria are consistently associated with high mortality rates and pose significant global health threats. Clostridium botulinum, for example, produces one of the most potent toxins known, but its impact is often limited by the relatively infrequent exposure. Similarly, Yersinia pestis (the cause of plague) can be highly deadly if left untreated, but effective antibiotics exist. Ultimately, the relative deadliness is contextual and dependent on many variables.
Defining "Most Deadly"
Defining the "most deadly" bacteria is challenging because mortality rates vary widely based on numerous factors. These factors include the virulence of the specific strain, the host's immune system strength, access to medical care (including prompt diagnosis and appropriate antibiotics), and pre-existing health conditions. A bacteria with high virulence might not be the deadliest if readily treatable, while a less virulent bacteria could cause high mortality in a vulnerable population lacking access to healthcare.
- Virulence: The ability of a bacterium to cause disease.
- Host Factors: The individual's immune system, age, and other health conditions.
- Environmental Factors: Access to clean water, sanitation, and medical care.
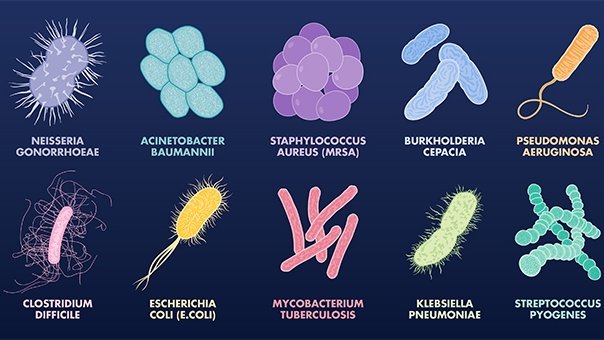
High Mortality Rate Bacteria: Clostridium difficile
Clostridium difficile (C. diff) is a bacterium responsible for significant hospital-acquired infections. While not always fatal, C. diff infections can lead to severe diarrhea, colitis, and even toxic megacolon, a life-threatening complication. The mortality rate of C. diff infections is influenced by factors such as age, underlying health conditions, and the severity of the infection. Antibiotic resistance also poses a considerable challenge in treating C. diff infections, contributing to higher mortality rates in certain populations.
- Antibiotic Resistance: Makes treatment more challenging.
- Severe Complications: Can lead to life-threatening conditions like toxic megacolon.
- High Prevalence in Hospitals: Makes it a significant concern for healthcare settings.
High Mortality Rate Bacteria: Streptococcus pneumoniae
Streptococcus pneumoniae is a common bacterium that can cause a range of infections, from mild respiratory illnesses to severe pneumonia, meningitis, and sepsis. While many infections are manageable with antibiotics, some strains of Streptococcus pneumoniae are increasingly resistant to these treatments. Mortality rates are particularly high in vulnerable populations, such as young children, the elderly, and individuals with weakened immune systems. Rapid diagnosis and appropriate antibiotic therapy are crucial in reducing mortality.
- Antibiotic Resistance: Limits treatment options and increases mortality risk.
- Vulnerable Populations: The elderly and immunocompromised are at higher risk of severe illness and death.
- Variety of Infections: Causes illnesses ranging from mild to life-threatening.
High Mortality Rate Bacteria: Staphylococcus aureus (MRSA)
Methicillin-resistant Staphylococcus aureus (MRSA) is a type of staph bacteria resistant to many common antibiotics. MRSA infections can range from skin infections to life-threatening bloodstream infections, pneumonia, and sepsis. The mortality rate of MRSA infections is significantly higher compared to non-resistant staph infections due to limited treatment options. Prompt diagnosis and the use of appropriate antibiotics (if available) are crucial factors in reducing mortality from MRSA.
- Antibiotic Resistance: A major factor in higher mortality rates.
- Severe Infections: Can lead to life-threatening bloodstream infections and pneumonia.
- Healthcare-Associated Infections: Common in hospitals and other healthcare settings.
