Do mouth ulcers mean a low immune system

Mouth ulcers, also known as canker sores, are lesions that develop in the mouth and can cause discomfort and pain. They are a common problem, with an estimated 20% of the population experiencing an ulcer at least once a year. While the exact cause of mouth ulcers is unknown, it is believed to be related to a number of factors, including stress, hormonal changes, and certain foods. There is also a belief that mouth ulcers may be a sign of a compromised immune system.
Do Mouth Ulcers Indicate a Weakened Immune System?
While mouth ulcers, also known as aphthous ulcers or canker sores, are a common occurrence, their relationship with a weakened immune system is complex and not fully understood. While a compromised immune system can increase the frequency and severity of mouth ulcers for some individuals, it's not a direct cause-and-effect relationship. Many factors contribute to mouth ulcer development, and a single ulcer doesn't automatically signal a low immune system. However, recurring or unusually severe mouth ulcers could be a symptom of an underlying issue, including immune deficiency. It's important to consult a doctor or dentist for proper diagnosis and treatment if you experience persistent or concerning symptoms.
What Causes Mouth Ulcers?
The exact cause of mouth ulcers remains unclear, but several factors are implicated. Minor trauma to the mouth (e.g., biting your cheek), stress, hormonal changes (like menstruation), certain foods (e.g., acidic or spicy foods), and nutritional deficiencies (e.g., vitamin B12, iron, or folate deficiency) can all trigger their formation. In some cases, underlying medical conditions, such as inflammatory bowel disease or celiac disease, can also contribute. While a weakened immune system can make an individual more susceptible to these triggers and potentially lead to more frequent or severe ulcers, it’s not always the primary cause. It's crucial to note that many individuals with perfectly healthy immune systems also experience mouth ulcers.
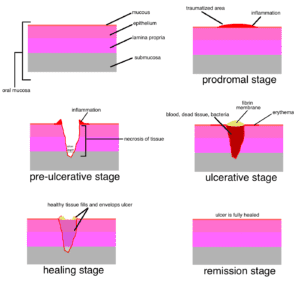
The Immune System's Role in Wound Healing
The immune system plays a crucial role in the healing process of any wound, including mouth ulcers. A healthy immune system efficiently manages inflammation, fights infection, and promotes tissue repair. However, a compromised immune system might delay healing and increase the risk of infection, potentially leading to more persistent or painful ulcers. This doesn't mean that every mouth ulcer points to a weakened immune system, but a prolonged healing time might warrant further investigation.
When Should You See a Doctor About Mouth Ulcers?
While occasional mouth ulcers are usually harmless, you should consult a doctor or dentist if you experience: frequent or persistent ulcers, ulcers that are unusually large or painful, ulcers that bleed excessively, ulcers accompanied by fever or other symptoms, or ulcers that don't heal within two weeks. These could be signs of an underlying medical condition, including an immune deficiency, requiring medical attention.
Other Conditions Mimicking Mouth Ulcers
It's important to remember that some conditions can mimic the appearance of mouth ulcers. Certain infections, like herpes simplex virus (HSV) or hand, foot, and mouth disease, can cause sores that resemble canker sores. Oral cancers can also present as mouth lesions. A healthcare professional can accurately diagnose the cause of your mouth sores through a physical examination and potentially further testing.
How to Support a Healthy Immune System
Maintaining a healthy lifestyle can generally support a strong immune system. This includes: eating a balanced diet rich in fruits, vegetables, and whole grains, getting sufficient sleep, managing stress levels effectively, engaging in regular exercise, and avoiding smoking and excessive alcohol consumption. These practices can contribute to overall health and well-being, potentially reducing the frequency and severity of mouth ulcers, among other health benefits.
| Symptom | Possible Indication |
|---|---|
| Frequent, recurring mouth ulcers | Possible underlying medical condition, including immune deficiency, but not always indicative of a low immune system. |
| Large, painful, or slow-healing ulcers | May indicate an underlying issue, warranting medical attention. |
| Ulcers accompanied by fever or other symptoms | Suggests a more serious condition requiring immediate medical evaluation. |
| Mouth ulcers with unusual appearance | Could indicate a different condition, such as an infection or oral cancer. |
https://youtube.com/watch?v=cnFGz6iY4es%26pp%3DygUJI2FpZGFwdHVz
Do Mouth Ulcers Indicate a Weakened Immune System?
