How to relieve a mouth ulcer

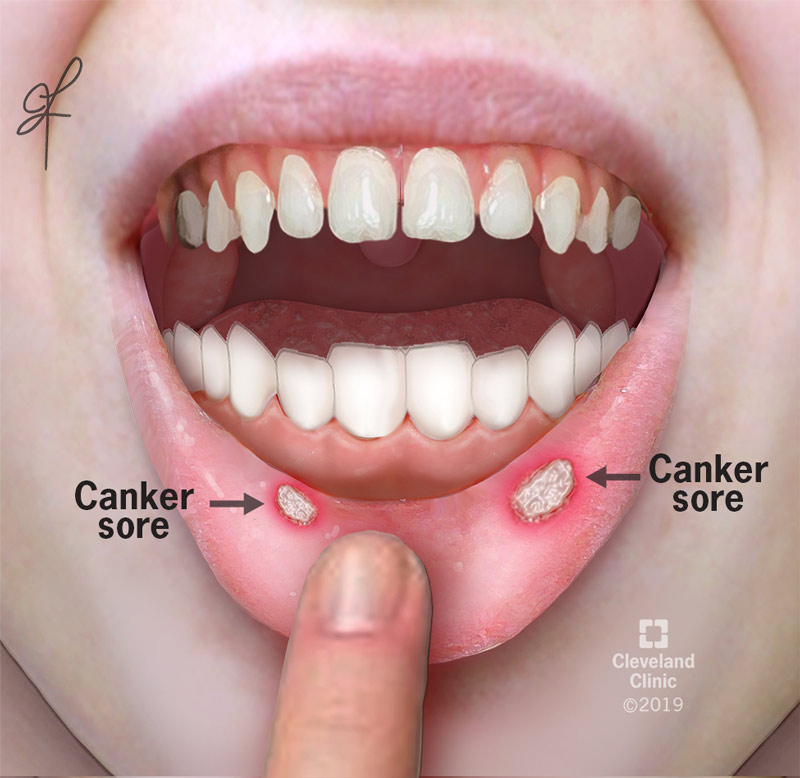
Mouth ulcers, also known as canker sores, are common and painful sores that can develop inside the mouth. They can be caused by a variety of factors, including stress, hormonal changes, vitamin deficiencies, and certain medications. While mouth ulcers are usually not serious, they can be very uncomfortable and interfere with eating, drinking, and talking. Fortunately, there are a number of things that can be done to relieve the pain and discomfort of mouth ulcers. In this article, we will discuss some of the most effective ways to relieve a mouth ulcer.
How to Soothe and Heal a Mouth Ulcer
Mouth ulcers, also known as aphthous ulcers or canker sores, are small, painful sores that develop inside the mouth. While they typically heal on their own within a week or two, there are several things you can do to relieve the discomfort and speed up the healing process. The key is to be gentle and avoid anything that could irritate the sore further.
Saltwater Rinse
Rinsing your mouth with warm salt water is a simple yet effective home remedy. Salt has natural antiseptic properties that can help reduce inflammation and kill bacteria, preventing infection. Dissolve ½ to ¾ teaspoon of salt in a glass of warm water and gently swish it around your mouth for 30-60 seconds, then spit it out. Repeat this several times a day, especially after meals.
Over-the-Counter Medications
Numerous over-the-counter (OTC) medications can provide relief from mouth ulcer pain. These include oral analgesics like benzocaine or lidocaine, which numb the area. You can also find topical ointments or gels containing corticosteroids that help reduce inflammation. Always follow the instructions on the packaging carefully and consult a doctor or pharmacist if you have any questions or concerns. Avoid products containing alcohol or hydrogen peroxide, as these can irritate the sore.
Dietary Adjustments
Certain foods and drinks can exacerbate mouth ulcers. Avoid acidic foods and drinks like citrus fruits, tomatoes, and spicy foods. Minimizing the consumption of caffeine and alcohol can also be beneficial, as they can further dehydrate the mouth and irritate the sore. Instead, focus on soft, bland foods that are easy to chew and swallow, such as mashed potatoes, yogurt, and oatmeal. Staying well-hydrated is also crucial for healing.
Maintaining Good Oral Hygiene
Practicing good oral hygiene is essential for preventing infection and promoting healing. Brush your teeth gently with a soft-bristled toothbrush, being careful not to irritate the ulcer. Flossing is also important but avoid flossing directly on the ulcer. Use a fluoride-based toothpaste. Rinsing with a fluoride mouthwash can also help strengthen tooth enamel and aid in healing.
