What do stress mouth sores look like

Stress can manifest itself physically in a variety of ways, including through the development of mouth sores. These sores can be painful and uncomfortable, making it difficult to eat and communicate. Understanding what stress mouth sores look like is essential for early diagnosis and treatment. In this article, we will explore the various types of stress mouth sores, their typical appearance, and the underlying causes associated with them.
What Do Stress-Induced Mouth Sores Look Like?
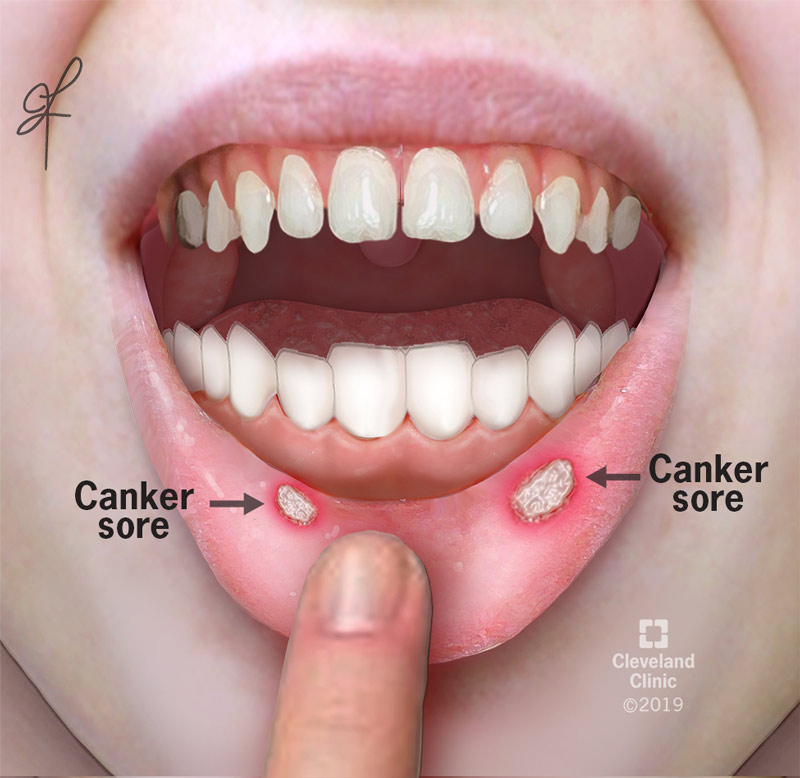
Stress can manifest in many ways, and one often overlooked symptom is the appearance of mouth sores, also known as aphthous ulcers or canker sores. While not all mouth sores are stress-related, stress can certainly exacerbate their development and worsen their symptoms. Stress-induced mouth sores typically present similarly to other types of canker sores, but their appearance might be linked to a more frequent occurrence or prolonged healing time due to the ongoing stress.
Size and Shape of Stress-Induced Mouth Sores
Stress-induced mouth sores generally appear as small, round or oval lesions. They can range in size from a few millimeters to a centimeter or more in diameter, depending on the severity of the stress and individual susceptibility. Their shape isn't always perfectly uniform; some might be irregular, and larger sores may have an uneven edge. The sores are typically shallow, unlike cold sores which are often more blister-like.
Color of Stress-Induced Mouth Sores
The color of a stress-induced mouth sore will typically be pale yellow or whitish-gray in the center, surrounded by a reddish halo. This red ring indicates inflammation. As the sore heals, the center may become slightly darker or yellowish-brown before eventually fading. The color can vary slightly depending on the stage of healing and the individual's overall health.
Location of Stress-Induced Mouth Sores
Unlike cold sores (caused by the herpes simplex virus), which usually appear on the outer lip, stress-induced mouth sores most commonly develop on the inside of the cheeks, lips, gums, and the underside of the tongue. They rarely appear on the hard palate (roof of the mouth). Their location is not diagnostic of stress as a causative factor, but it aligns with the typical location of canker sores.
Pain and Discomfort Associated with Stress-Induced Mouth Sores
A key characteristic of stress-induced mouth sores is the pain and discomfort they cause. This can range from mild burning or tingling to severe pain, especially when eating, drinking, or speaking. The pain level is often directly proportional to the size and number of sores present. The discomfort can significantly affect daily activities and contribute to overall stress levels, creating a vicious cycle.