Factors Influencing Bacterial Lethality
The lethality of a bacterium is complex and depends on several interrelated factors beyond the inherent virulence of the bacteria. These factors include the route of infection (inhalation, ingestion, wound), the dose of the bacteria, the individual's immune status, and access to and quality of medical care. For example, a highly virulent bacteria introduced through a small wound might cause a localized infection, while the same bacteria inhaled in large quantities could lead to a systemic and potentially fatal infection.
- Route of Infection: The way the bacteria enters the body.
- Infectious Dose: The amount of bacteria needed to cause infection.
- Immune Status: The strength of the host's immune response.
- Healthcare Access: Availability and quality of medical treatment.
Which bacteria has killed the most humans?

Which Bacteria Has Killed the Most Humans?
Pinpointing the single bacteria responsible for the most human deaths throughout history is incredibly difficult due to limitations in historical record-keeping, particularly for pre-modern eras. Many infectious diseases caused by various bacteria have ravaged populations for centuries, making direct comparison challenging. However, strong candidates include bacteria responsible for diseases like tuberculosis, pneumonia, and diarrheal diseases. The precise number of deaths attributed to any one bacterium is impossible to definitively determine. Accurate global mortality data, especially from earlier centuries, is often lacking or unreliable. The impact of a given bacteria is also highly dependent on factors like sanitation, healthcare access, and population density.
Estimating Historical Mortality: The Challenges
Accurately estimating historical mortality due to bacterial infections presents significant hurdles. Early records often lacked the diagnostic sophistication to differentiate between bacterial infections, and many deaths were simply attributed to vague causes like “fever” or “consumption.” This makes it nearly impossible to definitively isolate the role of specific bacteria. Furthermore, variations in reporting practices across different regions and time periods complicate efforts to build comprehensive datasets. The lack of standardized methods for disease identification and record-keeping throughout history presents a major obstacle to definitive answers.
- Incomplete historical data: Accurate records of infectious disease deaths, particularly from earlier centuries, are often missing or incomplete.
- Diagnostic limitations: Early medical understanding lacked the technology to precisely identify the causative bacteria in many instances.
- Confounding factors: Many deaths resulted from co-infections, making it difficult to attribute mortality solely to a specific bacterium.
Mycobacterium tuberculosis and Tuberculosis
Tuberculosis (TB), caused by Mycobacterium tuberculosis, is a strong contender for the bacterium that has killed the most humans. TB has been a significant human pathogen for millennia, with evidence suggesting its presence in ancient human remains. Its high transmissibility and the often-fatal nature of the disease, particularly before the advent of effective antibiotics, make it a leading candidate. While precise numbers remain elusive, the historical impact of TB is undeniably vast.
- High transmissibility: TB spreads easily through the air, increasing its potential for widespread infection.
- High mortality rate: Before effective treatment, TB often proved fatal.
- Long history: Evidence suggests TB has infected humans for thousands of years.
Diarrheal Diseases: A Leading Cause of Death
Diarrheal diseases, caused by a range of bacteria (such as Vibrio cholerae, Salmonella species, Shigella species, and Escherichia coli), represent another major category of bacterial infections responsible for countless deaths throughout history. These illnesses are particularly devastating in regions with poor sanitation and limited access to clean water. The sheer number of deaths caused by these infections, particularly among children, makes it difficult to exclude them from the discussion of the deadliest bacteria.
- High prevalence in developing countries: Poor sanitation and hygiene contribute to high rates of diarrheal diseases in many parts of the world.
- High mortality in children: Dehydration resulting from diarrheal diseases is a leading cause of death in young children.
- Multiple bacterial pathogens: Various bacteria contribute to diarrheal illness, making precise attribution challenging.
Pneumonia: A Frequent Killer
Pneumonia, frequently caused by bacteria like Streptococcus pneumoniae and Haemophilus influenzae, remains a significant cause of death worldwide, particularly among vulnerable populations. While the specific number of deaths attributable to bacterial pneumonia throughout history is unknown, it has undoubtedly contributed to a substantial portion of human mortality. Its impact is amplified in regions lacking adequate healthcare access.