While mouth ulcers, also known as aphthous ulcers or canker sores, are a common occurrence, their relationship with a weakened immune system is complex and not fully understood. While a compromised immune system can increase the frequency and severity of mouth ulcers for some individuals, it's not a direct cause-and-effect relationship. Many factors contribute to mouth ulcer development, and a single ulcer doesn't automatically signal a low immune system. However, recurring or unusually severe mouth ulcers could be a symptom of an underlying issue, including immune deficiency. It's important to consult a doctor or dentist for proper diagnosis and treatment if you experience persistent or concerning symptoms.
What Causes Mouth Ulcers?
The exact cause of mouth ulcers remains unclear, but several factors are implicated. Minor trauma to the mouth (e.g., biting your cheek), stress, hormonal changes (like menstruation), certain foods (e.g., acidic or spicy foods), and nutritional deficiencies (e.g., vitamin B12, iron, or folate deficiency) can all trigger their formation. In some cases, underlying medical conditions, such as inflammatory bowel disease or celiac disease, can also contribute. While a weakened immune system can make an individual more susceptible to these triggers and potentially lead to more frequent or severe ulcers, it’s not always the primary cause. It's crucial to note that many individuals with perfectly healthy immune systems also experience mouth ulcers.
The Immune System's Role in Wound Healing
The immune system plays a crucial role in the healing process of any wound, including mouth ulcers. A healthy immune system efficiently manages inflammation, fights infection, and promotes tissue repair. However, a compromised immune system might delay healing and increase the risk of infection, potentially leading to more persistent or painful ulcers. This doesn't mean that every mouth ulcer points to a weakened immune system, but a prolonged healing time might warrant further investigation.
When Should You See a Doctor About Mouth Ulcers?
While occasional mouth ulcers are usually harmless, you should consult a doctor or dentist if you experience: frequent or persistent ulcers, ulcers that are unusually large or painful, ulcers that bleed excessively, ulcers accompanied by fever or other symptoms, or ulcers that don't heal within two weeks. These could be signs of an underlying medical condition, including an immune deficiency, requiring medical attention.
Other Conditions Mimicking Mouth Ulcers
It's important to remember that some conditions can mimic the appearance of mouth ulcers. Certain infections, like herpes simplex virus (HSV) or hand, foot, and mouth disease, can cause sores that resemble canker sores. Oral cancers can also present as mouth lesions. A healthcare professional can accurately diagnose the cause of your mouth sores through a physical examination and potentially further testing.
How to Support a Healthy Immune System
Maintaining a healthy lifestyle can generally support a strong immune system. This includes: eating a balanced diet rich in fruits, vegetables, and whole grains, getting sufficient sleep, managing stress levels effectively, engaging in regular exercise, and avoiding smoking and excessive alcohol consumption. These practices can contribute to overall health and well-being, potentially reducing the frequency and severity of mouth ulcers, among other health benefits.
| Symptom | Possible Indication |
|---|---|
| Frequent, recurring mouth ulcers | Possible underlying medical condition, including immune deficiency, but not always indicative of a low immune system. |
| Large, painful, or slow-healing ulcers | May indicate an underlying issue, warranting medical attention. |
| Ulcers accompanied by fever or other symptoms | Suggests a more serious condition requiring immediate medical evaluation. |
| Mouth ulcers with unusual appearance | Could indicate a different condition, such as an infection or oral cancer. |
Do mouth ulcers mean you are getting sick?
Mouth ulcers, also known as aphthous ulcers or canker sores, are small, shallow lesions that develop on the soft tissues in your mouth. While they're incredibly common and usually harmless, they don't directly mean you're getting sick in the sense of having a contagious illness. The precise cause of mouth ulcers isn't fully understood, but several factors can trigger their appearance. These include minor injuries to the mouth (like biting your cheek), stress, hormonal changes, nutritional deficiencies (like iron or vitamin B12), and certain medical conditions. While a mouth ulcer itself isn't a sign of a broader illness, its appearance mightcoincide with the onset of an illness due to the shared underlying factors like stress or a weakened immune system. However, the ulcer is not the cause of the illness, nor is the illness necessarily causing the ulcer.
Possible Connections Between Mouth Ulcers and Illness
Although mouth ulcers aren't a direct indicator of illness, there can be indirect connections. A weakened immune system, often associated with illness, might make you more susceptible to developing mouth ulcers. Similarly, stress, a common trigger for both illness and mouth ulcers, could lead to their simultaneous appearance. However, it's crucial to remember correlation doesn't equal causation. The presence of a mouth ulcer doesn't automatically mean you're contracting an infection or other illness.
