What is the most painful chronic disease

Chronic pain is a debilitating condition that affects millions of people worldwide. It can be caused by a variety of underlying medical conditions, injuries, or other factors, and its intensity and duration can vary greatly. While all chronic pain is debilitating, some chronic diseases are widely recognized as causing some of the most severe and unrelenting pain imaginable. In this article, we will explore the various perspectives on the most painful chronic disease and provide insights into the experiences of those living with it.
What is the Most Painful Chronic Disease?
There's no single answer to the question of "what is the most painful chronic disease?" Pain is a subjective experience, varying greatly from person to person based on factors like genetics, tolerance, and psychological factors. What one person finds excruciating, another might find manageable. Further complicating matters, many chronic diseases involve multiple pain types (e.g., neuropathic, nociceptive, inflammatory) making direct comparison difficult. However, several chronic illnesses are frequently cited as being among the most painful.
Fibromyalgia: Widespread Chronic Pain
Fibromyalgia is characterized by widespread musculoskeletal pain accompanied by fatigue, sleep disturbances, and cognitive difficulties. The pain is often described as a deep, aching, and burning sensation that may be accompanied by tenderness to the touch at specific points on the body. The cause remains unknown, making diagnosis and treatment challenging. While there is no cure, management focuses on pain relief, improving sleep, and addressing other symptoms.
Trigeminal Neuralgia: Excruciating Facial Pain
Trigeminal neuralgia (TN) is a nerve disorder that causes severe, sudden, and sharp facial pain. The pain is typically described as electric shock-like sensations and can be triggered by seemingly innocuous stimuli such as touching the face, eating, or even a breeze. The unpredictable nature and intensity of the pain make it incredibly debilitating.
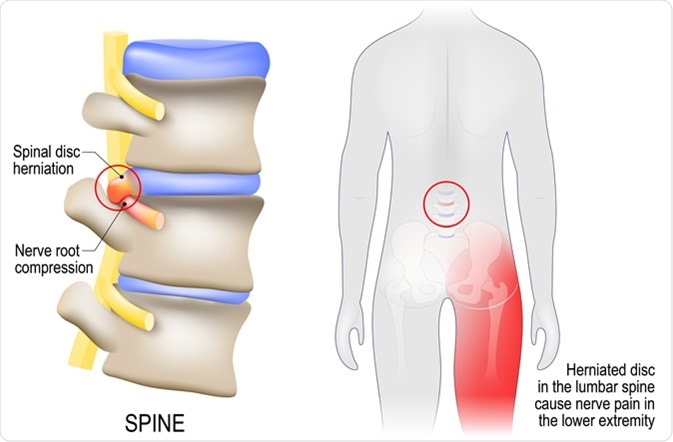
Complex Regional Pain Syndrome (CRPS): Persistent and Debilitating Pain
CRPS is a chronic pain condition that typically develops after an injury, surgery, or stroke. It's characterized by intense, burning pain that is disproportionate to the initial injury. Other symptoms may include swelling, changes in skin temperature and color, and impaired movement. The mechanisms underlying CRPS are not fully understood, but it's believed to involve dysfunction in the nervous system.
Osteoarthritis: Degenerative Joint Pain
Osteoarthritis is the most common form of arthritis, affecting millions worldwide. It is a degenerative joint disease that causes pain, stiffness, and reduced range of motion. The pain typically worsens with activity and improves with rest, though severe cases can experience pain even at rest. Osteoarthritis primarily affects weight-bearing joints like hips and knees, but can affect any joint in the body.
Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS): Chronic Bladder Pain
IC/BPS is a chronic condition characterized by pain in the bladder and pelvic region. Symptoms include persistent pelvic pain, urinary urgency and frequency, and pain during urination. The cause is unknown, and treatment focuses on managing pain and other symptoms.
| Disease | Primary Pain Characteristics | Other Key Symptoms |
|---|---|---|
| Fibromyalgia | Widespread musculoskeletal pain, aching, burning | Fatigue, sleep disturbances, cognitive difficulties |
| Trigeminal Neuralgia | Severe, sudden, sharp facial pain, electric shock-like sensations | Facial twitching, spasms |
| Complex Regional Pain Syndrome (CRPS) | Intense, burning pain, disproportionate to injury | Swelling, changes in skin temperature and color, impaired movement |
| Osteoarthritis | Pain, stiffness, reduced range of motion in joints | Joint swelling, deformity |
| Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS) | Pain in the bladder and pelvic region | Urinary urgency, frequency, pain during urination |
https://youtube.com/watch?v=index.html
What is the hardest chronic illness to live with?

