What disease is the biggest killer of all time
In the annals of medical history, one disease stands tall as the greatest annihilator of human life. Its shadow has cast a pall over civilizations, claimed countless souls, and shaped the course of history. The name of this ruthless killer, responsible for more deaths than any other, is smallpox.
What Disease Holds the Grim Title of History's Deadliest?
Determining the single biggest killer of all time is a complex task, fraught with challenges in accurately recording historical data. Different eras had varying methods of disease classification and record-keeping, leading to inconsistencies. However, considering the sheer scale of its impact across millennia, infectious diseases, in general, claim the unfortunate title. No single disease consistently reigns supreme throughout history; rather, different infectious diseases have dominated at various points, causing devastating pandemics that wiped out significant portions of the global population.
The Plague's Devastating Reign
The Black Death (bubonic plague), caused by the bacterium Yersinia pestis, stands as a prime contender for history's deadliest disease. Sweeping across Eurasia and North Africa in the mid-14th century, it's estimated to have killed 30-60% of Europe's population. The plague’s impact wasn't limited to a single event; it recurred in waves throughout history, continuously claiming lives and shaping societies. Its method of transmission (fleas on rodents) made containment extremely difficult.
Smallpox: A Scourge Eradicated
Smallpox, caused by the variola virus, was another horrific killer responsible for an estimated 300-500 million deaths in the 20th century alone. Highly contagious and leaving survivors with characteristic scarring, it ravaged populations globally for millennia. The successful eradication of smallpox in 1980 stands as a testament to the power of global vaccination efforts, making it a significant turning point in combating infectious diseases.
Tuberculosis: A Persistent Threat
Tuberculosis (TB), caused by the bacterium Mycobacterium tuberculosis, remains a significant global health concern. While not as acutely lethal as some other infectious diseases on this list, its persistent presence throughout history and its high mortality rate, especially among vulnerable populations, have resulted in a staggering death toll estimated in the billions over centuries. Its airborne transmission makes containment challenging.
Influenza Pandemics: Waves of Death
Several influenza pandemics, particularly the 1918 Spanish flu, have caused immense devastation. The 1918 pandemic is estimated to have killed 50-100 million people worldwide in a remarkably short time. The virus’s rapid spread and high mortality rate, particularly among young adults, made it exceptionally deadly. The potential for future influenza pandemics remains a major public health concern.
Malaria: A Persistent Killer in Tropical Regions
Malaria, caused by parasites of the genus Plasmodium and transmitted by mosquitoes, continues to claim hundreds of thousands of lives annually, primarily in sub-Saharan Africa. While exact historical figures are difficult to obtain, its long-standing presence and persistent impact on human populations throughout history place it among the deadliest diseases. Its continuous evolution and development of resistance to antimalarial drugs present ongoing challenges to global health efforts.
| Disease | Estimated Deaths | Significant Characteristics |
|---|---|---|
| Bubonic Plague | 30-60% of Europe's population (14th century) | Rodent-borne, highly contagious |
| Smallpox | 300-500 million (20th century) | Highly contagious, eradicated in 1980 |
| Tuberculosis | Billions (throughout history) | Airborne transmission, persistent threat |
| 1918 Influenza | 50-100 million (1918-1919) | Rapid spread, high mortality rate |
| Malaria | Hundreds of thousands annually | Mosquito-borne, persistent in tropical regions |
What is the biggest killer disease in history?
Pinpointing the single biggest killer disease in history is incredibly difficult due to limitations in historical record-keeping, particularly for ancient times. Different methodologies for tracking deaths (e.g., cause of death vs. symptoms) and inconsistent data across different populations and eras further complicate the task. However, strong candidates for the title include the plague (bubonic plague) and various forms of infectious diseases that caused widespread mortality throughout history. The impact of these diseases is amplified by factors like population density, sanitation levels, and access to medical care, which varied significantly across different times and places. Therefore, claiming a single disease as the absolute "biggest killer" is an oversimplification.