- Stress and Immune Function: Stress significantly impacts immune function. A compromised immune system might make you more prone to both infections and mouth ulcers.
- Nutritional Deficiencies: Deficiencies in certain vitamins and minerals, such as iron, vitamin B12, and folic acid, are known to increase the risk of mouth ulcers. These deficiencies can also weaken the immune system making you more vulnerable to illness.
- Coincidence: Sometimes, a mouth ulcer might appear around the same time as you develop another illness, purely by coincidence. There's no direct causal link.
Viral Infections and Mouth Ulcers
While mouth ulcers are not themselves caused by viruses, some viral infections can sometimes precedethe appearance of mouth ulcers. This could be due to the body's overall weakened state and increased susceptibility to minor problems. It's important to understand that this is not a direct cause-and-effect relationship. The virus doesn't directly causethe mouth ulcer; rather, a weakened immune system combating the virus might make the ulcer more likely to develop.
- Weakened Immunity: Viral infections often temporarily weaken the immune system, creating a more favorable environment for the development of mouth ulcers.
- Timing: The appearance of mouth ulcers after a viral infection may be purely coincidental; the ulcer could have developed regardless of the viral infection.
- Underlying Factors: Both viral infections and mouth ulcers can be exacerbated by similar underlying factors such as stress and poor nutrition.
Differentiating Mouth Ulcers from Other Oral Conditions
It's vital to distinguish mouth ulcers from other oral conditions that canindicate illness. For example, cold sores (caused by the herpes simplex virus) are contagious and a sign of viral infection. Mouth ulcers are not contagious. If you have concerns about an oral lesion, it's crucial to consult a doctor or dentist for a proper diagnosis to rule out other, more serious conditions.
- Cold Sores: Cold sores are caused by the herpes simplex virus and are highly contagious. They are distinct from mouth ulcers in appearance and cause.
- Oral Thrush: Oral thrush, a fungal infection, can present as white patches in the mouth and requires medical treatment.
- Oral Cancer: While rare, persistent or unusual oral lesions warrant immediate medical attention to rule out the possibility of oral cancer.
When to See a Doctor About Mouth Ulcers
Most mouth ulcers heal on their own within a week or two. However, there are instances where you should consult a medical professional. Persistent ulcers that don't heal, unusually large or painful ulcers, or ulcers accompanied by other symptoms (fever, swollen lymph nodes, etc.) warrant a doctor's visit. This is important to rule out underlying medical conditions or infections.
- Persistent Ulcers: Ulcers that last longer than two weeks require medical evaluation.
- Severe Pain or Size: Excessively painful or large ulcers may indicate a more serious underlying issue.
- Accompanying Symptoms: Fever, swollen glands, or other systemic symptoms along with mouth ulcers necessitate a doctor's consultation.
Mouth Ulcer Treatment and Prevention
While many mouth ulcers resolve spontaneously, there are ways to manage them and reduce their recurrence. Over-the-counter pain relievers and mouthwashes can help alleviate discomfort. Maintaining good oral hygiene, reducing stress, and ensuring adequate nutrition are key preventative measures. In some cases, a doctor may prescribe medication to address underlying causes or persistent ulcers.
- Over-the-counter Treatments: Pain relievers, topical anesthetics, and mouthwashes can provide temporary relief.
- Lifestyle Changes: Reducing stress, improving diet, and maintaining good oral hygiene are crucial in preventing future occurrences.
- Prescription Medications: For recurrent or severe ulcers, a doctor may prescribe corticosteroids or other medications.
What is my body lacking if I keep getting mouth ulcers?
Recurring mouth ulcers, also known as aphthous ulcers, can indicate several underlying deficiencies or imbalances in your body. Pinpointing the exact cause requires a consultation with a doctor or dentist, as self-diagnosis can be inaccurate. However, some common contributing factors related to nutritional deficiencies include:
Nutritional Deficiencies
Several vitamins and minerals play crucial roles in maintaining the health of your oral mucosa. A deficiency in any of these can increase your susceptibility to mouth ulcers. These deficiencies are often interrelated, meaning a lack of one can impact the absorption or utilization of others. A proper diet is key to preventing this.
- Vitamin B12 deficiency: This vitamin is essential for cell growth and repair, including the cells lining your mouth. Deficiency can lead to various symptoms, including mouth sores.