When to See a Doctor
Most mouth ulcers heal on their own within a couple of weeks. However, it's important to consult a doctor or dentist if: the ulcer is unusually large or painful; it lasts longer than two weeks; you experience recurring ulcers frequently; you have a fever or other signs of infection; or you have difficulty swallowing or eating. Your doctor can determine the underlying cause and recommend appropriate treatment.
| Remedy | Benefits | Cautions |
|---|---|---|
| Saltwater Rinse | Reduces inflammation, kills bacteria | May sting initially |
| OTC Medications (Benzocaine/Lidocaine) | Numbs pain | May cause allergic reactions; follow instructions carefully |
| Dietary Changes (Bland Foods) | Avoids irritation, promotes healing | Requires careful meal planning |
| Gentle Oral Hygiene | Prevents infection, promotes healing | Avoid harsh brushing near the ulcer |
| Medical Consultation | Diagnosis and treatment of underlying causes | Necessary for persistent or severe ulcers |
How to Soothe and Heal a Mouth Ulcer
Mouth ulcers, also known as aphthous ulcers or canker sores, are small, painful sores that develop inside the mouth. While they typically heal on their own within a week or two, there are several things you can do to relieve the discomfort and speed up the healing process. The key is to be gentle and avoid anything that could irritate the sore further.
Saltwater Rinse
Rinsing your mouth with warm salt water is a simple yet effective home remedy. Salt has natural antiseptic properties that can help reduce inflammation and kill bacteria, preventing infection. Dissolve ½ to ¾ teaspoon of salt in a glass of warm water and gently swish it around your mouth for 30-60 seconds, then spit it out. Repeat this several times a day, especially after meals.
Over-the-Counter Medications
Numerous over-the-counter (OTC) medications can provide relief from mouth ulcer pain. These include oral analgesics like benzocaine or lidocaine, which numb the area. You can also find topical ointments or gels containing corticosteroids that help reduce inflammation. Always follow the instructions on the packaging carefully and consult a doctor or pharmacist if you have any questions or concerns. Avoid products containing alcohol or hydrogen peroxide, as these can irritate the sore.
Dietary Adjustments
Certain foods and drinks can exacerbate mouth ulcers. Avoid acidic foods and drinks like citrus fruits, tomatoes, and spicy foods. Minimizing the consumption of caffeine and alcohol can also be beneficial, as they can further dehydrate the mouth and irritate the sore. Instead, focus on soft, bland foods that are easy to chew and swallow, such as mashed potatoes, yogurt, and oatmeal. Staying well-hydrated is also crucial for healing.
Maintaining Good Oral Hygiene
Practicing good oral hygiene is essential for preventing infection and promoting healing. Brush your teeth gently with a soft-bristled toothbrush, being careful not to irritate the ulcer. Flossing is also important but avoid flossing directly on the ulcer. Use a fluoride-based toothpaste. Rinsing with a fluoride mouthwash can also help strengthen tooth enamel and aid in healing.
When to See a Doctor
Most mouth ulcers heal on their own within a couple of weeks. However, it's important to consult a doctor or dentist if: the ulcer is unusually large or painful; it lasts longer than two weeks; you experience recurring ulcers frequently; you have a fever or other signs of infection; or you have difficulty swallowing or eating. Your doctor can determine the underlying cause and recommend appropriate treatment.
| Remedy | Benefits | Cautions |
|---|---|---|
| Saltwater Rinse | Reduces inflammation, kills bacteria | May sting initially |
| OTC Medications (Benzocaine/Lidocaine) | Numbs pain | May cause allergic reactions; follow instructions carefully |
| Dietary Changes (Bland Foods) | Avoids irritation, promotes healing | Requires careful meal planning |
| Gentle Oral Hygiene | Prevents infection, promotes healing | Avoid harsh brushing near the ulcer |
| Medical Consultation | Diagnosis and treatment of underlying causes | Necessary for persistent or severe ulcers |
What makes ulcers in your mouth go away?
What Makes Mouth Ulcers Go Away?
Mouth ulcers, also known as aphthous ulcers or canker sores, are small, shallow lesions that develop on the soft tissues inside the mouth. They are usually quite painful and can take anywhere from a few days to several weeks to heal. While there's no single cure, several factors contribute to their resolution, and several approaches can speed up the healing process. The body's natural healing mechanisms are primarily responsible for their eventual disappearance. This involves the inflammatory response, where the body works to repair the damaged tissue. However, various treatments can support this process.