- High mortality in vulnerable groups: The elderly, infants, and individuals with weakened immune systems are particularly susceptible to fatal pneumonia.
- Multiple bacterial causes: Several bacterial species can cause pneumonia, making precise attribution difficult.
- Widespread impact: Pneumonia has been a significant cause of death across diverse populations and geographical areas.
What are the worst bacteria diseases in history?

The Plague (Yersinia pestis)
The Plague, also known as the Black Death, is arguably the most devastating bacterial disease in human history. Caused by the bacterium Yersinia pestis, it swept across Eurasia and North Africa in multiple waves, most notably during the mid-14th century. The disease's high mortality rate and rapid spread led to a catastrophic loss of life, significantly altering the course of history and leaving a lasting impact on society. Its impact extended beyond immediate deaths, causing widespread social upheaval, economic collapse, and profound psychological trauma.
- High mortality rate: Estimates suggest that the Black Death killed 30-60% of Europe's population.
- Multiple forms: The plague exists in bubonic, septicemic, and pneumonic forms, each with varying levels of severity and transmission routes.
- Long-lasting societal impact: The plague's devastation resulted in labor shortages, religious fervor, and significant changes in social structures.
Tuberculosis (Mycobacterium tuberculosis)
Tuberculosis (TB), caused by Mycobacterium tuberculosis, remains a significant global health problem. Though its impact is less dramatic in a single event compared to the Plague, its persistent presence and chronic nature have resulted in an immense cumulative death toll throughout history. TB's ability to lie dormant within the body and reactivate later makes it particularly challenging to control. It disproportionately affects vulnerable populations, further compounding its impact.
- Chronic and persistent infection: TB can remain dormant for years before reactivating, making diagnosis and treatment difficult.
- Global health burden: Millions of people worldwide are infected with TB, resulting in a substantial number of deaths annually.
- Drug resistance: The emergence of drug-resistant strains of TB poses a major threat to global public health.
Typhoid Fever (Salmonella Typhi)
Typhoid fever, caused by Salmonella Typhi, has been a scourge throughout history, characterized by high fever, headache, and gastrointestinal distress. While outbreaks have been effectively controlled in many developed nations through sanitation and vaccination, it remains a significant concern in regions with inadequate sanitation and access to clean water. Its fecal-oral transmission route contributes to its persistence in areas with poor hygiene.
- Fecal-oral transmission: Contaminated food and water are the primary sources of typhoid fever infection.
- High fever and gastrointestinal symptoms: Typhoid fever's characteristic symptoms often lead to severe dehydration and complications.
- Continued prevalence in developing countries: Typhoid remains a public health threat in many parts of the world due to inadequate sanitation.
Cholera (Vibrio cholerae)
Cholera, caused by Vibrio cholerae, is a severe diarrheal illness that can be fatal if left untreated. Characterized by rapid dehydration, cholera has historically been associated with unsanitary conditions and outbreaks often follow natural disasters or periods of conflict. Although treatments exist, the disease remains a significant challenge in areas with limited access to healthcare and clean water.
- Severe dehydration: The profuse diarrhea caused by cholera can lead to rapid and potentially fatal dehydration.
- Waterborne transmission: Cholera spreads through contaminated water sources, making it particularly prevalent in areas with poor sanitation.
- Outbreaks following disasters: Disruptions to sanitation and water infrastructure often lead to cholera outbreaks.
Leprosy (Mycobacterium leprae)
Leprosy, caused by Mycobacterium leprae, is a chronic infectious disease primarily affecting the skin, peripheral nerves, mucosa of the upper respiratory tract, and the eyes. Historically, leprosy has been associated with significant stigma and social isolation, resulting in devastating consequences for individuals affected. Although treatable with multidrug therapy, the disease still persists in many parts of the world.
- Chronic and progressive disease: Leprosy can cause progressive damage to the skin, nerves, and other tissues if left untreated.
- Significant social stigma: The historical stigma associated with leprosy has led to social isolation and discrimination.
