What is silent sepsis

Silent sepsis, a stealthy and often deadly infection, has emerged as a significant threat, particularly among hospitalized patients. Unlike classic sepsis, which presents with overt symptoms, silent sepsis is characterized by a deceptively benign presentation, making it difficult to diagnose and treat promptly. This article delves into the nature of silent sepsis, exploring its unique characteristics, risk factors, and implications for healthcare professionals. By shedding light on this elusive condition, we aim to improve recognition, facilitate timely intervention, and ultimately save lives.
What is Silent Sepsis? Understanding the Hidden Threat
Silent sepsis, also known as occult sepsis, is a dangerous condition where the classic signs and symptoms of sepsis are either absent or very subtle. This makes it incredibly difficult to diagnose, leading to delayed treatment and potentially life-threatening consequences. Unlike typical sepsis, which presents with obvious signs like fever, rapid heart rate, and low blood pressure, silent sepsis can develop insidiously, often mimicking other illnesses or appearing as seemingly minor ailments. This makes early detection crucial, as prompt intervention can significantly improve outcomes. The lack of clear indicators makes it particularly challenging for healthcare professionals to identify and manage, emphasizing the importance of increased awareness and thorough investigation of seemingly minor symptoms.
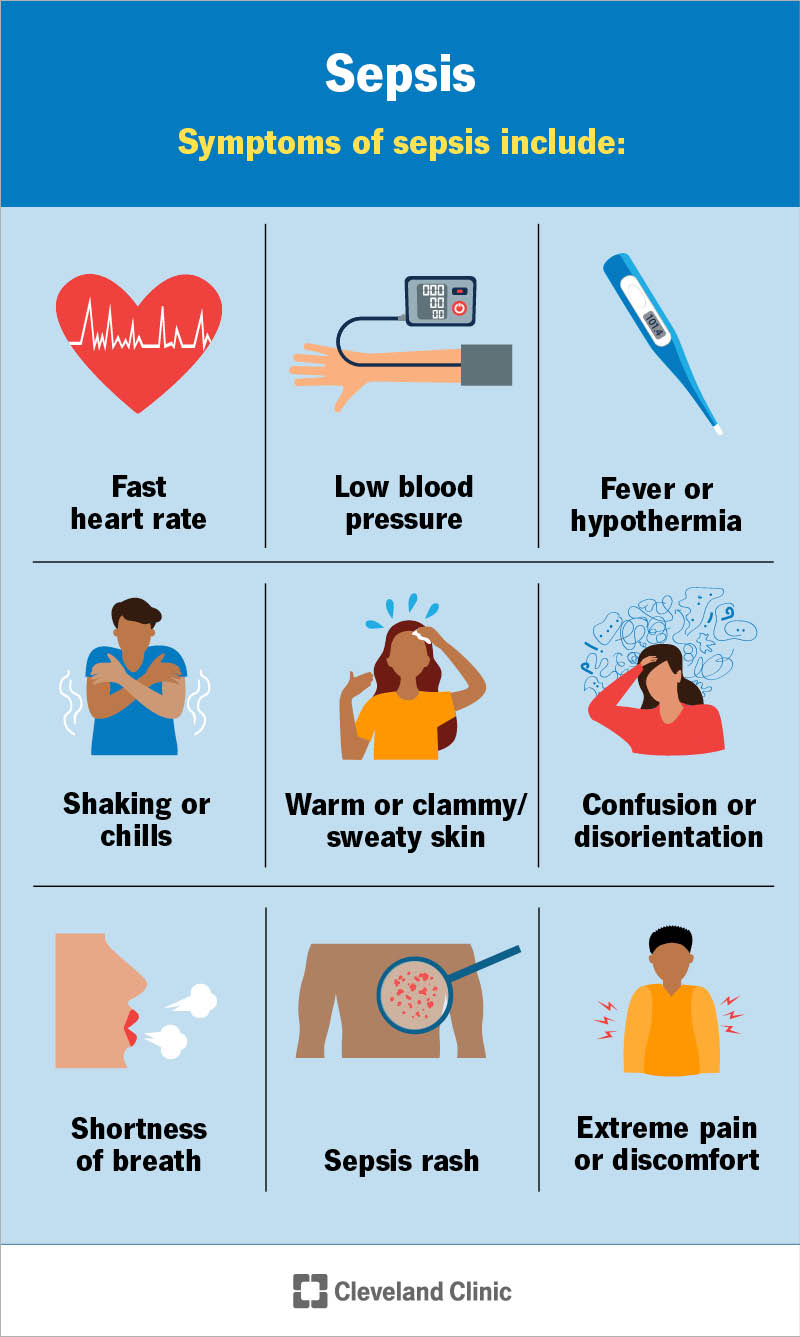
What are the typical symptoms of silent sepsis?