Estimating Mortality Rates for Historical Diseases
Accurately estimating the death toll from historical plagues and pandemics is a challenge. While certain events like the Black Death left relatively well-documented (though still incomplete) records, many earlier epidemics have far less comprehensive information. The available data often focuses on specific regions or populations, making extrapolation to global figures extremely unreliable. Historians and epidemiologists employ various methodologies, including analyzing historical documents, demographic data, and archaeological evidence, but considerable uncertainty remains in estimations.
- Challenges in Data Collection: Lack of standardized record-keeping across diverse cultures and time periods makes comparisons difficult.
- Indirect Evidence: Historians must often rely on indirect evidence such as burial records, descriptions of symptoms in historical texts, and analysis of skeletal remains.
- Modeling and Estimation: Statistical modeling techniques are used to extrapolate from incomplete data, but these models inherently contain uncertainties.
The Black Death's Impact
The Black Death, a pandemic caused by the bacterium Yersinia pestis, is widely considered one of the most devastating pandemics in history. Sweeping across Europe and Asia in the mid-14th century, it is estimated to have killed 30-60% of Europe's population. The disease spread rapidly, largely due to unsanitary conditions and the lack of understanding of disease transmission. Its impact extended far beyond the immediate death toll, causing significant societal, economic, and religious upheaval.
- Massive Population Decline: The Black Death resulted in a drastic reduction in the population across affected regions.
- Social and Economic Disruption: The pandemic led to labor shortages, social unrest, and significant changes in economic structures.
- Religious and Philosophical Impacts: The widespread death and suffering caused by the plague led to significant changes in religious beliefs and philosophical thought.
Other Major Infectious Disease Killers
Beyond the Black Death, numerous other infectious diseases have caused catastrophic mortality throughout history. Smallpox, for example, devastated populations globally for centuries before the development of a vaccine. Influenza pandemics, including the 1918 Spanish flu, caused millions of deaths. Tuberculosis (TB) remains a significant global health challenge, although its prevalence has been reduced in many parts of the world.
- Smallpox: A highly contagious disease that has been eradicated through global vaccination efforts.
- Influenza: Recurring pandemics have caused significant mortality throughout history, with the 1918 Spanish flu being particularly deadly.
- Tuberculosis: A bacterial infection that continues to pose a significant public health threat in many regions.
Factors Influencing Disease Mortality