Healing Time of Stress-Induced Mouth Sores
While the healing time for mouth sores varies, those triggered or worsened by stress may take longer to heal compared to sores caused by other factors. This extended healing time is often due to the body's impaired ability to repair tissues effectively under the influence of chronic stress. While most minor canker sores heal within 1-2 weeks, those exacerbated by stress can persist for a much longer duration. Reducing stress levels can greatly contribute to faster healing.
| Characteristic | Description |
|---|---|
| Appearance | Small, round or oval lesions; pale yellow or whitish-gray center; reddish halo; irregular shape possible. |
| Location | Inside of cheeks, lips, gums, underside of tongue. |
| Pain | Mild burning to severe pain; exacerbated by eating, drinking, and speaking. |
| Healing Time | Potentially longer healing time than non-stress-related sores. |
| Causation | Stress can exacerbate existing susceptibility or trigger new occurrences. |
What Do Stress-Induced Mouth Sores Look Like?
Stress can manifest in many ways, and one often overlooked symptom is the appearance of mouth sores, also known as aphthous ulcers or canker sores. While not all mouth sores are stress-related, stress can certainly exacerbate their development and worsen their symptoms. Stress-induced mouth sores typically present similarly to other types of canker sores, but their appearance might be linked to a more frequent occurrence or prolonged healing time due to the ongoing stress.
Size and Shape of Stress-Induced Mouth Sores
Stress-induced mouth sores generally appear as small, round or oval lesions. They can range in size from a few millimeters to a centimeter or more in diameter, depending on the severity of the stress and individual susceptibility. Their shape isn't always perfectly uniform; some might be irregular, and larger sores may have an uneven edge. The sores are typically shallow, unlike cold sores which are often more blister-like.
Color of Stress-Induced Mouth Sores
The color of a stress-induced mouth sore will typically be pale yellow or whitish-gray in the center, surrounded by a reddish halo. This red ring indicates inflammation. As the sore heals, the center may become slightly darker or yellowish-brown before eventually fading. The color can vary slightly depending on the stage of healing and the individual's overall health.
Location of Stress-Induced Mouth Sores
Unlike cold sores (caused by the herpes simplex virus), which usually appear on the outer lip, stress-induced mouth sores most commonly develop on the inside of the cheeks, lips, gums, and the underside of the tongue. They rarely appear on the hard palate (roof of the mouth). Their location is not diagnostic of stress as a causative factor, but it aligns with the typical location of canker sores.
Pain and Discomfort Associated with Stress-Induced Mouth Sores
A key characteristic of stress-induced mouth sores is the pain and discomfort they cause. This can range from mild burning or tingling to severe pain, especially when eating, drinking, or speaking. The pain level is often directly proportional to the size and number of sores present. The discomfort can significantly affect daily activities and contribute to overall stress levels, creating a vicious cycle.
Healing Time of Stress-Induced Mouth Sores
While the healing time for mouth sores varies, those triggered or worsened by stress may take longer to heal compared to sores caused by other factors. This extended healing time is often due to the body's impaired ability to repair tissues effectively under the influence of chronic stress. While most minor canker sores heal within 1-2 weeks, those exacerbated by stress can persist for a much longer duration. Reducing stress levels can greatly contribute to faster healing.
| Characteristic | Description |
|---|---|
| Appearance | Small, round or oval lesions; pale yellow or whitish-gray center; reddish halo; irregular shape possible. |
| Location | Inside of cheeks, lips, gums, underside of tongue. |
| Pain | Mild burning to severe pain; exacerbated by eating, drinking, and speaking. |
| Healing Time | Potentially longer healing time than non-stress-related sores. |
| Causation | Stress can exacerbate existing susceptibility or trigger new occurrences. |
How long do stress mouth sores last?
The duration of stress-induced mouth sores, also known as aphthous ulcers or canker sores, is variable and depends on several factors. Generally, minor aphthous ulcers, the most common type, typically heal within 7 to 10 days without any specific treatment. However, some can persist for up to three weeks. Major aphthous ulcers, which are larger and deeper, can take several weeks or even months to heal completely. The size, location, and individual's immune response all play a role in healing time.
What Factors Influence Healing Time?