The insidious nature of silent sepsis means that symptoms are often vague and non-specific, making it difficult to distinguish from other conditions. Instead of the typical high fever and rapid heart rate associated with sepsis, patients might experience subtle changes such as mild confusion, unexplained fatigue, general malaise, mild shortness of breath, or a slight increase in heart rate. These symptoms can be easily overlooked or attributed to other less serious causes, delaying diagnosis and treatment. Changes in mental status, such as decreased alertness or confusion, can be a crucial, albeit subtle, indicator. Gastrointestinal issues such as nausea, vomiting, or diarrhea can also be present. It's vital to pay close attention to any unusual changes in your body and seek medical attention if concerned.
Who is at higher risk of developing silent sepsis?
While anyone can develop sepsis, certain individuals are at a higher risk of experiencing the silent form. Older adults, particularly those with pre-existing conditions such as diabetes or heart disease, are more vulnerable. Their immune systems may be weakened, and their bodies may not respond to infection in the typical, more noticeable ways. Individuals with weakened immune systems due to diseases like HIV or those undergoing chemotherapy are also at increased risk. Infants and young children might not exhibit the classic signs of sepsis, making it crucial for parents and caregivers to be vigilant about subtle changes in their behavior or overall health. People with chronic illnesses that compromise their immune function or organ systems are also at a significantly increased risk.
How is silent sepsis diagnosed?
Diagnosing silent sepsis is challenging due to the absence of typical symptoms. Blood tests are crucial for identifying infection and assessing organ function. Imaging studies, such as chest X-rays or CT scans, might be necessary to identify the source of infection. Detailed medical history is vital, including recent illnesses, surgeries, or injuries. Careful monitoring of vital signs, even seemingly minor changes, can help detect subtle signs of deterioration. Lactate levels, a marker of tissue oxygen deprivation, are often monitored closely. Early and aggressive treatment is critical for improving outcomes, highlighting the need for a high index of suspicion in at-risk patients.
What is the treatment for silent sepsis?
Prompt and aggressive treatment is critical for managing silent sepsis. Antibiotics are typically administered immediately to combat the infection. Intravenous fluids are often given to maintain blood pressure and improve organ perfusion. Supportive care, such as oxygen therapy and monitoring of vital signs, is essential. Treatment focuses on addressing the underlying infection and supporting the body's natural ability to fight the infection. The specific treatment approach will depend on the source of the infection and the individual's overall health status. Early intervention significantly improves the chances of survival and recovery.
What are the long-term effects of silent sepsis?
Even with successful treatment, silent sepsis can have long-term consequences. Organ damage, especially to the kidneys, lungs, or heart, is possible. Cognitive impairment, such as difficulty concentrating or memory problems, can occur. Physical limitations, such as fatigue and weakness, can persist. Psychological impact, including anxiety and depression, can be significant. Early diagnosis and treatment are essential to minimize the risk of these long-term effects. Ongoing monitoring and rehabilitation may be necessary to help patients recover and manage any residual effects.
| Symptom | Description | Significance |
|---|---|---|
| Mild Confusion | Slight disorientation or difficulty concentrating. | Can be an early sign of sepsis, often overlooked. |
| Unexplained Fatigue | Persistent tiredness and lack of energy. | May indicate underlying infection or inflammation. |
| Slight Increase in Heart Rate | A subtle elevation in heart rate without other obvious causes. | Body's attempt to compensate for reduced blood flow. |
| Mild Shortness of Breath | Slightly labored breathing or feeling breathless without exertion. | Possible indication of reduced oxygen levels. |
| Gastrointestinal Issues | Nausea, vomiting, or diarrhea. | Can accompany systemic infection. |
What are the symptoms of silent sepsis?