The severity of a disease's impact isn't solely determined by its virulence (ability to cause disease). Several factors influence its overall death toll. Population density plays a crucial role, as does access to clean water and sanitation. Medical advancements, such as the development of vaccines and antibiotics, have significantly reduced mortality from many infectious diseases. Nutritional status of the population is another critical factor.
- Population Density: High population density facilitates the spread of infectious diseases.
- Sanitation and Hygiene: Poor sanitation and hygiene practices contribute to the transmission of infectious diseases.
- Medical Interventions: Access to healthcare, including vaccines and treatments, greatly affects mortality rates.
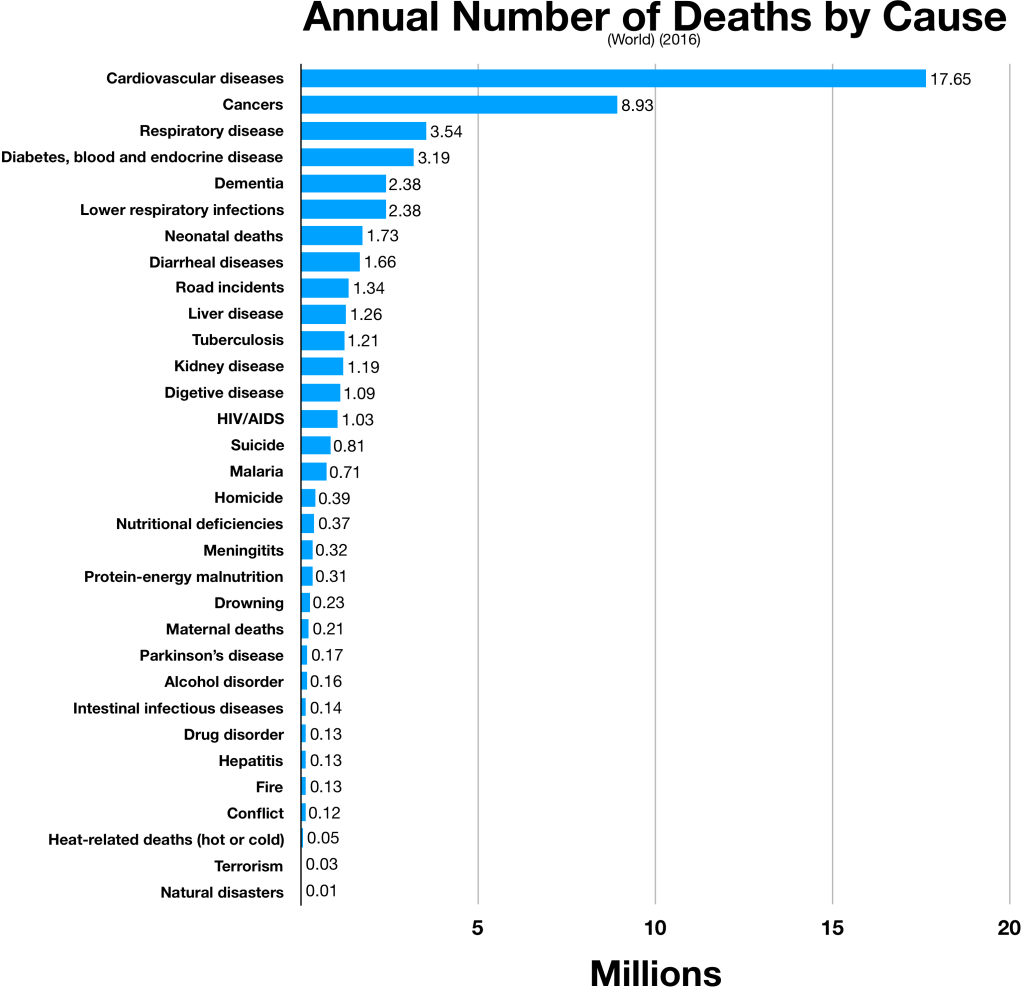
What is the number 1 disease that causes death?
Ischemic heart disease is the number one cause of death globally.
What is Ischemic Heart Disease?
Ischemic heart disease (IHD), also known as coronary artery disease (CAD), is a condition where the blood flow to the heart muscle is reduced, usually due to atherosclerosis. Atherosclerosis is a process where plaque builds up inside the arteries, narrowing them and restricting blood flow. This reduced blood flow deprives the heart muscle of oxygen and nutrients, leading to a range of problems, from angina (chest pain) to heart attacks and ultimately, death. The severity and impact of IHD depend on the extent of the blockage and the individual's overall health.
- Reduced blood flow to the heart muscle is the hallmark of IHD.
- Atherosclerosis is the primary cause of this reduced blood flow.
- Symptoms can range from mild chest discomfort to severe heart attacks.
Risk Factors for Ischemic Heart Disease
Numerous factors increase the risk of developing IHD. These can be broadly categorized as modifiable and non-modifiable risk factors. Modifiable risk factors, which can be changed through lifestyle choices or medical interventions, include smoking, high blood pressure, high cholesterol, obesity, diabetes, lack of physical activity, and unhealthy diet. Non-modifiable risk factors, such as age, family history, and gender, cannot be altered. Understanding and managing these risk factors is crucial in preventing IHD.
- Modifiable risk factors: Smoking, high blood pressure, high cholesterol, obesity, diabetes, physical inactivity, unhealthy diet.
- Non-modifiable risk factors: Age, family history, gender.
- Effective management of risk factors is key to prevention.
Symptoms of Ischemic Heart Disease
Symptoms of IHD can vary significantly depending on the severity of the disease and the individual. Many experience angina, a squeezing or pressure sensation in the chest, often triggered by physical exertion or stress. However, some individuals, particularly women, may experience atypical symptoms such as shortness of breath, fatigue, nausea, or back pain. In severe cases, IHD can lead to a heart attack (myocardial infarction), which is a life-threatening event characterized by sudden, intense chest pain, shortness of breath, and potential loss of consciousness. Prompt medical attention is crucial in these situations.