- Iron deficiency: Iron is vital for oxygen transport and overall cell function. Anemia (low iron) is often linked to a weakened immune system, making you more prone to infections, including oral ulcers.
- Folic acid deficiency: This B vitamin is vital for cell growth and repair, similar to Vitamin B12, making it also relevant to oral health. Deficiency can manifest in numerous ways, including mouth sores.
- Zinc deficiency: Zinc plays a role in wound healing and immune function, both important in the recovery from mouth ulcers. A deficiency can impair these processes, leading to prolonged or recurring ulcers.
- Vitamin C deficiency: Though less directly linked than other deficiencies, a severe lack of vitamin C can weaken your immune system, making you more vulnerable to various infections, including mouth ulcers.
Stress and Immune System
Chronic stress significantly impacts your immune system. When your immune system is compromised, you're more likely to develop infections and experience slower healing times, both contributing to recurring mouth ulcers. Managing stress is crucial for overall health, including oral health.
- Elevated Cortisol Levels: Prolonged stress leads to increased cortisol production, a hormone that can suppress immune function.
- Weakened Immune Response: A weakened immune system leaves your body less capable of fighting off infections, including those that can cause mouth ulcers.
- Delayed Wound Healing: Stress can impair the body's ability to heal efficiently, prolonging the duration and increasing the likelihood of recurring ulcers.
Underlying Medical Conditions
Certain medical conditions can increase the risk of mouth ulcers. These conditions often require medical intervention to manage the underlying cause and reduce the frequency of ulcers. Consult a doctor if you suspect an underlying medical condition is contributing to your mouth ulcers.
- Autoimmune diseases: Conditions like Crohn's disease, Behçet's disease, and ulcerative colitis can manifest as oral ulcers.
- Gastrointestinal issues: Problems such as celiac disease or irritable bowel syndrome (IBS) can sometimes be linked to recurrent mouth ulcers.
- Infections: Viral or bacterial infections can also contribute to the formation of mouth ulcers.
Allergies and Irritants
Certain foods, drinks, or oral hygiene products can trigger allergic reactions or irritate the delicate lining of your mouth, leading to mouth ulcers. Identifying and avoiding these triggers is crucial for managing recurring ulcers.
- Food allergies: Sensitivity to certain foods, like nuts, dairy products, or citrus fruits can cause oral irritation leading to ulcers.
- Oral hygiene products: Some toothpastes, mouthwashes, or dental products can contain ingredients that irritate sensitive mouths.
- Certain drinks: Highly acidic drinks like soda or juices can irritate the mouth and contribute to ulcer development.
Lifestyle Factors
Poor oral hygiene, smoking, and inadequate hydration can all negatively impact your oral health. These factors can create an environment conducive to the development and recurrence of mouth ulcers.
- Poor oral hygiene: Neglecting proper brushing and flossing allows bacteria to accumulate, increasing inflammation and the risk of ulcers.
- Smoking: Smoking impairs the body's natural healing processes, reducing the effectiveness of wound healing and increasing the likelihood of ulcers.
- Dehydration: Inadequate water intake can dry out the mucous membranes in your mouth, making them more susceptible to irritation and ulcers.
Why am I prone to mouth ulcers?
Why Am I Prone to Mouth Ulcers?
Mouth ulcers, also known as aphthous ulcers or canker sores, are small, painful sores that develop inside the mouth. The exact cause of mouth ulcers isn't fully understood, but several factors can increase your susceptibility. Genetics play a significant role, with a family history often being a strong predictor. Stress is another major contributing factor, as heightened cortisol levels can weaken the immune system and trigger ulcer formation. Nutritional deficiencies, particularly in iron, vitamin B12, and folic acid, can also increase your risk. Minor injuries to the mouth, like biting your cheek or accidental abrasion from a toothbrush, can initiate an ulcer. Finally, certain medical conditions and medications can be implicated. The interplay of these factors makes determining the precise reason for your individual proneness to mouth ulcers complex.
Genetic Predisposition
A family history of mouth ulcers significantly increases your risk. If multiple family members experience frequent outbreaks, the likelihood of you experiencing them is also higher. This suggests a genetic component that influences immune responses and the susceptibility to ulcer development. The exact genes involved are still under investigation, but research is ongoing to pinpoint specific genetic markers associated with increased mouth ulcer prevalence.
- Inherited immune system characteristics can make some individuals more vulnerable to triggering events.
- Genetic studies are investigating specific genes that might influence mouth ulcer development.
- Family history provides a strong indicator of personal susceptibility.