Several factors influence how quickly a stress-induced mouth sore heals. These include the severity of the ulcer, your overall health, and your body's natural healing processes. Stress levels themselves can prolong healing, as prolonged stress weakens the immune system. Furthermore, nutritional deficiencies, particularly in iron, vitamin B12, and folic acid, can hinder healing. Finally, the presence of underlying medical conditions or medications can also influence recovery time.
- Severity of the ulcer: Minor sores heal faster than major ones.
- Immune system strength: A strong immune system promotes faster healing.
- Nutritional status: Deficiencies can delay healing.
How to Differentiate Between Stress-Induced and Other Mouth Sores?
While stress can exacerbate canker sores, it's crucial to differentiate them from other mouth sores. Canker sores are typically small, shallow ulcers with a yellowish base and a reddish border. They usually appear inside the mouth, on the cheeks, gums, or tongue. In contrast, cold sores (caused by the herpes simplex virus) appear on the lips and are characterized by blisters that eventually crust over. Other mouth sores might indicate infections or other medical conditions requiring professional medical attention. If unsure, consult a healthcare professional for proper diagnosis.
- Location: Canker sores are inside the mouth; cold sores are on the lips.
- Appearance: Canker sores are shallow ulcers; cold sores are blisters that crust.
- Causative agent: Canker sores are not contagious; cold sores are caused by a virus.
When to See a Doctor About a Stress-Induced Mouth Sore?
Most stress-induced mouth sores heal on their own, but there are instances when seeking medical attention is necessary. If a sore lasts longer than three weeks, is exceptionally painful, unusually large, or bleeds excessively, a doctor should be consulted. Additionally, if you experience frequent recurring sores, it's vital to seek professional evaluation to rule out underlying medical conditions or nutritional deficiencies. A doctor can provide proper diagnosis and recommend appropriate treatment if needed.
- Prolonged duration (over 3 weeks): This warrants medical attention.
- Severe pain or bleeding: These indicate a more serious issue.
- Frequent recurrences: This may indicate an underlying problem.
Home Remedies for Faster Healing of Stress Mouth Sores
While medical attention is sometimes necessary, several home remedies can help alleviate pain and promote faster healing of stress-induced mouth sores. Rinsing the mouth with warm salt water several times a day can help clean the area and reduce inflammation. Applying a topical anesthetic gel can provide temporary pain relief. Maintaining good oral hygiene, including regular brushing and flossing, is also crucial to prevent infection. Ensuring adequate hydration and a balanced diet, rich in vitamins and minerals, can support the body's natural healing processes.
- Salt water rinses: Reduce inflammation and clean the sore.
- Topical anesthetic gels: Provide temporary pain relief.
- Good oral hygiene: Prevents infection and promotes healing.
The Role of Stress Management in Preventing Mouth Sores
Since stress can exacerbate or even trigger canker sores, implementing effective stress management techniques is vital in preventing their recurrence. Regular exercise, sufficient sleep, and mindfulness practices, such as meditation or yoga, can help reduce stress levels. Lifestyle changes like incorporating relaxation techniques into daily routines can also have a positive impact. Addressing underlying sources of stress through counselling or other therapeutic interventions can lead to long-term improvement and reduced frequency of mouth sores.
- Exercise: Reduces stress hormones.
- Sleep: Allows the body to repair and rejuvenate.
- Mindfulness practices: Help manage stress levels.
Why am I suddenly getting blisters in my mouth?

Sudden blisters in your mouth can be caused by a variety of factors, and pinpointing the exact cause often requires a visit to a doctor or dentist. Several conditions can lead to oral blisters, ranging from relatively minor irritations to more serious viral infections. The sudden onset suggests a recent trigger, which could be anything from a new food or toothpaste to a viral infection or a reaction to medication. The size, location, and accompanying symptoms (such as fever, pain, or difficulty swallowing) will all help in determining the underlying cause. It's crucial to seek professional medical advice if the blisters are severe, persistent, painful, or accompanied by other concerning symptoms.
Possible Viral Infections
Many viral infections can manifest as oral blisters. Herpes simplex virus (HSV), for example, is a common culprit behind cold sores or fever blisters, typically appearing on the lips but sometimes inside the mouth. Other viral infections like hand, foot, and mouth disease (HFMD) can also cause painful mouth blisters. These viral infections are often contagious and can spread through contact with saliva or infected surfaces.