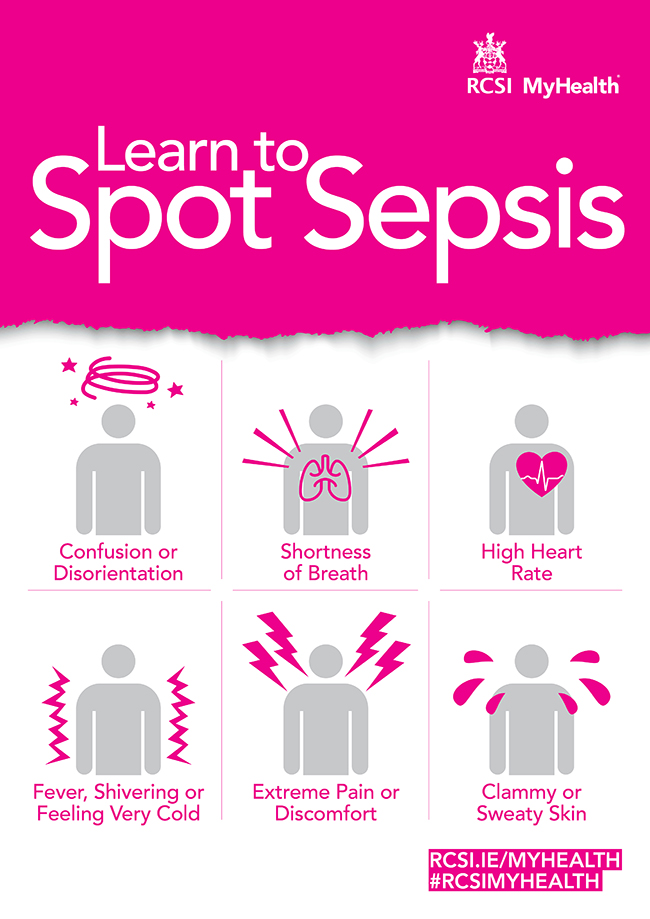
Silent sepsis, also known as occult sepsis, is a dangerous condition because its symptoms are often subtle, vague, and easily dismissed. Unlike typical sepsis, which presents with a dramatic and obvious inflammatory response, silent sepsis can develop insidiously, making early diagnosis challenging. This often leads to delays in treatment, increasing the risk of severe complications and even death. The symptoms can vary widely depending on the underlying infection and the individual's overall health. Many times, patients experience symptoms that mimic other, less serious illnesses, further hindering prompt identification.
General Malaise and Fatigue
One of the most common early signs of silent sepsis is a general feeling of being unwell. This might manifest as unexplained fatigue, significantly more tiredness than usual, or a persistent lack of energy. Other symptoms accompanying this malaise might be subtle and easy to overlook. This makes it difficult for patients and even medical professionals to connect these seemingly benign symptoms to a severe underlying infection. It is crucial to pay attention to even seemingly minor changes in one's energy levels, especially if accompanied by other symptoms.
- Persistent fatigue: More severe than typical tiredness; lasting for days or weeks.
- Unexplained weakness: Difficulty performing routine tasks.
- General feeling of illness: A vague sense of being unwell without a clear cause.
Changes in Mental Status
Silent sepsis can affect brain function, leading to noticeable changes in mental clarity and alertness. Confusion, disorientation, and difficulty concentrating are common indicators. These cognitive impairments can be sudden or gradual, making them harder to recognize as sepsis symptoms. Older adults, those with pre-existing conditions like dementia, or individuals already experiencing cognitive decline might exhibit less obvious mental status changes, making the identification of silent sepsis particularly challenging in these populations.
- Confusion: Disorientation to time, place, or person.
- Lethargy: Excessive drowsiness and sluggishness.
- Difficulty concentrating: Trouble focusing or remembering things.
Gastrointestinal Symptoms
Silent sepsis can present with various gastrointestinal symptoms, including nausea, vomiting, diarrhea, or abdominal pain. The severity and type of gastrointestinal symptoms can vary widely depending on the location of the infection. For example, an infection in the abdomen might present with more pronounced abdominal pain, while an infection elsewhere might only cause mild nausea or diarrhea. These symptoms can easily be attributed to less serious conditions like indigestion or a stomach bug, further delaying diagnosis and treatment.