- Treatable but persistent: While effective treatment exists, leprosy remains a public health concern in several regions.
What is the king of all bacteria?
There is no single "king of all bacteria." The term implies a hierarchical structure and a single dominant species, which doesn't accurately reflect the vast diversity and complex relationships within the bacterial domain. Bacteria are incredibly diverse, occupying virtually every habitat on Earth and exhibiting a wide range of metabolic strategies and lifestyles. Instead of a single "king," there's a vast kingdom of bacteria with various dominant species in different environments. The concept of a "king" is an anthropomorphic projection onto a biological system that doesn't possess such a structure.
The Diversity of Bacterial Kingdoms
The bacterial world is incredibly diverse, encompassing a vast array of species with different shapes, sizes, metabolic capabilities, and ecological roles. They are not a unified group under a single ruler, but rather a vast collection of lineages with independent evolutionary histories. Attempting to crown a single species as the "king" ignores this fundamental aspect of bacterial biology. This diversity is reflected in their varied habitats, from the deep ocean to the human gut, and their diverse functions within ecosystems.
- Phylogenetic diversity: Bacteria represent multiple distinct lineages that diverged billions of years ago.
- Metabolic diversity: Bacteria utilize a vast array of metabolic pathways, ranging from photosynthesis to chemosynthesis.
- Ecological diversity: Bacteria occupy virtually every ecosystem on Earth, playing crucial roles in nutrient cycling, decomposition, and symbiotic relationships.
The Concept of Dominance in Bacterial Communities
While there is no "king," certain bacterial species can become dominant in specific environments under particular conditions. This dominance is often temporary and context-dependent, influenced by factors like nutrient availability, environmental stress, and interactions with other organisms. A species that thrives in one niche might be completely outcompeted in another. The idea of a single dominant species across all environments is simply not applicable to bacteria.
- Environmental factors: Temperature, pH, nutrient availability and oxygen levels strongly influence bacterial community composition.
- Competitive interactions: Bacteria compete for resources, produce antibiotics, and engage in other interactions that shape community structure.
- Symbiotic relationships: Many bacteria engage in symbiotic relationships with other organisms, which can affect their abundance and distribution.
Challenges in Defining a "King" in Bacteria
The very notion of a "king" implies a hierarchical structure with a single dominant entity at the apex. Bacterial communities are far more complex, often displaying a more intricate web of interactions among various species. There's rarely a clear-cut dominance hierarchy, and even when one species becomes abundant, it's usually due to specific environmental conditions rather than inherent superiority.
- Horizontal gene transfer: The frequent exchange of genetic material between bacterial species blurs lines of traditional evolutionary hierarchies.
- Complex community dynamics: Bacterial communities are characterized by intricate interactions, including cooperation, competition, and predation.
- Lack of a central authority: Unlike multicellular organisms with centralized control, bacteria operate as individual units or as loosely organized communities.
Examples of Ecologically Successful Bacteria
Instead of searching for a "king," it's more informative to study highly successful bacterial species that thrive in particular environments. These species have evolved strategies to compete effectively in their chosen niche, but their success is context-dependent. No single species reigns supreme across all environments.
- Escherichia coli: A common inhabitant of the human gut, exhibiting remarkable adaptability.
- Bacillus subtilis: A soil bacterium known for its resilience and ability to form spores.
- Cyanobacteria: Photosynthetic bacteria that play a critical role in global carbon cycling.
Misconceptions about Bacterial Dominance
The search for a "king" of bacteria stems from a misunderstanding of the nature of bacterial communities. These are not centrally organized systems with a single leader, but rather complex assemblages of interacting organisms. Attributing the concept of "kingship" to bacteria anthropomorphizes a biological system that operates under vastly different principles than human societies.
- Anthropomorphism: Projecting human societal structures onto bacteria leads to inaccurate and misleading interpretations.
- Oversimplification: Reducing the complexity of bacterial communities to a single dominant species ignores the intricate interactions and ecological roles of various species.