1. The Body's Natural Healing Process
Your body's immune system plays a crucial role in healing mouth ulcers. The inflammatory response, characterized by redness, swelling, and pain, is a vital part of this process. White blood cells rush to the affected area to fight off any infection and begin the repair of damaged tissue. This process, while sometimes uncomfortable, is essential for the ulcer to eventually heal. Over time, the ulcer will gradually shrink, the pain will lessen, and the area will re-epithelialize (form new skin). This natural healing typically takes between 7 to 10 days, but can vary depending on the size and severity of the ulcer.
- Inflammation: The body's initial response, bringing white blood cells to fight infection and begin tissue repair.
- Tissue Repair: Damaged cells are replaced with new ones, gradually filling in the ulcer.
- Epithelialization: New skin cells form over the healed area, completing the repair process.
2. Over-the-Counter Treatments
Several over-the-counter (OTC) medications can help manage the symptoms and potentially speed up the healing process of mouth ulcers. These often provide temporary pain relief and create a protective barrier over the ulcer. Many OTC treatments contain analgesics (pain relievers) like benzocaine or lidocaine to numb the area. Others offer protective coatings to prevent irritation and promote faster healing. Always follow the instructions on the packaging and consult a healthcare professional if symptoms persist or worsen.
- Analgesic gels or sprays: Numb the area, providing pain relief.
- Protective mouth rinses: Create a protective barrier and reduce irritation.
- Topical corticosteroids: (Some OTC options available) Reduce inflammation and may speed healing.
3. Home Remedies
Various home remedies can provide relief from the pain and discomfort of mouth ulcers. While not scientifically proven to significantly reduce healing time, they can offer comfort and support the healing process. Rinsing your mouth with warm salt water is a common and often effective remedy, as it helps to clean the area and reduce inflammation. Other remedies include applying a small amount of honey, which has antibacterial and anti-inflammatory properties, or using aloe vera gel, which soothes the affected tissue.
- Saltwater rinses: Clean the area and reduce inflammation.
- Honey application: Provides antibacterial and anti-inflammatory benefits.
- Aloe vera gel: Soothes the ulcer and may promote healing.
4. Dietary Changes
Certain foods and drinks can irritate mouth ulcers and prolong healing time. Avoiding acidic, spicy, or very hot foods and drinks is crucial. Similarly, hard or crunchy foods can cause further trauma to the already sensitive area. Maintaining good oral hygiene, by brushing and flossing gently, can help prevent infection and promote healing. A balanced diet, rich in essential nutrients, supports the body's natural healing processes.
- Avoid irritants: Acidic, spicy, and hot foods should be avoided.
- Gentle oral hygiene: Brush and floss carefully to prevent further irritation.
- Nutrient-rich diet: Supports the body's natural healing mechanisms.
5. Underlying Medical Conditions
In some cases, recurring or severe mouth ulcers may indicate an underlying medical condition, such as vitamin deficiencies (especially B12 and iron), immune system disorders, or inflammatory bowel disease (IBD). If you experience frequent or unusually severe mouth ulcers, it's important to consult a doctor or dentist to rule out any underlying health issues. They can perform tests and recommend appropriate treatment if necessary.
- Vitamin deficiencies: B12 and iron deficiencies can contribute to mouth ulcers.
- Immune system disorders: Certain conditions can weaken the immune system, making ulcers more likely.
- Inflammatory bowel disease (IBD): IBD can manifest with mouth ulcers as a symptom.
How to stop an ulcer from hurting?
:max_bytes(150000):strip_icc()/VWH_Illustration_Natural-Remedies-for-Stomach-Ulcers_Danie-Drankwalter_Final-53fe423966274ed0930616388c3d0c9d.jpg)
How to Stop an Ulcer From Hurting?
Stopping ulcer pain requires a multi-pronged approach focusing on healing the ulcer and managing symptoms. It's crucial to understand that home remedies alone might not suffice, and professional medical attention is essential for diagnosis and treatment. Ignoring ulcer pain can lead to serious complications. The following strategies can help alleviate pain while you seek medical advice.
1. Medication
Your doctor will likely prescribe medications to address the underlying cause of your ulcer and relieve pain. This commonly includes:
- Antacids: These neutralize stomach acid, providing immediate relief from burning sensations. They're often available over-the-counter but should be used as directed.
- H2 blockers: These reduce stomach acid production, offering longer-lasting relief than antacids. Examples include ranitidine and famotidine.