- Nausea and Vomiting: Feeling sick to the stomach and throwing up.
- Diarrhea: Loose or watery stools.
- Abdominal Pain: Discomfort or pain in the stomach area.
Subtle Fever or Temperature Fluctuations
A high fever is a classic sign of infection, but in silent sepsis, the fever might be low-grade or intermittent. Patients might experience subtle temperature fluctuations or only slight elevations in temperature that are easily missed or attributed to other factors. The absence of a high fever does not rule out sepsis. It's crucial to monitor temperature regularly, especially if other symptoms are present.
- Low-grade fever: Slightly elevated temperature, often below 101°F (38.3°C).
- Intermittent fever: Fluctuations in temperature, with periods of normal temperature interspersed with fever.
- Chills: Feeling cold despite a normal or slightly elevated temperature.
Respiratory Changes
While shortness of breath is a common symptom of sepsis, silent sepsis might present with subtle respiratory changes that are easily overlooked. These could include increased respiratory rate, slight shortness of breath, or a feeling of tightness in the chest. These symptoms might be attributed to other respiratory conditions such as mild asthma or allergies, further delaying proper diagnosis and treatment. Any change in breathing pattern or comfort should be investigated.
- Increased respiratory rate: Breathing faster than usual.
- Slight shortness of breath: Feeling slightly winded or out of breath.
- Chest tightness: A feeling of pressure or discomfort in the chest.
Can you have sepsis for days without knowing?
Yes, it is possible to have sepsis for days without knowing. Sepsis, a life-threatening condition arising from the body's overwhelming response to an infection, can develop subtly and its early symptoms are often non-specific and easily mistaken for other common illnesses. This means that the initial signs might be overlooked or attributed to something less serious, delaying diagnosis and treatment, which can have severe consequences. The insidious onset allows the infection to progress unchecked, potentially leading to organ damage and a higher risk of mortality.
Early Sepsis Symptoms Can Be Subtle
Early sepsis symptoms can be very subtle and easily dismissed. Many people initially experience symptoms that are non-specific and can mimic the flu or a common cold. This makes early detection challenging, as the symptoms aren't immediately alarming. Early recognition is crucial for improving outcomes. The delay in diagnosis, often caused by the ambiguity of early symptoms, makes the disease more difficult to treat and increases the chances of complications.
- Fever or chills: These can be mild and easily overlooked.
- Fatigue and weakness: Often attributed to stress or lack of sleep.
- Increased heart rate: May not be noticeable without monitoring.
Sepsis Mimics Other Illnesses
One of the major challenges in diagnosing sepsis early is that its initial symptoms often mimic other, less severe illnesses. This similarity makes it difficult for both patients and healthcare providers to distinguish sepsis from more benign conditions. Therefore, a thorough medical evaluation is needed to properly diagnose and address this potentially life-threatening situation. The overlapping symptoms can lead to delays in diagnosis and treatment.
- Influenza (flu): Sepsis can share symptoms like fever, chills, muscle aches, and fatigue.
- Gastroenteritis: Nausea, vomiting, and diarrhea can be present in both conditions.
- Pneumonia: Respiratory symptoms can overlap, making it difficult to differentiate.
Individual Variability in Sepsis Presentation
The presentation of sepsis can vary significantly from person to person, making it even harder to diagnose. Some individuals may experience only mild symptoms, while others may exhibit more severe manifestations. This variability underscores the importance of prompt medical attention when any concerning symptoms are present. The severity of symptoms can differ dramatically among individuals. This variability is why it's crucial to seek medical advice if you're concerned.
- Age and overall health: Older adults and those with pre-existing conditions may present differently.
- Underlying infection type: The source of infection impacts symptom presentation.
- Immune system strength: A weakened immune system can lead to a more severe response.
Delayed Diagnosis Increases Severity
A delay in sepsis diagnosis significantly worsens the prognosis. The longer the infection goes untreated, the more likely it is to cause organ damage and lead to long-term complications or even death. Early intervention is key to improving survival rates and reducing the risk of long-term health problems. Prompt treatment is essential in reducing the severity of sepsis and its complications.
- Organ damage: Untreated sepsis can damage vital organs like kidneys, lungs, and heart.