There is no single answer to the question of . The experience of living with a chronic illness is profoundly personal and subjective. The "hardest" illness depends heavily on a multitude of factors, including: the specific symptoms, the individual's personality and coping mechanisms, available support systems, access to healthcare, and the overall impact on their quality of life. Conditions like cancer, heart disease, and multiple sclerosis are often cited as extremely challenging, but even less widely known illnesses can be devastatingly difficult for those who experience them. The severity and impact of a chronic illness also vary significantly from person to person, even within the same diagnosis.
The Impact of Pain on Daily Life
Chronic pain is a debilitating symptom present in many chronic illnesses, significantly impacting daily life. The constant ache, sharp stabs, or burning sensations can make even simple tasks incredibly difficult. The unpredictability of pain further exacerbates the problem, preventing individuals from engaging in activities or planning for the future. This unpredictable nature also leads to feelings of isolation, exhaustion, and anxiety, as sufferers often find themselves unable to maintain a regular routine.
- Difficulty performing everyday tasks such as dressing, bathing, or eating.
- Sleep disturbances due to pain and discomfort.
- Limited participation in social activities and relationships due to pain.
The Mental Health Toll of Chronic Illness
The psychological burden of living with a chronic illness is immense. Chronic illnesses frequently lead to anxiety, depression, and feelings of hopelessness. The uncertainty of the future, the constant need for medical attention, and the limitations imposed by the illness significantly impact mental well-being. This is further compounded by the potential for social isolation and financial strain.
- Increased risk of depression and anxiety disorders.
- Difficulty concentrating and decreased cognitive function.
- Social isolation and loneliness due to limitations imposed by the illness.
The Financial Burden of Chronic Illness
Chronic illnesses often incur substantial financial burdens. The cost of medication, doctor visits, specialized therapies, and adaptive equipment can quickly become overwhelming. Many individuals face significant financial strain, forcing them to make difficult choices between medical care and other essential needs. This financial instability can worsen stress and anxiety, further compounding the challenges of living with a chronic illness.
- High costs of medication, therapies, and medical equipment.
- Potential loss of income due to inability to work.
- Increased healthcare expenses leading to financial burden and debt.
The Impact on Relationships and Social Life
Chronic illnesses can profoundly impact relationships and social interactions. The limitations imposed by the illness, alongside the emotional toll it takes, can strain personal relationships. Individuals may struggle to maintain social connections due to fatigue, pain, or other symptoms. This isolation can lead to feelings of loneliness and exacerbate the challenges of managing the illness.
- Strain on relationships with family and friends due to illness-related limitations.
- Social isolation and feelings of loneliness.
- Difficulty participating in social activities and events.
The Importance of Individual Variation
It's crucial to emphasize that the experience of chronic illness is highly individualized. While some illnesses might present more significant physical challenges, others may have a greater impact on mental health or social functioning. There is no universal "hardest" illness; each individual's experience is shaped by their specific condition, their personality, their support system, and their access to resources.
- Variation in symptom severity and impact among individuals with the same diagnosis.
- The influence of personal coping mechanisms and support systems.
- The significant role of access to quality healthcare and resources.
What are the top 10 most painful?

What are the top 10 most painful experiences?
Defining the "top 10 most painful experiences" is inherently subjective and difficult due to the lack of a universally accepted pain scale that accounts for individual pain tolerance, psychological factors, and the context of the experience. Pain is a complex and personal sensation. However, based on medical literature, anecdotal evidence, and reported intensity, we can list some experiences commonly cited as extremely painful:
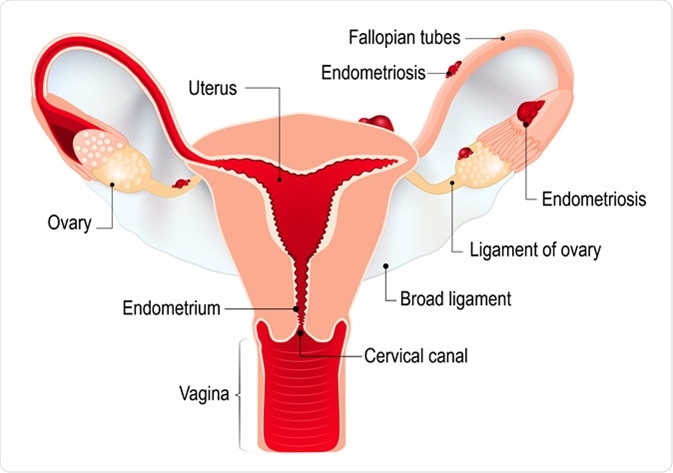
1. Childbirth
Childbirth is frequently cited as one of the most intensely painful experiences. The pain stems from the powerful contractions of the uterus and the stretching and dilation of the cervix. The pain is often described as intense, agonizing, and overwhelming.