- Ignoring environmental context: The success of a bacterial species depends heavily on environmental factors and is not solely determined by inherent traits.
What is considered the deadliest bacteria in history and why?
Pinpointing the single “deadliest” bacteria in history is difficult due to several factors. First, accurate historical records of bacterial infections are inconsistent, particularly in pre-modern eras. Many deaths attributed to other causes might have actually stemmed from bacterial infections. Second, the lethality of a bacterium is dependent on numerous factors including the virulence of the specific strain, the host’s immune system, access to medical care, and environmental conditions. That being said, some bacteria have consistently caused widespread devastation and high mortality rates throughout history. Yersinia pestis, the bacterium responsible for the plague, is a strong contender for this title. Its ability to spread rapidly through flea bites and cause devastating pneumonic, bubonic, and septicemic forms of the disease led to millions of deaths across multiple pandemics. Other contenders include Vibrio cholerae, responsible for cholera outbreaks causing severe dehydration and death, and Mycobacterium tuberculosis, causing tuberculosis, which remains a significant global health threat with a high mortality rate, especially in immunocompromised individuals. It's important to remember that the "deadliest" is a relative term and depends heavily on the context and time period in question.
How many people have died from the deadliest bacteria?
Precise figures on the total number of deaths caused by any single bacterium throughout history are impossible to obtain. Historical records, especially for earlier pandemics, are frequently incomplete and unreliable. For example, while the Black Death (caused by Yersinia pestis) is estimated to have killed 30-60% of Europe's population in the 14th century, the exact numbers are speculative. Similarly, estimating the cumulative death toll from tuberculosis (caused by Mycobacterium tuberculosis) across millennia is extraordinarily challenging, given the disease’s long history and varying prevalence across different populations. Cholera (caused by Vibrio cholerae) has caused numerous devastating outbreaks throughout history, each claiming thousands to millions of lives depending on the scale and location of the outbreak. Therefore, providing a definitive answer to how many people have died from the "deadliest" bacteria is unfortunately impossible with current data. The vast, and often unknown, number of deaths highlights the impact these bacteria have had on human civilization.
Are there any new deadliest bacteria emerging?
The emergence of antibiotic-resistant bacteria poses a significant threat, potentially creating new “deadliest” bacteria in the future. Bacteria constantly evolve, and the overuse and misuse of antibiotics are driving the selection and spread of strains resistant to multiple drugs. This means infections that were once easily treatable can become life-threatening. For example, the rise of carbapenem-resistant Enterobacteriaceae (CRE) is a serious concern, as these bacteria are resistant to many last-resort antibiotics. Similarly, the increasing prevalence of antibiotic resistance in Staphylococcus aureus (MRSA) and other common pathogens makes them significantly more dangerous. While these bacteria may not be inherently “new” species, their acquired antibiotic resistance transforms them into much more lethal threats, requiring innovative approaches to treatment and prevention. Monitoring the emergence and spread of antibiotic-resistant bacteria is crucial for public health and preventing future pandemics.
What are the current efforts to combat the deadliest bacteria?
Combating the deadliest bacteria involves a multi-pronged approach focusing on prevention, treatment, and research. Vaccination programs are crucial for preventing many bacterial infections, such as those caused by Haemophilus influenzae type b (Hib) and Streptococcus pneumoniae. Improved sanitation and hygiene practices play a significant role in reducing the spread of bacteria, especially in regions with limited access to clean water and sanitation. Development and deployment of new antibiotics are vital for treating bacterial infections, although the increasing prevalence of antibiotic resistance is a major challenge. Researchers are actively exploring alternative strategies, including the development of new antibiotics, bacteriophages (viruses that infect bacteria), and innovative therapies targeting bacterial virulence factors. Public health surveillance is essential for monitoring the spread of bacterial infections, identifying outbreaks, and implementing timely interventions. Finally, education about antibiotic stewardship and hygiene practices is crucial for promoting responsible antibiotic use and preventing the spread of resistant bacteria.
Deja una respuesta