- Angina: Chest pain or pressure.
- Atypical symptoms: Shortness of breath, fatigue, nausea, back pain.
- Heart attack (myocardial infarction): A life-threatening emergency requiring immediate medical attention.
Diagnosis and Treatment of Ischemic Heart Disease
Diagnosis of IHD typically involves a combination of physical examination, electrocardiogram (ECG), blood tests, and imaging techniques such as echocardiography or coronary angiography. Treatment options depend on the severity of the disease and may include lifestyle modifications, medications (such as statins, beta-blockers, and aspirin), angioplasty, or coronary artery bypass grafting (CABG) surgery. Early diagnosis and treatment are crucial in preventing complications and improving survival rates.
- Diagnosis involves physical exam, ECG, blood tests, and imaging.
- Treatment options include lifestyle changes, medications, angioplasty, and CABG surgery.
- Early intervention is vital for optimal outcomes.
Global Impact and Prevention of Ischemic Heart Disease
Ischemic heart disease poses a significant global health burden, accounting for a substantial number of deaths annually. Preventive measures play a crucial role in reducing its incidence and impact. These include adopting a heart-healthy lifestyle, which encompasses regular exercise, a balanced diet low in saturated and trans fats, maintaining a healthy weight, not smoking, managing blood pressure and cholesterol levels, and regular health checkups. Public health initiatives aimed at promoting heart-healthy lifestyles are essential in combating this leading cause of death.
- IHD is a major global health concern.
- Prevention is crucial through lifestyle modification and regular health checks.
- Public health initiatives are vital in reducing the burden of IHD.
What disease kills you the quickest?

There is no single disease that universally kills the quickest. The speed of death depends on numerous factors, including the specific strain of the disease, the individual's overall health, access to medical care, and the promptness of treatment. However, some diseases are known for their rapid progression and high mortality rate if left untreated.
Rapidly Fatal Infections
Some bacterial infections, like fulminant meningococcal septicemia (a severe form of meningitis), can progress incredibly rapidly. Untreated, it can lead to death within hours. Other rapidly progressing bacterial infections include necrotizing fasciitis ("flesh-eating bacteria") and certain forms of pneumonia. The speed of death depends heavily on the virulence of the bacteria, the host's immune response, and the availability of effective antibiotics. Early diagnosis and aggressive treatment are crucial for survival.
- Speed of Onset: Symptoms can develop within hours, making early detection challenging.
- Severity of Symptoms: Symptoms are often severe and rapidly worsen, including high fever, shock, and organ failure.
- Treatment: Immediate administration of antibiotics is essential; delays greatly reduce survival chances.
Neurological Diseases with Rapid Progression
Certain neurological diseases can also be incredibly fast-acting. Rabies, for instance, is almost always fatal if untreated. While the incubation period can vary, once symptoms appear, death usually occurs within days to weeks due to inflammation of the brain. Other rapidly progressive neurological conditions, though less common, can also cause death within a short time frame.
- Incubation Period: Varies greatly, but once symptoms appear the progression is rapid.
- Symptoms: Include fever, headache, muscle weakness, confusion, and eventually paralysis.
- Treatment: Post-exposure prophylaxis (PEP) is effective before symptoms appear; treatment after symptoms is rarely successful.
Cardiovascular Events
While not strictly "diseases" in the same way as infections, certain cardiovascular events can cause death exceptionally quickly. A massive myocardial infarction (heart attack), for example, can lead to sudden cardiac arrest and death within minutes. The speed of death depends on the size and location of the blockage in the coronary artery, as well as the individual's heart health. Similarly, a ruptured aortic aneurysm can also cause near-instantaneous death due to massive internal bleeding.
- Sudden Onset: Often occurs without warning and leads to immediate circulatory collapse.
- Severity: Results in immediate life-threatening conditions.
- Treatment: Requires immediate medical intervention such as CPR, defibrillation, or surgery.
Toxins and Poisons
Exposure to certain toxins and poisons can also lead to incredibly rapid death. Cyanide poisoning, for example, can cause death within minutes due to its rapid interference with cellular respiration. Other highly toxic substances, including certain venoms and nerve agents, can also induce extremely rapid mortality.