- Proton pump inhibitors (PPIs): These are stronger acid reducers, suppressing acid production more effectively than H2 blockers. Omeprazole and pantoprazole are examples.
- Antibiotics: If your ulcer is caused by H. pylori bacteria, your doctor will prescribe antibiotics to eradicate the infection.
- Pain relievers: Over-the-counter pain relievers like ibuprofen or acetaminophen can help manage pain, but shouldn't replace prescribed ulcer medication.
2. Dietary Changes
What you eat significantly impacts ulcer healing and pain levels. Adopting a gentle diet can significantly reduce irritation.
- Avoid acidic foods: Citrus fruits, tomatoes, coffee, alcohol, and spicy foods can exacerbate ulcer pain.
- Eat small, frequent meals: This prevents your stomach from becoming overly full and producing excess acid.
- Increase fiber intake: Fiber promotes healthy digestion and can help protect your stomach lining.
- Stay hydrated: Drinking plenty of water aids in digestion and helps dilute stomach acid.
- Consider bland foods: Opt for easily digestible foods like plain rice, toast, oatmeal, and boiled potatoes until your ulcer heals.
3. Lifestyle Modifications
Certain lifestyle habits can either worsen or improve ulcer symptoms. Making positive changes can contribute to faster healing.
- Quit smoking: Smoking significantly impairs ulcer healing and increases the risk of complications.
- Manage stress: Stress can worsen ulcers. Practice stress-reduction techniques like yoga, meditation, or deep breathing.
- Avoid NSAIDs: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen can irritate the stomach and worsen ulcers. Consult your doctor about alternatives.
- Get enough sleep: Adequate rest is crucial for healing and overall health.
- Maintain a healthy weight: Obesity can contribute to digestive issues.
4. Home Remedies (Use with Caution)
While not substitutes for medical treatment, some home remedies might provide temporary relief. Always consult your doctor before trying any home remedy, particularly if you have other health conditions.
- Aloe vera juice: Some studies suggest it may have soothing effects on the stomach lining.
- Cabbage juice: Contains compounds that may help with ulcer healing.
- Licorice root (consult a doctor first): It has anti-inflammatory properties, but potential drug interactions exist.
5. When to Seek Immediate Medical Attention
Ulcer pain isn't always a simple inconvenience; sometimes it signals a serious problem. Seek immediate medical attention if you experience:
- Severe, persistent pain: Pain that doesn't respond to medication or home remedies.
- Bloody or black stools: This indicates potential bleeding from the ulcer.
- Vomiting blood: A serious symptom requiring immediate medical attention.
- Sudden, sharp pain: Could indicate perforation (a hole in the stomach lining).
- Signs of dehydration: Excessive vomiting or diarrhea can lead to dehydration.
Why do mouth ulcers hurt so much?
Mouth ulcers, also known as aphthous ulcers or canker sores, are painful lesions that develop inside the mouth. Their intense pain stems from a combination of factors. The exposed nerve endings in the ulcer bed are highly sensitive, making them exquisitely vulnerable to irritation from food, drink, and even saliva. The inflammatory process itself contributes significantly to the pain. The body's immune response to the ulcer involves the release of various inflammatory mediators, such as bradykinin and prostaglandins, which directly stimulate nerve fibers and amplify pain signals. Furthermore, the ulcer's acidic environment can further irritate the already sensitive tissue. The depth and size of the ulcer also play a role; deeper and larger ulcers tend to be more painful. Finally, the location of the ulcer influences the intensity of pain, as ulcers on the tongue or soft palate are often perceived as more painful due to their increased nerve density.
The Role of Nerve Endings
Mouth ulcers are incredibly sensitive because they expose a high concentration of nerve endings. These nerve fibers transmit pain signals directly to the brain. The lack of a protective epithelial layer over the ulcer bed intensifies the sensitivity. Even mild stimulation, such as contact with food or drink, can trigger significant pain. The density of nerve endings in the affected area directly correlates with the intensity of pain experienced.
- Nerve fiber exposure: The ulcer breaks the protective surface of the mouth, exposing underlying nerve endings.
- Direct stimulation: Any contact with the ulcer, no matter how gentle, stimulates these exposed nerves.
- Signal transmission: These nerves transmit pain signals rapidly to the brain, resulting in the perceived discomfort.
The Inflammatory Response
The body's inflammatory response to a mouth ulcer plays a significant role in pain. The immune system attempts to heal the wound, releasing various chemicals that cause swelling, redness, and pain. These inflammatory mediators, such as bradykinin and prostaglandins, sensitize pain receptors and amplify pain signals. The inflammatory process often persists throughout the ulcer's lifespan, prolonging pain.