- Increased mortality risk: Delayed diagnosis and treatment significantly increase the risk of death.
- Long-term disability: Sepsis survivors can experience long-term physical and cognitive impairments.
Lack of Awareness Contributes to Delayed Diagnosis
A significant factor contributing to delayed sepsis diagnosis is a lack of public awareness about the condition and its subtle early signs. Many individuals are unfamiliar with the symptoms and the urgency of seeking medical attention. Increased public awareness about the signs and symptoms of sepsis can lead to earlier diagnosis and treatment. Educating the public about the importance of seeking prompt medical care is crucial in improving outcomes.
- Misinterpretation of symptoms: Many people attribute early symptoms to less serious illnesses.
- Delayed seeking medical attention: This delay can have serious consequences.
- Underdiagnosis by healthcare providers: Early signs are often subtle and can be easily missed.
What are the three types of sepsis?
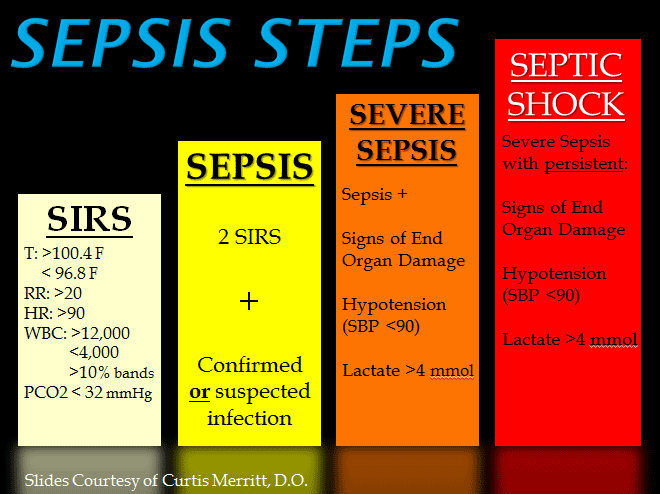
There isn't a universally agreed-upon classification of sepsis into precisely threedistinct types. Sepsis is a clinical syndrome, not a disease with discrete subtypes. Instead, sepsis is staged based on its severity and progression. The stages are often described as sepsis, severe sepsis, and septic shock. However, the term "severe sepsis" is increasingly being phased out in favor of a simpler, two-stage classification: sepsis and septic shock. The descriptions below reflect this evolving understanding.
Sepsis
Sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection. This means the body's response to an infection is overwhelming and damaging to its own tissues and organs. It's crucial to understand that sepsis isn't simply a severe infection; it's the body's reactionto the infection that causes the harm.
- Characterized by: A suspected or confirmed infection, along with evidence of organ dysfunction (e.g., altered mental status, low blood pressure, high heart rate, low urine output).
- Diagnosis: Relies on clinical assessment and laboratory tests, such as blood cultures, complete blood count (CBC), and lactate levels.
- Treatment: Focuses on identifying and treating the underlying infection (e.g., with antibiotics), providing supportive care to maintain organ function (e.g., fluid resuscitation, vasopressors), and monitoring for complications.
Septic Shock
Septic shock represents the most severe form of sepsis. It's characterized by persistent hypotension despite adequate fluid resuscitation. This means the blood pressure remains dangerously low even after attempts to increase fluid volume in the body. This is a sign of severe circulatory failure caused by the body's overwhelming immune response.
- Defining Feature: Persistent hypotension requiring vasopressors to maintain adequate blood pressure.
- Organ Dysfunction: Marked by multiple organ failure due to inadequate blood flow and oxygen delivery.
- High Mortality Risk: Septic shock carries a significantly higher mortality rate compared to sepsis without shock, necessitating immediate and aggressive treatment.
Organ Dysfunction in Sepsis
Organ dysfunction is a central feature of both sepsis and septic shock. It reflects the damage the body's excessive immune response inflicts on various organs and systems. The specific organs affected can vary, but common manifestations include acute kidney injury, respiratory failure, and altered mental status.
- Acute Kidney Injury (AKI): Impaired kidney function, often leading to a decreased ability to filter waste products from the blood.
- Respiratory Failure: Inability of the lungs to adequately exchange oxygen and carbon dioxide, often requiring mechanical ventilation.