- Mechanism of Action: Interfere with essential bodily functions very quickly.
- Symptoms: Vary depending on the substance but often include respiratory failure, seizures, and cardiac arrest.
- Treatment: Specific antidotes may exist but often require immediate administration to be effective.
Severe Allergic Reactions
Anaphylaxis is a severe, life-threatening allergic reaction. It can cause a rapid drop in blood pressure, airway constriction, and circulatory collapse, leading to death within minutes if not treated immediately with epinephrine. The speed of death is highly dependent on the individual's sensitivity to the allergen and the promptness of treatment.
- Allergic Trigger: Can be triggered by a wide range of substances, including insect stings, medications, and foods.
- Rapid Progression: Symptoms such as hives, swelling, breathing difficulties, and dizziness can develop rapidly.
- Treatment: Immediate administration of epinephrine via auto-injector is crucial, followed by emergency medical care.
What disease is the #1 killer in the United States today?
Heart disease is the 1 killer in the United States today.
What is Heart Disease?
Heart disease, also known as cardiovascular disease (CVD), encompasses a range of conditions affecting the heart and blood vessels. It's a broad term that includes several specific diseases, all stemming from a buildup of plaque in the arteries (atherosclerosis). This plaque buildup narrows the arteries, reducing blood flow to the heart and other organs. The most common types of heart disease include coronary artery disease (CAD), heart failure, stroke, and high blood pressure (hypertension). These conditions can lead to serious complications and even death if left untreated.
- Coronary Artery Disease (CAD): Narrowing of the coronary arteries, reducing blood flow to the heart muscle.
- Heart Failure: The heart's inability to pump enough blood to meet the body's needs.
- Stroke: Blood supply to part of the brain is interrupted, causing brain damage.
Risk Factors for Heart Disease
Numerous factors increase the risk of developing heart disease. Some are modifiable, meaning they can be changed through lifestyle choices, while others are non-modifiable, such as age and family history. Managing modifiable risk factors is crucial in preventing heart disease. These factors include unhealthy diet, lack of physical activity, smoking, obesity, high blood pressure, high cholesterol, and diabetes.
- Modifiable Risk Factors: Diet, exercise, smoking, weight management, blood pressure, cholesterol levels, diabetes management.
- Non-Modifiable Risk Factors: Age, sex, family history, ethnicity.
- Other Risk Factors: Stress, sleep apnea, certain medical conditions.
Symptoms of Heart Disease
Symptoms of heart disease can vary greatly depending on the specific condition. Some individuals may experience no symptoms at all, even with significant disease, while others may experience chest pain (angina), shortness of breath, fatigue, irregular heartbeat, and swelling in the legs and ankles. It's crucial to seek medical attention if you experience any concerning symptoms, even if they seem mild. Early diagnosis and treatment can significantly improve outcomes.
- Chest Pain (Angina): Pressure, tightness, or pain in the chest.
- Shortness of Breath: Difficulty breathing, especially during exertion.
- Fatigue: Unexplained tiredness or weakness.
Diagnosis and Treatment of Heart Disease
Diagnosing heart disease typically involves a physical examination, medical history review, and various diagnostic tests. These tests may include electrocardiograms (ECGs), echocardiograms, stress tests, and blood tests. Treatment options vary depending on the specific condition and its severity but may include lifestyle changes, medications, minimally invasive procedures, or surgery.
- Lifestyle Changes: Diet, exercise, smoking cessation, weight management.
- Medications: Blood pressure medication, cholesterol-lowering drugs, blood thinners.
- Procedures and Surgery: Angioplasty, bypass surgery, valve repair/replacement.
Prevention of Heart Disease
Preventing heart disease involves adopting a healthy lifestyle that addresses modifiable risk factors. This includes maintaining a healthy weight, eating a balanced diet rich in fruits, vegetables, and whole grains, engaging in regular physical activity, avoiding smoking, and managing stress levels. Regular checkups with your doctor are also crucial for early detection and management of any potential problems.