- Mediator release: The body releases inflammatory mediators to fight infection and promote healing.
- Pain receptor sensitization: These mediators make pain receptors more sensitive, even to mild stimuli.
- Prolonged inflammation: Inflammation continues as long as the ulcer persists, leading to sustained pain.
The Ulcer's Acidic Environment
The environment within a mouth ulcer is often acidic. This acidity can further irritate the already damaged and sensitive tissues, contributing to the burning or stinging sensation often associated with these lesions. The acidic environment can directly damage nerve endings and exacerbate pain. This contributes to the overall discomfort, especially when the ulcer is located in a sensitive area of the mouth.
- Acid production: Bacterial activity within the ulcer can contribute to an acidic environment.
- Tissue damage: The acidic pH can damage the already compromised tissue within the ulcer.
- Increased sensitivity: This damage can increase the sensitivity of the area, making it more prone to pain.
Depth and Size of the Ulcer
Larger and deeper mouth ulcers generally cause more intense pain. The extent of tissue damage and nerve involvement directly correlates with pain levels. A deeper ulcer exposes a larger area of nerve endings, potentially leading to more intense pain signals. Similarly, larger ulcers impact a wider area of the oral mucosa, resulting in a greater overall area of discomfort.
- Tissue damage: Deeper ulcers cause more significant tissue damage and nerve involvement.
- Nerve fiber density: Larger ulcers affect a greater area with a high density of nerve fibers.
- Pain signal amplification: The larger affected area transmits a more intense pain signal to the brain.
Location of the Ulcer
The location of the mouth ulcer significantly influences pain perception. Ulcers in areas with a higher concentration of nerve endings, such as the tongue or soft palate, tend to be more painful. Conversely, ulcers located in areas with fewer nerve endings, such as the hard palate, may cause less intense pain. Nerve density varies across different regions within the mouth, directly affecting pain sensitivity.
- Nerve density variation: Different areas of the mouth possess varying densities of nerve endings.
- Pain perception: Areas with higher nerve density experience more intense pain.
- Location impact: The location of the ulcer directly influences the intensity of the pain experienced.
Does ice help mouth ulcers?
:max_bytes(150000):strip_icc()/canker-sore-remedies-that-actually-work-10589251-5c82c86cc9e77c00010c21d1.png)
Does Ice Help Mouth Ulcers?
While ice can provide temporary relief from the pain and discomfort associated with mouth ulcers (also known as canker sores or aphthous ulcers), it doesn't actually treat the underlying cause. The numbing effect of the cold can help reduce inflammation and pain, but it's a purely symptomatic treatment. Ice won't cure the ulcer, and its effectiveness varies from person to person. Some individuals find significant relief, while others experience little to no benefit. It's important to remember that prolonged exposure to ice can potentially damage the delicate tissues in your mouth, so using it sparingly and correctly is crucial.
How Does Ice Help Mouth Ulcers?
The primary mechanism by which ice helps mouth ulcers is through its vasoconstrictive properties. Applying ice to the affected area causes the blood vessels to constrict, reducing blood flow to the ulcer. This reduction in blood flow can help minimize swelling and inflammation, thereby lessening pain and discomfort. Additionally, the cold temperature has a numbing effect on the nerve endings, providing temporary pain relief. However, it's important to note that this is only temporary relief and doesn't address the root cause of the ulcer.
- Reduces inflammation by constricting blood vessels.
- Numbs the nerve endings, providing temporary pain relief.
- Can help reduce swelling.
When to Use Ice for Mouth Ulcers
Ice can be a useful tool for managing the pain of a mouth ulcer, especially during the initial stages when the pain is most intense. It's particularly helpful if you're experiencing significant discomfort that's interfering with your daily life, such as eating or speaking. However, it's crucial to use ice cautiously and only for short periods of time to avoid tissue damage. It's not a substitute for proper medical treatment if the ulcers are persistent, severe, or unusually frequent.
- During initial stages when pain is most severe.
- When discomfort impacts daily activities (eating, speaking).
- As a temporary pain management strategy.
How to Use Ice Safely for Mouth Ulcers
To use ice effectively and safely for mouth ulcers, wrap an ice cube or ice pack in a thin, clean cloth or paper towel. Never apply ice directly to the skin, as this can cause significant tissue damage. Apply the ice pack to the affected area for no more than 10-15 minutes at a time, several times a day as needed. Allow at least 30 minutes between applications to prevent tissue damage from the cold. If you experience increased pain or numbness, stop using the ice immediately.