- Acute Liver Injury: Elevated liver enzymes that indicate damage to the liver, often leading to impaired clotting factors and other biochemical abnormalities.
The Role of Infection in Sepsis
Sepsis always originates from an infection, although identifying the specific infection source can sometimes be challenging. The infection might be localized (e.g., pneumonia, urinary tract infection) or spread throughout the body (sepsis). The severity of sepsis does not always correlate directly with the severity of the initial infection.
- Common Sources: Pneumonia, urinary tract infections, intra-abdominal infections, skin and soft tissue infections, and bloodstream infections.
- Diagnostic Challenges: Identifying the source of infection is crucial for effective treatment, but it may require extensive investigation (e.g., imaging tests, cultures).
- Impact on Treatment: Once the infection source is identified, targeted antibiotic therapy is essential to manage the underlying infection and improve outcomes.
Management and Treatment of Sepsis
Early recognition and treatment are critical in improving outcomes for individuals with sepsis. Treatment aims to control the infection, support vital organ functions, and manage complications. This requires a multidisciplinary approach involving intensive care specialists, infectious disease experts, and other healthcare professionals.
- Rapid Assessment: Prompt identification of sepsis is vital, often involving quick assessment of vital signs, laboratory tests, and imaging studies.
- Fluid Resuscitation: Replenishing fluid volume is crucial to restore blood pressure and improve tissue perfusion.
- Antibiotic Therapy: Broad-spectrum antibiotics are usually administered immediately while awaiting culture results to identify the specific causative organism.
What are the symptoms of mild sepsis?
Mild sepsis, also known as systemic inflammatory response syndrome (SIRS), can present with a wide range of symptoms, and they can be subtle and easily overlooked. It's crucial to remember that mild sepsis is a serious condition that requires prompt medical attention to prevent progression to severe sepsis or septic shock. Symptoms are often non-specific, meaning they overlap with many other illnesses. The intensity of symptoms varies greatly depending on the individual's overall health, the source of infection, and the body's response.
Fever or Hypothermia
A hallmark symptom of sepsis is a fever (temperature above 101°F or 38.3°C). However, in some cases, particularly in older adults or individuals with weakened immune systems, sepsis can manifest as hypothermia (temperature below 96.8°F or 36°C). This temperature fluctuation is caused by the body's dysregulated response to infection. Changes in body temperature often accompany other symptoms and should be taken seriously, especially in conjunction with other symptoms.
- Fever: Temperature above 101°F (38.3°C)
- Hypothermia: Temperature below 96.8°F (36°C)
- Chills: Feeling cold and shivering, even with a fever.
Increased Heart Rate and Breathing Rate
The body's response to infection often includes an increased heart rate (tachycardia) and respiratory rate (tachypnea). This is the body's attempt to compensate for the reduced blood flow and oxygenation that can occur during sepsis. The increased heart rate helps circulate blood and oxygen more effectively, while increased breathing attempts to take in more oxygen. These changes are often subtle initially but can worsen as sepsis progresses.
- Tachycardia: Rapid heart rate (over 90 beats per minute)
- Tachypnea: Rapid breathing rate (over 20 breaths per minute)
- Shortness of breath: Difficulty breathing or feeling winded.
Changes in White Blood Cell Count
Changes in the white blood cell count (WBC) are a common laboratory finding in sepsis. While a high WBC count often indicates infection, sometimes the count can be low (leukopenia) or even normal. The body's response to infection is complex and WBC count alone is not diagnostic. This requires further testing to rule out other causes.
- Leukocytosis: Elevated white blood cell count
- Leukopenia: Decreased white blood cell count
- Normal WBC count: Can still occur in some cases of sepsis.
Mental Status Changes
Mild sepsis can cause subtle changes in mental status, such as confusion, disorientation, or lethargy. These cognitive changes occur due to the body's overall inflammatory response and the potential for reduced oxygen delivery to the brain. These cognitive changes, however mild, require immediate medical attention as they can indicate worsening infection.
- Confusion: Difficulty thinking clearly
- Disorientation: Feeling lost or unaware of surroundings
- Lethargy: Feeling unusually tired or sluggish
Other Symptoms
Mild sepsis can also present with a variety of other non-specific symptoms, including extreme fatigue, muscle aches, nausea, vomiting, diarrhea, and abdominal pain. These symptoms can overlap with many common illnesses. The combination of several symptoms, rather than any single symptom, is more suggestive of sepsis.