- Healthy Diet: Focus on fruits, vegetables, whole grains, and lean proteins.
- Regular Exercise: Aim for at least 150 minutes of moderate-intensity aerobic activity per week.
- Stress Management: Practice relaxation techniques such as yoga or meditation.
What is the biggest killer of all time?
Determining the single biggest killer of all time is complex and depends on how you define "killer" and what data you consider. There isn't a definitive answer readily available, as accurate global mortality data throughout history is extremely limited and often unreliable. However, several strong contenders exist. Infectious diseases, such as the Black Death (bubonic plague), have historically claimed the lives of millions, even decimating entire populations. Estimates for the Black Death range from 30% to 60% of Europe’s population. Similarly, other pandemics like the 1918 influenza pandemic (Spanish Flu) killed tens of millions worldwide. While these events caused devastating spikes in mortality, malnutrition and famine have also been responsible for an immense number of deaths throughout history, often exacerbated by conflict, disease, and environmental factors. It's important to note that these factors are often intertwined; famine weakens individuals, making them more susceptible to infectious diseases. Therefore, attributing a single cause as the absolute "biggest killer" is problematic. Instead of focusing on a single disease, it’s more accurate to consider the cumulative impact of infectious diseases, malnutrition, and related factors over millennia as the primary cause of mortality throughout human history.
Can we pinpoint one specific disease as the biggest killer?
No, we cannot definitively pinpoint one specific disease as the biggest killer of all time. The difficulty lies in several factors. First, historical record-keeping was inconsistent, especially in pre-modern times. Accurate mortality statistics are simply unavailable for much of human history. Secondly, many deaths were caused by a combination of factors rather than a single disease. A person weakened by malnutrition might be far more susceptible to succumbing to an infectious disease. Similarly, poor sanitation and lack of clean water dramatically increased death rates from easily preventable illnesses. Therefore, separating the cause of death into neat categories can be misleading. Even with modern data, assigning a precise cause of death can be complicated. Someone dying from pneumonia may have underlying health conditions that contributed significantly to their demise. Finally, the impact of certain diseases varied widely across different populations and geographical regions due to factors such as climate, immunity, and access to healthcare. Any attempt to declare a single “biggest killer” ignores the complexities of human mortality throughout history.
What are some of the leading contenders for the title of biggest killer?
Several diseases and factors compete for the title of biggest killer of all time. As previously mentioned, infectious diseases are strong contenders, especially those that caused widespread pandemics. The Black Death and the 1918 influenza pandemic are two prime examples. However, malnutrition and famine are equally strong contenders. These have caused countless deaths throughout history, often exceeding those directly caused by a single disease outbreak. Additionally, diseases related to poverty and poor sanitation, such as diarrheal diseases, tuberculosis, and respiratory infections, have contributed significantly to global mortality. Conflict and warfare also dramatically increase mortality rates, both directly through combat and indirectly through famine, disease, and displacement. The difficulty isn't in identifying diseases with high death tolls, but rather in comparing vastly different contexts, data limitations, and the often interwoven nature of the causes of death across vast stretches of time.
How does the impact of disease change over time?
The impact of disease has dramatically changed over time, primarily due to advances in medicine, sanitation, and public health. In pre-modern societies, infectious diseases were rampant due to poor hygiene, lack of understanding of disease transmission, and limited access to treatment. The development of vaccinations, antibiotics, and improved sanitation practices has significantly reduced the mortality rates associated with many previously devastating illnesses. However, emerging infectious diseases and antibiotic resistance remain significant challenges. Furthermore, while infectious diseases are less prevalent in many parts of the world, non-communicable diseases (NCDs) like heart disease, cancer, and diabetes are now leading causes of death globally, often linked to lifestyle factors such as diet, smoking, and lack of exercise. The changing landscape of disease highlights the continuous need for improved healthcare infrastructure, public health initiatives, and ongoing research to address emerging challenges and mitigate the impact of both infectious and non-communicable diseases.
/data-and-analytics-(dna)/monitoring-forecasting-inequalities-(mfi)/global_both_sexes.svg?sfvrsn=97146ffc_1)
Deja una respuesta