- Wrap ice in a clean cloth before applying.
- Apply for 10-15 minutes at a time.
- Allow at least 30 minutes between applications.
Limitations of Using Ice for Mouth Ulcers
It's crucial to understand that ice is not a cure for mouth ulcers. While it can temporarily alleviate pain and discomfort, it does not address the underlying causes of the ulcers. Furthermore, prolonged exposure to ice can damage the delicate tissues of the mouth, leading to further discomfort and potentially delaying healing. Ice should be considered a temporary pain management tool, not a primary treatment for mouth ulcers.
- Does not treat the underlying cause of the ulcers.
- Prolonged use can damage mouth tissues.
- Only provides temporary pain relief.
What are mouth ulcers?
Mouth ulcers, also known as aphthous ulcers or canker sores, are small, shallow lesions that develop on the soft tissues in your mouth. They're characterized by a painful, whitish-gray center surrounded by a reddish border. The size can vary, ranging from tiny (less than a centimeter) to quite large, causing significant discomfort. Several factors can contribute to their formation, including stress, hormonal changes (like menstruation), injuries to the mouth (from biting your cheek or accidental burns), nutritional deficiencies (such as iron, vitamin B12, or folate), and even certain medical conditions like inflammatory bowel disease. They are not contagious, unlike cold sores (caused by the herpes simplex virus). While typically harmless and self-limiting, meaning they heal on their own within 1-3 weeks, recurrent and persistent mouth ulcers can be a sign of underlying health issues, requiring a visit to a doctor or dentist. The exact cause of mouth ulcers isn't fully understood, but it's thought to involve an immune system response. Understanding this helps in identifying ways to manage and prevent them.
How can I relieve the pain of a mouth ulcer?
Managing the pain associated with mouth ulcers is crucial for comfort. Several readily available over-the-counter remedies can provide significant relief. Rinsing your mouth with a saltwater solution (a half-teaspoon of salt in a glass of warm water) several times a day can help clean the area and reduce inflammation. Applying a topical anesthetic gel or cream containing benzocaine or lidocaine can numb the affected area, offering immediate pain relief. These are usually available at pharmacies without a prescription. Avoid acidic, spicy, or highly seasoned foods as these can irritate the ulcer and exacerbate the pain. Opt for soft, bland foods that are easy to chew and swallow, such as mashed potatoes, yogurt, or applesauce. Furthermore, drinking plenty of fluids helps keep the mouth hydrated and promotes healing. Some people find relief from applying a small amount of milk of magnesia directly to the ulcer using a cotton swab. However, if the pain is severe, persistent, or accompanied by other symptoms, consult a healthcare professional.
What are some home remedies for mouth ulcers?
Beyond over-the-counter treatments, several home remedies are often suggested for managing mouth ulcers. Aloe vera gel, known for its soothing and anti-inflammatory properties, can be applied directly to the ulcer to provide pain relief and accelerate healing. Honey, with its natural antibacterial and wound-healing properties, can also be applied topically. Make sure it's pure, raw honey. Ice cubes can be held against the affected area for short periods to reduce swelling and numb the pain. Similarly, lukewarm chamomile tea can be used as a rinse; it has calming and anti-inflammatory effects. Remember that these remedies may not be effective for everyone, and their efficacy varies. Maintaining good oral hygiene is crucial for preventing the worsening of mouth ulcers, so continue brushing and flossing gently, avoiding direct contact with the ulcer itself. While these home remedies offer potential relief, it's important to consult a healthcare provider if symptoms persist or worsen.
When should I see a doctor about a mouth ulcer?
While most mouth ulcers heal within a couple of weeks, there are situations where it's crucial to seek professional medical advice. If your mouth ulcer is exceptionally large, lasts longer than three weeks, or is accompanied by other symptoms like fever, swollen lymph nodes, or difficulty swallowing, you should consult a doctor or dentist immediately. These symptoms may indicate a more serious underlying condition. Similarly, if you experience frequent or recurrent mouth ulcers, especially if they are severely painful or interfere with your daily life, it is important to seek medical attention. A healthcare professional can help determine the underlying cause of the ulcers and recommend appropriate treatment, potentially including medications or dietary changes. Don't hesitate to contact a healthcare provider if you're experiencing significant discomfort or have any concerns about your mouth ulcers. Early diagnosis and treatment can prevent complications and improve your overall oral health.

Deja una respuesta