Stress and Immune Function
Chronic or acute stress is a well-established trigger for mouth ulcers. When stressed, the body releases cortisol, a hormone that can suppress the immune system. This weakened immune response makes you more vulnerable to various infections and irritations, including the development of mouth ulcers. Managing stress levels through techniques like meditation, exercise, or yoga can be beneficial in preventing outbreaks.
- Elevated cortisol levels suppress the immune system.
- Stress weakens the body's ability to fight off minor irritations.
- Stress management techniques can significantly reduce ulcer frequency.
Nutritional Deficiencies
Deficiencies in certain vitamins and minerals, such as iron, vitamin B12, and folic acid, have been linked to an increased incidence of mouth ulcers. These nutrients play crucial roles in cell growth and repair, and a deficiency can impair the mouth's ability to heal itself. Ensuring a balanced diet rich in these nutrients can help to prevent or reduce the severity of mouth ulcer outbreaks.
- Iron deficiency anemia is strongly associated with increased mouth ulcer frequency.
- Vitamin B12 and folic acid are essential for proper cell function and healing.
- A balanced diet rich in fruits, vegetables, and whole grains is crucial for preventing deficiencies.
Trauma and Irritation
Minor injuries to the mouth, such as biting your cheek, accidentally scratching the inside of your mouth, or using a harsh toothbrush, can cause mouth ulcers. These injuries disrupt the delicate lining of the mouth, creating an opening for inflammation and ulcer formation. Using a soft-bristled toothbrush, avoiding sharp foods, and practicing good oral hygiene can help minimize the risk of these types of injuries.
- Rough toothbrushes or aggressive brushing can damage the soft tissues.
- Sharp or hard foods can cause abrasions inside the mouth.
- Gentle oral hygiene practices are crucial for preventing trauma.
Underlying Medical Conditions and Medications
Certain medical conditions, such as inflammatory bowel disease (IBD), Behçet's disease, and Crohn's disease, are associated with a higher incidence of mouth ulcers. Some medications, such as chemotherapy drugs and non-steroidal anti-inflammatory drugs (NSAIDs), can also increase your risk. If you are experiencing frequent mouth ulcers, it's important to consult a doctor to rule out any underlying medical issues or medication interactions.
- Inflammatory bowel disease (IBD) often presents with oral manifestations.
- Certain medications can have mouth ulceration as a side effect.
- Consult a physician if mouth ulcers are persistent or severe.
What diseases are mouth ulcers a symptom of?
Mouth ulcers, also known as aphthous ulcers or canker sores, are a common symptom of several conditions, but they are not always indicative of a serious underlying illness. Their cause is often unknown, but certain factors like stress, injury, or hormonal changes can trigger them. However, recurring or unusual mouth ulcers may warrant medical attention to rule out more serious conditions.
Here's a more detailed look at some diseases and conditions where mouth ulcers can be a symptom:
Behçet's Disease
Behçet's disease is a rare, chronic inflammatory disorder that affects blood vessels throughout the body. Mouth ulcers are a hallmark symptom of Behçet's disease, often appearing as painful, recurrent sores that can persist for several weeks. Other symptoms include genital ulcers, skin lesions, and eye inflammation. The exact cause of Behçet's disease is unknown, but it's believed to involve an autoimmune response.
- Recurrent and painful mouth ulcers are a defining characteristic.
- Genital ulcers and skin lesions are common.
- Eye inflammation (uveitis) can lead to vision problems.
Inflammatory Bowel Disease (IBD)
Inflammatory bowel diseases, such as Crohn's disease and ulcerative colitis, are chronic conditions that cause inflammation in the digestive tract. While not always present, mouth ulcers can be a manifestation of IBD, especially in individuals with Crohn's disease. The ulcers may be associated with other gastrointestinal symptoms like abdominal pain, diarrhea, and weight loss. The connection between IBD and mouth ulcers is not fully understood, but it's likely related to the systemic inflammation associated with the disease.
- Mouth ulcers can occur alongside other gastrointestinal symptoms.
- Crohn's disease is more strongly associated with mouth ulcers than ulcerative colitis.
- The severity of mouth ulcers may correlate with the severity of IBD symptoms.
HIV/AIDS
In the early stages of HIV infection, oral candidiasis (thrush), characterized by white patches on the tongue and inner cheeks, can occur. While not strictly a mouth ulcer, thrush can be a precursor to more significant oral lesions. As HIV progresses to AIDS, severe immunosuppression leads to opportunistic infections that can cause more extensive oral ulcers and other manifestations of the disease. It's crucial to get tested for HIV if you experience persistent or unusual oral symptoms.