- Fatigue: Extreme tiredness
- Muscle aches: Pain or soreness in the muscles
- Gastrointestinal symptoms: Nausea, vomiting, diarrhea, and abdominal pain
What is silent sepsis?
Silent sepsis, also known as hidden sepsis or occult sepsis, refers to a severe infection that doesn't present with the typical, easily recognizable signs and symptoms of sepsis. Unlike classic sepsis, which is characterized by high fever, rapid heart rate, low blood pressure, and confusion, silent sepsis can be deceptively subtle. Individuals may experience only mild or atypical symptoms, such as fatigue, malaise, or a slight temperature elevation that is easily dismissed. This makes diagnosis exceptionally challenging, as the body's typical warning signals are muted or absent altogether. The insidious nature of silent sepsis allows the infection to progress undetected, leading to potentially life-threatening complications, including organ damage and septic shock, often before a proper diagnosis can be made. Early recognition and treatment are crucial, but the very nature of the condition makes this difficult to achieve. Risk factors for silent sepsis can include underlying conditions like diabetes, immunocompromised states, or the presence of indwelling medical devices. Older adults are particularly vulnerable due to their often blunted inflammatory responses.
How is silent sepsis different from regular sepsis?
The key difference between silent sepsis and regular sepsis lies in the presentation of symptoms. Regular sepsis presents with a constellation of readily apparent signs, such as a high fever (often above 101°F or 38.3°C), rapid heart rate (tachycardia), rapid breathing (tachypnea), and a drop in blood pressure (hypotension). Patients often appear acutely ill, exhibiting symptoms like confusion, disorientation, or extreme lethargy. These classic manifestations allow for relatively prompt diagnosis and intervention. In contrast, silent sepsis is characterized by a lack of these dramatic symptoms. Instead, affected individuals may experience vague, nonspecific symptoms, such as mild fatigue, general weakness, subtle changes in mental state, or a low-grade fever that might be easily attributed to other causes. The insidious nature of silent sepsis means that the infection can progress significantly before it's detected, making early intervention more challenging and increasing the risk of severe complications. This difference in presentation highlights the importance of a high index of suspicion among healthcare professionals, especially when dealing with at-risk populations.
What are the symptoms of silent sepsis?
The symptoms of silent sepsis are often subtle and nonspecific, making it difficult to distinguish from other minor illnesses. This is precisely what makes silent sepsis so dangerous. Instead of the classic signs of sepsis, such as high fever and low blood pressure, individuals may experience symptoms like: unexplained fatigue and weakness, lasting longer than a few days; mild fever, possibly only a slight elevation in temperature; general malaise, a feeling of overall illness or discomfort; subtle changes in mental status, such as confusion, lethargy, or disorientation; decreased urine output; and shortness of breath. Importantly, the absence of a fever does not rule out sepsis. It's crucial to remember that the symptoms can be highly variable and depend on several factors, including the site of infection, the individual's immune status, and underlying medical conditions. Because the symptoms can mimic other common illnesses, a thorough medical evaluation is necessary to rule out silent sepsis, especially in individuals at high risk.
How is silent sepsis diagnosed?
Diagnosing silent sepsis is particularly challenging due to its atypical presentation. Standard sepsis diagnostic criteria often fail to capture the subtlety of this condition. Diagnosis relies on a combination of clinical assessment, laboratory tests, and imaging studies. A thorough medical history, including assessment of symptoms, risk factors, and recent medical interventions, is crucial. Blood tests, such as complete blood counts (CBC) and blood cultures to identify the infecting organism, are essential. Biomarkers, such as procalcitonin and C-reactive protein, can provide further clues, but they are not always definitive. Imaging studies like chest X-rays or CT scans may be used to identify the source of infection. The diagnosis often involves a process of elimination, comparing the patient’s symptoms and test results with other potential conditions. Given the insidious nature of silent sepsis, a high index of suspicion is critical for early diagnosis and treatment. Often, it's diagnosed after the patient has developed severe complications, emphasizing the need for prompt medical attention even when symptoms are vague or seemingly minor.
Deja una respuesta