- Herpes simplex virus (HSV): Causes cold sores, often preceded by tingling or burning. Can recur in the same location.
- Hand, foot, and mouth disease (HFMD): Causes small, painful blisters in the mouth, hands, and feet; often accompanied by fever.
- Other viral infections: Various other viruses can cause similar symptoms; a doctor can help determine the specific virus.
Allergic Reactions
An allergic reaction to a food, medication, or even toothpaste can trigger oral blisters. These reactions can manifest as a sudden onset of painful blisters, often accompanied by other symptoms like itching, swelling, or difficulty breathing (in severe cases). Identifying the allergen is crucial to prevent future occurrences, and this might require allergy testing.
- Food allergies: Reactions to certain foods can cause oral blisters, along with other symptoms like hives or gastrointestinal distress.
- Medication allergies: Some medications can cause an allergic reaction in the mouth, manifesting as blisters or other oral lesions.
- Oral hygiene products: Toothpaste, mouthwash, or other dental products can sometimes cause allergic reactions.
Physical Trauma
Accidental injury to the mouth, such as biting your cheek, tongue, or lip, can result in blisters. These injuries usually heal within a few days without complications. However, if the injury is severe or becomes infected, medical attention might be necessary.
- Biting the inside of your cheek or lip: A common cause of minor mouth blisters that usually heal quickly.
- Dental work: Procedures like extractions or dental appliances can sometimes cause minor trauma leading to blisters.
- Burns: Hot foods or drinks can burn the mouth, leading to blisters.
Autoimmune Diseases
Certain autoimmune diseases, like pemphigus vulgaris or pemphigoid, can cause oral blisters as part of a wider range of symptoms. These conditions cause the body's immune system to attack healthy skin and mucous membranes, resulting in blisters that can be painful and difficult to heal. Diagnosis requires specialized medical testing.
- Pemphigus vulgaris: A rare autoimmune disease characterized by painful blisters in the mouth and on the skin.
- Pemphigoid: Another autoimmune disease that can cause similar symptoms to pemphigus vulgaris.
- Other autoimmune diseases: Several other less common autoimmune disorders can involve oral blisters as a symptom.
Other Less Common Causes
Beyond the more common causes, there are other, less frequent possibilities. Certain medications, nutritional deficiencies, or underlying medical conditions can sometimes contribute to the development of oral blisters. A thorough medical evaluation may be needed to explore these less likely scenarios.
- Certain medications: Some medications have side effects that can include oral blisters.
- Nutritional deficiencies: Deficiencies in certain vitamins or minerals might contribute to oral health problems.
- Underlying medical conditions: Rarely, underlying health issues can manifest as oral blisters.
What do autoimmune mouth sores look like?

Autoimmune mouth sores, often associated with conditions like Behçet's disease, lupus, or Crohn's disease, can vary significantly in appearance depending on the underlying condition and its severity. They aren't easily distinguishable from other types of mouth sores without a proper medical diagnosis. However, some common characteristics may include:
Appearance of Autoimmune Mouth Sores
Autoimmune mouth sores can manifest as painful ulcers, ranging in size from tiny spots to large, deep lesions. They may be single or multiple, appearing anywhere in the mouth – on the tongue, gums, inside the cheeks, or on the lips. Unlike canker sores, they may not always be round or oval and can have irregular shapes and borders. The color can also vary, ranging from yellowish-white to reddish or grayish, often with a red halo surrounding the sore. The sores might also be accompanied by swelling and inflammation of the surrounding tissue.
- Painful ulcers: A key characteristic often more severe than simple canker sores.
- Variable size and shape: Unlike typical canker sores, size and shape are less predictable.
- Multiple lesions: Often more than one sore is present.
Behçet's Disease Mouth Sores
In Behçet's disease, mouth sores are a hallmark symptom. These ulcers are typically deep, painful, and can be quite large. They often appear on the gums and the inner lining of the mouth. These sores may heal and then reappear, representing a chronic and recurring pattern. They often persist for several days to weeks, sometimes resulting in scarring. Diagnosing Behçet's requires multiple symptoms, and mouth sores are one piece of the puzzle.
- Large and deep ulcers: Often more significant than those associated with other conditions.