- Intense uterine contractions cause significant muscle pain.
- Cervical dilation stretches the cervix to a considerable extent.
- Tissue trauma during delivery can contribute to the overall pain.
2. Kidney Stones
Kidney stones cause excruciating pain as they travel through the urinary tract. The sharp, cramping pain is often described as the worst pain a person can experience. The location and size of the stone significantly impact the severity of the pain.
- Sharp, stabbing pain radiating from the flank to the groin.
- Intense cramping in the abdomen and lower back.
- Nausea and vomiting often accompany the intense pain.
3. Cluster Headaches
Cluster headaches are severe, debilitating headaches that occur in clusters or groups. They are characterized by excruciating, intense pain, often localized around one eye. The pain is described as burning, piercing, or stabbing.
- Intense, unilateral pain behind or around one eye.
- Accompanying symptoms may include tearing, nasal congestion, and eyelid drooping.
- Attacks can last for minutes to hours, occurring multiple times a day.
4. Trigeminal Neuralgia
Trigeminal neuralgia, also known as tic douloureux, is a chronic pain condition affecting the trigeminal nerve, which carries sensation from the face. The pain is characterized by sudden, severe, electric shock-like sensations in the face.
- Sudden, sharp, shooting pains in the face.
- Pain triggered by everyday activities such as chewing, talking, or brushing teeth.
- Intense, debilitating pain that can significantly impact quality of life.
5. Burns
Severe burns cause intense, searing pain. The degree of pain depends on the depth and extent of the burn. Deep burns can damage nerve endings, leading to a complex, protracted pain experience. The pain is often associated with significant tissue damage and potential complications.
- Intense, searing pain immediately following the burn.
- Prolonged pain during healing and recovery.
- Risk of infection and other complications.
What is the most excruciating pain known to humanity?
Defining the single "most excruciating pain" is impossible due to the subjective nature of pain and the lack of a universally agreed-upon objective measurement scale. Pain perception varies widely between individuals based on factors like genetics, psychological state, cultural background, and the specific circumstances of the injury or illness. However, certain conditions and injuries are widely considered to be among the most intensely painful experiences a human can endure. These often involve intense, prolonged nerve damage, inflammation, and/or the simultaneous activation of multiple pain pathways in the body. Conditions like cluster headaches and trigeminal neuralgia are often cited as contenders for the title of the "most excruciating pain," but even within those conditions, the experience varies greatly from person to person. It is important to remember that pain is a complex and personal experience.
Subjective Nature of Pain
Pain is a subjective experience, meaning it's entirely dependent on the individual's perception. There's no objective way to measure pain universally. What one person finds excruciating, another might find tolerable. This subjectivity makes comparing pain levels across individuals inherently difficult, if not impossible. Factors influencing pain perception include:
- Genetic predisposition: Some individuals are genetically more sensitive to pain than others.
- Psychological factors: Anxiety, depression, and stress can significantly amplify pain perception.
- Cultural background: Societal norms and learned behaviors influence how individuals express and interpret their pain.
Cluster Headaches
Cluster headaches are incredibly intense, described as a burning, searing, or piercing pain behind one eye. They typically occur in clusters, with multiple headaches occurring daily over a period of weeks or months, followed by periods of remission. These headaches are often accompanied by other symptoms, such as watering eyes, nasal congestion, and facial sweating. The intensity of the pain is frequently cited as being among the most severe known to humanity.
- Location: Primarily affecting one side of the head, often around the eye.
- Intensity: Described as excruciating, debilitating, and often unbearable.
- Duration: Attacks can last from 15 minutes to 3 hours, and cluster periods can last for weeks or months.
Trigeminal Neuralgia
Trigeminal neuralgia is a nerve disorder that affects the trigeminal nerve, which carries sensation from the face. It's characterized by sudden, severe, stabbing or burning facial pain that can last for seconds or minutes. Even minor stimuli, such as touching the face or brushing teeth, can trigger an attack. The intensity of the pain is often described as excruciating, and it can lead to significant disability.
- Cause: Often caused by compression of the trigeminal nerve, possibly by a blood vessel.
- Symptoms: Intense, sharp, shooting pains in the face, often unilateral (one-sided).
- Triggers: Everyday activities such as chewing, talking, or even a slight breeze can trigger attacks.