- Oral thrush (candidiasis) is a common early sign of HIV infection.
- Severe immunosuppression increases the risk of developing more serious oral ulcers.
- Other opportunistic infections can occur in the mouth and elsewhere in the body.
Vitamin Deficiencies
Deficiencies in certain vitamins, such as B vitamins (B12, folate) and iron, can lead to various health problems, including mouth ulcers. These deficiencies can affect the body's ability to repair tissues, making it more susceptible to ulcers and other complications. A doctor can perform blood tests to determine if vitamin deficiencies are contributing to the development of mouth ulcers. Addressing the underlying deficiency typically resolves the issue.
- B vitamin (B12, folate) and iron deficiencies are common causes.
- These deficiencies impair tissue repair.
- Blood tests can help diagnose and monitor vitamin levels.
Lupus
Systemic lupus erythematosus (SLE) is an autoimmune disease that can affect multiple organs and systems. While mouth ulcers are not always present, they can occur as a symptom of lupus in some individuals. Other symptoms can include joint pain, fatigue, skin rashes, and kidney problems. The ulcers in lupus may be related to the systemic inflammation and immune dysfunction characteristic of the disease. Diagnosis requires a thorough medical evaluation.
- Mouth ulcers can be a symptom, though not a defining characteristic.
- Lupus presents with various symptoms affecting different organ systems.
- Diagnosis requires comprehensive testing and clinical assessment.
Do mouth ulcers always indicate a weakened immune system?
Not necessarily. While a weakened immune system can make you more susceptible to developing mouth ulcers, they don't always directly indicate a compromised immune response. Many factors can trigger mouth ulcers, including minor trauma to the mouth (like accidentally biting your cheek), stress, hormonal changes (particularly in women), certain food allergies or sensitivities, and even deficiencies in certain vitamins and minerals like iron, B12, or zinc. A person with a perfectly healthy immune system can still experience mouth ulcers from time to time. The presence of mouth ulcers alone is not a reliable indicator of a weakened immune system. If you're concerned about your immune system, it's best to consult a doctor for a proper assessment rather than relying solely on the presence or absence of mouth ulcers.
If I have recurring mouth ulcers, does this mean my immune system is constantly low?
Recurring mouth ulcers, while often frustrating, don't automatically equate to a constantly low immune system. As mentioned before, many factors besides immune function contribute to their development. Stress, hormonal fluctuations, and nutritional deficiencies can all trigger repeated outbreaks. While a chronically weakened immune system might increase your susceptibility, it's crucial to rule out other causes. A doctor can help determine the underlying reason for your recurring ulcers through a thorough examination and possibly some blood tests. They might look at your overall health, diet, and lifestyle to get a complete picture. Self-diagnosing a low immune system based solely on mouth ulcers is inaccurate and can lead to unnecessary worry or delayed appropriate treatment for other potential causes.
Can treating mouth ulcers boost my immune system?
Treating mouth ulcers directly doesn't necessarily boost your overall immune system. While managing the symptoms provides relief, it doesn't address the root cause of a potentially weakened immune system. If your mouth ulcers are a symptom of an underlying immune deficiency, treating the underlying condition is essential for improving your overall immune health. For example, if a vitamin deficiency is contributing to your mouth ulcers, supplementing with that vitamin will help alleviate the ulcers but primarily addresses the deficiency, not directly strengthening the immune system. In cases where stress is a contributing factor, stress management techniques like exercise, yoga, or mindfulness could help reduce ulcer frequency and indirectly benefit immune function by reducing overall stress levels. However, it's important to understand that treating mouth ulcers focuses on managing the symptoms, not directly bolstering the immune system.
What should I do if I'm worried about my immune system and have mouth ulcers?
If you're concerned about a potential weakened immune system and are experiencing mouth ulcers, the best course of action is to consult a doctor. They can conduct a thorough assessment, consider your medical history, and order relevant tests (like blood tests) to determine if there is an underlying immune deficiency or other health condition contributing to your symptoms. Based on the assessment, they can provide appropriate recommendations, which might include addressing nutritional deficiencies, managing stress, or referring you to specialists for further evaluation if necessary. Don't self-diagnose or self-treat; a professional medical opinion is crucial for accurate diagnosis and effective management of your health concerns.

Deja una respuesta