- Recurrent nature: They frequently heal and reappear.
- Gum involvement: Gums are a common site for these ulcers.
Lupus Mouth Sores
Mouth sores in lupus are often linked to oral manifestations of the disease. They might appear as small, painful ulcers similar to canker sores, but can also be more severe and occur in clusters. These sores can be accompanied by other symptoms of lupus, such as facial rash (malar rash), fatigue, and joint pain. A physician's diagnosis is crucial because oral lesions in lupus can be less prominent and easily misidentified.
- Painful sores: Often present, ranging in severity.
- Possible association with other lupus symptoms: Appearance often correlates with other signs of lupus.
- Diagnosis requires comprehensive evaluation: Oral lesions alone aren't sufficient for diagnosis.
Crohn's Disease Mouth Sores
In Crohn's disease, mouth sores can be a less common symptom compared to gastrointestinal involvement. They usually appear as aphthous ulcers (canker sores) that are small, shallow, and painful. These ulcers may be accompanied by other Crohn's symptoms like abdominal pain, diarrhea, and weight loss. These sores are typically treated in the context of managing Crohn's disease, rather than as an isolated issue.
- Aphthous ulcers: Resemble typical canker sores.
- Often part of a broader Crohn's symptom presentation: Often not the primary diagnostic indicator.
- Treatment focuses on Crohn's disease management: Treatment is secondary to managing the overall condition.
Other Autoimmune Diseases and Mouth Sores
Several other autoimmune conditions can lead to mouth sores. The appearance of these sores can vary considerably and often mirrors characteristics of the conditions mentioned above – painful ulcers, different sizes and locations, recurrent nature. Precise diagnosis requires a thorough medical examination and potentially further testing to identify the underlying autoimmune disorder. It’s crucial to seek professional medical advice for persistent or unusual mouth sores.
- Variety of presentations: Appearance significantly varies depending on the specific autoimmune disease.
- Requires medical evaluation: Proper diagnosis needs a doctor's assessment.
- Treatment depends on underlying condition: Treatment focuses on managing the specific autoimmune disease.
What are the symptoms of stress in the mouth?

Temporomandibular Joint (TMJ) Disorders
Stress can significantly exacerbate temporomandibular joint (TMJ) disorders. The TMJ connects your jaw to your skull, and when you're stressed, you might unconsciously clench or grind your teeth (bruxism), putting immense pressure on this joint. This can lead to a range of symptoms, impacting your jaw's functionality and comfort.
- Jaw pain and tenderness: Pain can radiate to the temples, ears, or neck.
- Limited jaw movement: Difficulty opening your mouth wide or chewing.
- Clicking or popping sounds in the jaw: Noticed when opening or closing your mouth.
Oral Lesions and Canker Sores
Stress is a known trigger for oral lesions and recurrent canker sores (aphthous ulcers). These painful sores typically appear inside the mouth on the cheeks, tongue, or gums. The exact mechanism isn't fully understood, but stress hormones likely play a role in weakening the immune system, making individuals more susceptible to these lesions.
- Small, shallow ulcers with a yellowish-white base: Often surrounded by a red halo.
- Burning or tingling sensation before the sore appears: A precursor to the lesion developing.
- Pain and discomfort while eating, drinking, or talking: The sores can be quite sensitive.
Dry Mouth (Xerostomia)
Stress can reduce saliva production, leading to dry mouth (xerostomia). Saliva is essential for oral health, as it lubricates the mouth, neutralizes acids, and contains antimicrobial properties. Reduced saliva flow can increase the risk of cavities, gum disease, and other oral infections.
- Persistent feeling of dryness in the mouth: Making it difficult to swallow or speak.
- Sticky or thick saliva: A change in the consistency of saliva.
- Increased thirst: A compensatory response to the dryness.
Bruxism (Teeth Grinding)
Bruxism, or teeth grinding, is a common manifestation of stress. It often occurs unconsciously, particularly during sleep, and can lead to significant wear and tear on the teeth. The constant friction can result in various dental problems.
- Tooth sensitivity: Increased pain when consuming hot or cold foods.
- Flattened or chipped teeth: Visible signs of wear and tear.
- Jaw pain and headaches: Due to the constant pressure on the jaw muscles.