Cancer Pain
Pain associated with cancer can vary widely depending on the type and stage of cancer, the location of the tumor, and the presence of metastases. However, cancer pain can be incredibly intense and debilitating, particularly in advanced stages. It can stem from nerve compression, tissue damage, inflammation, and other factors. Managing cancer pain effectively is a crucial aspect of palliative care.
- Types: Can involve bone pain, nerve pain (neuropathic pain), visceral pain (organ pain), and soft tissue pain.
- Severity: Can range from mild discomfort to excruciating pain, often resistant to conventional analgesics.
- Management: Requires a multi-modal approach, often involving medication, radiation therapy, surgery, and other interventions.
Phantom Limb Pain
Phantom limb pain is a chronic pain experienced by amputees in the missing limb. Despite the absence of the limb, the brain continues to receive pain signals from the area where the limb used to be. The pain can be severe and debilitating, and its cause is not fully understood. It demonstrates how pain can be experienced even without a physical stimulus in the corresponding area.
- Mechanism: Likely involves reorganization of the nervous system after amputation.
- Symptoms: Can involve burning, aching, shooting, or stabbing pains in the missing limb.
- Treatment: Management often involves medication, physical therapy, and other interventions.
What is the most painful disorder?
There is no single answer to the question of what the most painful disorder is. Pain is a subjective experience, and what one person finds excruciating, another might tolerate better. Furthermore, different disorders cause different types of pain – sharp, dull, burning, aching, etc. – making direct comparisons difficult. However, several conditions are frequently cited as being among the most painful. These include conditions that cause neuropathic pain (damage to the nervous system), which is often described as burning, shooting, or stabbing pain that is difficult to treat. Also, conditions involving widespread inflammation and/or severe tissue damage are typically very painful.
Subjective Nature of Pain
The experience of pain is highly individual and influenced by a multitude of factors. These factors include psychological state, cultural background, and individual pain thresholds. What might be unbearable pain for one person could be manageable for another. Pain assessment scales are used, but they offer only a limited view of the true experience. There is no objective measure to determine the "most" painful disorder.
- Psychological factors: Anxiety, depression, and stress can significantly amplify pain perception.
- Cultural influences: Societal norms and learned responses to pain can influence how individuals report and experience pain.
- Genetic predisposition: An individual's genetic makeup can affect their pain sensitivity and response to treatment.
Cluster Headaches
Cluster headaches are severe, debilitating headaches that occur in clusters or groups. The pain is typically described as excruciating, intense, and often located around one eye. They can last from 15 minutes to 3 hours and are frequently accompanied by other symptoms, such as tearing, nasal congestion, and eyelid drooping. The intensity and frequency of cluster headaches make them a strong contender for one of the most painful conditions.
- Location: Often behind or around one eye.
- Intensity: Described as piercing or stabbing.
- Accompanying symptoms: Eye watering, nasal congestion, eyelid swelling.
Trigeminal Neuralgia
Trigeminal neuralgia, also known as tic douloureux, is a chronic pain condition affecting the trigeminal nerve, which carries sensation from the face to the brain. This condition causes episodes of intense, stabbing facial pain, described as electric shock-like sensations. The pain can be triggered by seemingly innocuous stimuli like touching the face or brushing teeth.
- Nerve affected: Trigeminal nerve, responsible for facial sensation.
- Pain description: Intense, sharp, shooting pain.
- Triggers: Often triggered by touching the face, chewing, or temperature changes.
Fibromyalgia
Fibromyalgia is a chronic widespread pain condition. It's characterized by widespread musculoskeletal pain accompanied by fatigue, sleep, memory and mood issues. While the pain isn't always as intensely sharp as in conditions like trigeminal neuralgia or cluster headaches, its chronic and pervasive nature makes it incredibly debilitating and painful for sufferers. The pain is often described as a deep, aching, burning, or throbbing sensation.
- Widespread pain: Affecting multiple areas of the body.
- Chronic nature: Lasting for months or years.
- Associated symptoms: Fatigue, sleep disturbances, cognitive difficulties.
Cancer Pain
Cancer pain can manifest in various ways and intensities depending on the type and location of cancer, the stage of the disease, and the presence of metastases. Pain may be due to tumor growth itself, nerve compression, or treatment-related side effects. The severity of cancer pain varies widely and can range from mild to excruciating, sometimes becoming intractable. It's worth noting that managing cancer pain is an important aspect of cancer care.
- Causes: Tumor growth, nerve compression, treatment side effects.