Changes in Taste and Appetite
Stress can impact the sense of taste and appetite, indirectly affecting oral health. Changes in food intake can lead to decreased saliva production, increased sugar consumption (increasing cavity risk), or neglect of oral hygiene practices. Alterations in taste perception can also occur, leading to food aversions or changes in dietary habits.
- Loss of appetite or overeating: Stress can lead to both extremes.
- Changes in taste preference: Certain foods might taste different or less appealing.
- Difficulty swallowing: Due to stress-induced changes in the muscles involved in swallowing.
What exactly are stress mouth sores?
Stress mouth sores, also known as aphthous ulcers or canker sores, are small, shallow lesions that develop inside the mouth. While stress can be a trigger for their appearance, it's important to understand that they aren't directly caused by stress. Instead, stress acts as a contributing factor that can exacerbate the underlying conditions that lead to their formation. These conditions often include a weakened immune system, hormonal fluctuations, or even minor injuries to the mouth's lining. The sores themselves are typically characterized by a painful, whitish-yellow center surrounded by a red border. They can vary in size, ranging from a few millimeters to a centimeter in diameter. Importantly, stress mouth sores are different from cold sores (fever blisters), which are caused by the herpes simplex virus and appear on the outside of the lips. While the appearance might seem similar at a glance, the underlying causes and locations distinctly differentiate them. The key takeaway is that while stress can influence their frequency and severity, it is not the sole or direct cause of these common oral lesions.
How can I tell the difference between a stress mouth sore and something else?
Differentiating stress mouth sores from other oral lesions can be crucial for proper treatment. Location is a primary indicator. Stress mouth sores typically appear on the inner lining of the cheeks, lips, gums, or the base of the tongue. They rarely appear on the outside of the lips or the vermilion border (the lip's red area), which is a key characteristic of cold sores. The appearance is also distinctive. Stress mouth sores usually have a round or oval shape with a pale yellowish-white center and a distinctly red, inflamed border. They are typically shallow and not accompanied by fever blisters or other systemic symptoms. Other oral conditions, such as oral thrush (a fungal infection), exhibit a different appearance and often present with a more widespread, white coating on the mouth's surface. Similarly, oral cancer sores may be harder to distinguish but typically present as persistent, non-healing ulcers that may bleed easily. If you're unsure about the nature of an oral lesion, it is vital to consult a dentist or doctor for a proper diagnosis and to rule out more serious conditions. Self-treating can delay appropriate medical intervention.
What makes stress sores appear more often when I'm stressed?
The link between stress and the frequency of stress mouth sores is multifaceted and not fully understood. However, several theories exist. Stress weakens the immune system. This compromised immune response makes the body less effective at fighting off minor infections or irritations within the mouth. A minor injury, such as a bite or irritation from food, may be enough to trigger a sore when the immune system is already stressed. Secondly, stress affects hormonal balance. Hormonal fluctuations can impact the body's inflammatory response, making individuals more susceptible to developing aphthous ulcers. Stress also often leads to changes in sleep patterns and diet, which can further compromise the immune system and overall oral health. Poor sleep and nutrition create an environment that is conducive to the development of mouth sores. Finally, stress can lead to poor oral hygiene practices. When stressed, individuals might neglect proper brushing and flossing, contributing to the formation of sores. While stress itself isn't the direct cause, it undeniably creates a cascade of factors that increase the likelihood of developing or experiencing more frequent stress mouth sores.
When should I see a doctor about a stress mouth sore?
While most stress mouth sores heal on their own within a couple of weeks, there are situations requiring professional medical attention. Persistent sores that don't heal within two to three weeks should be evaluated by a dentist or doctor. This is crucial to rule out other underlying conditions. Large or unusually painful sores, those that are unusually numerous or widespread, are also cause for concern. If the sores are accompanied by other symptoms, such as fever, swollen lymph nodes, or difficulty swallowing, immediate medical attention is necessary. Moreover, if the sores appear to be bleeding excessively or exhibit unusual characteristics, a professional examination is essential. Recurrent outbreaks of stress sores, despite managing stress levels, warrant a consultation to explore potential underlying medical issues or dietary deficiencies. Don't hesitate to seek professional help if you are worried about the appearance, size, or persistence of your mouth sores. Early diagnosis and treatment can prevent potential complications and ensure optimal oral health.
Deja una respuesta