- Types of pain: Sharp, dull, aching, burning, or stabbing.
- Management: Requires a multidisciplinary approach including pain medication and supportive therapies.
What is considered the most painful chronic disease?
There isn't a single definitive answer to the question of what the "most painful" chronic disease is. Pain is a subjective experience, varying significantly from person to person based on factors like genetics, psychological state, coping mechanisms, and the specific characteristics of their disease. While some conditions are widely recognized for their severe pain potential, ranking them objectively is impossible. Studies attempting to quantify pain across different diseases often rely on self-reported pain scales, which are inherently limited. These scales don't account for the complex interplay of factors affecting an individual's perception and experience of pain. For example, a patient with fibromyalgia may experience widespread, debilitating pain, while a patient with trigeminal neuralgia may experience short, excruciating bursts of facial pain. Both conditions are devastating, but the nature and intensity of pain are vastly different, making direct comparison difficult. Furthermore, the severity of pain in any chronic condition is greatly impacted by the individual's overall health, their access to effective treatment and pain management strategies, and their emotional well-being. Therefore, focusing on the individual's experience of pain and providing tailored treatment approaches remains crucial.
Are there any chronic diseases consistently ranked high for pain levels?
Several chronic diseases are frequently cited as causing intense and persistent pain. Fibromyalgia is often highlighted, characterized by widespread musculoskeletal pain, fatigue, sleep disturbances, and cognitive issues. The pain associated with fibromyalgia is often described as chronic, deep, aching, and difficult to manage. Another condition often mentioned is complex regional pain syndrome (CRPS), a debilitating condition resulting from nerve damage that causes intense, spontaneous pain, often accompanied by swelling, changes in skin temperature and color, and limited mobility. Trigeminal neuralgia, a nerve disorder affecting the face, causes episodes of excruciating, sharp, stabbing pain. Osteoarthritis, a degenerative joint disease, is a major source of chronic pain for many individuals, particularly as it progresses. The level of pain experienced by patients with these conditions can vary significantly, depending on factors such as the disease's severity, individual sensitivity to pain, and access to appropriate medical care. Finally, cancer pain is a significant concern, varying greatly depending on the type of cancer and its location and stage. It is important to recognize that the ranking of these diseases in terms of pain is not universally agreed upon, and the subjective nature of pain must be kept in mind.
How is pain managed in these highly painful chronic diseases?
Pain management in chronic diseases is a complex and multifaceted process that often involves a combination of approaches. Pharmacological interventions, including analgesics (such as opioids, NSAIDs, and acetaminophen), antidepressants, and anticonvulsants, may play a significant role. However, the use of opioids, in particular, is often carefully considered due to concerns about addiction and side effects. Non-pharmacological methods are also critical and often used in conjunction with medication. These include physical therapy, occupational therapy, cognitive behavioral therapy (CBT), and mindfulness-based stress reduction techniques. Physical therapy helps improve mobility, strength, and flexibility, reducing pain and improving function. Occupational therapy helps patients adapt their daily activities to manage pain and maintain independence. CBT helps individuals develop coping mechanisms for managing pain and improving their overall well-being. Mindfulness practices can help individuals reduce stress and improve their ability to cope with chronic pain. Interventional pain management techniques, such as nerve blocks or spinal cord stimulation, may be used in cases of severe, intractable pain that doesn't respond to other treatments. The specific management strategy for each individual will depend on the nature of their condition, the severity of their pain, and their overall health status. A holistic approach, involving a team of healthcare professionals, is often the most effective way to manage chronic pain.
What research is being done to better understand and treat chronic pain?
Significant research efforts are underway to better understand and treat chronic pain. Researchers are exploring the neurobiological mechanisms underlying chronic pain, investigating the complex interactions between the nervous system, immune system, and psychological factors that contribute to the development and maintenance of chronic pain conditions. Advances in neuroimaging techniques are providing new insights into brain activity and changes in brain structure associated with chronic pain. This research is helping identify potential targets for new pain therapies. Scientists are also working on developing novel analgesic drugs with improved efficacy and fewer side effects. This includes research into non-opioid analgesics, targeting specific pain pathways in the nervous system, and exploring the potential of gene therapy. Furthermore, research into non-pharmacological treatments is expanding, with studies investigating the effectiveness of different types of physical therapy, mental health interventions, and lifestyle modifications in managing chronic pain. Ultimately, the goal of this research is to develop more effective, personalized treatments that can improve the lives of individuals living with chronic pain, reducing their suffering and improving their quality of life. This field is dynamic, and significant progress is being made each year.
Deja una respuesta