Why have I suddenly got mouth ulcers

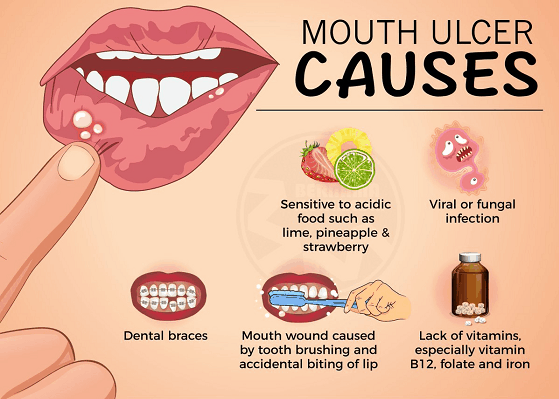
Mouth ulcers, also known as canker sores, are small, painful sores that can develop inside the mouth. They are a common problem, affecting up to 20% of the population. While mouth ulcers are usually not serious, they can be uncomfortable and interfere with eating, drinking, and talking. There are many different causes of mouth ulcers, including stress, hormonal changes, certain foods, and nutritional deficiencies. In some cases, mouth ulcers can be a sign of an underlying medical condition. If you are experiencing frequent or severe mouth ulcers, it is important to see a doctor to rule out any underlying causes.
Why Have I Suddenly Got Mouth Ulcers?
The sudden appearance of mouth ulcers, also known as aphthous ulcers or canker sores, can be frustrating and painful. While they're usually harmless and heal on their own within a week or two, understanding the potential causes can help you manage them better and potentially prevent future outbreaks. There isn't one single definitive answer to why you've suddenly developed mouth ulcers, as various factors can trigger them. Often, it's a combination of contributing elements rather than a single culprit.
Stress and Anxiety
Stress and anxiety are commonly cited triggers for mouth ulcers. When you're stressed, your immune system can be weakened, making you more susceptible to infections and inflammation, including mouth ulcers. Managing stress through techniques like exercise, meditation, yoga, or sufficient sleep can be beneficial in reducing their frequency and severity. It's important to note that while stress is a common trigger, it doesn't directly cause the ulcers; it creates an environment where they're more likely to develop.
Minor Injuries to the Mouth
Even minor trauma to the inside of your mouth, such as accidentally biting your cheek, brushing too hard, or using harsh mouthwash, can initiate the formation of a mouth ulcer. The injury triggers an inflammatory response, leading to the characteristic painful sore. Being mindful of how you brush your teeth and avoiding sharp foods can help minimize the risk of accidental injuries.
Nutritional Deficiencies
Nutritional deficiencies, particularly in vitamin B12, iron, and folic acid, can sometimes contribute to the development of mouth ulcers. A deficiency weakens your immune system, making you more prone to various infections and inflammatory responses, including mouth ulcers. A balanced diet rich in these nutrients can help, but it's crucial to consult a doctor to rule out deficiencies if mouth ulcers are recurrent.
Certain Medications
Some medications can have mouth ulcers as a side effect. This is often seen with medications that affect the immune system or cause dryness in the mouth. Always consult your doctor or pharmacist if you suspect a medication might be contributing to your mouth ulcers. They may be able to suggest alternatives or adjustments to your treatment plan.
Hormonal Changes
Hormonal fluctuations, particularly those experienced during menstruation or pregnancy, can influence the immune system and potentially trigger mouth ulcers. The exact mechanism is not fully understood, but the changes in hormone levels seem to play a role in the increased susceptibility to mouth ulcers during these periods. While this is a potential contributing factor, it's important to remember that many women experience hormonal changes without developing mouth ulcers.
| Potential Cause | Description | Management |
|---|---|---|
| Stress | Weakened immune system, increased inflammation. | Stress management techniques (exercise, meditation, etc.) |
| Minor Injuries | Trauma to the mouth lining. | Gentle brushing, avoiding sharp foods. |
| Nutritional Deficiencies (B12, Iron, Folic Acid) | Weakened immune system. | Balanced diet, consult doctor for testing. |
| Medications | Side effect of certain drugs. | Consult doctor about medication alternatives. |
| Hormonal Changes | Fluctuations in hormone levels. | No specific management, usually resolves with hormonal balance. |
https://youtube.com/watch?v=mouth-ulcers
Why Have I Suddenly Got Mouth Ulcers?
The sudden appearance of mouth ulcers, also known as aphthous ulcers or canker sores, can be frustrating and painful. While they're usually harmless and heal on their own within a week or two, understanding the potential causes can help you manage them better and potentially prevent future outbreaks. There isn't one single definitive answer to why you've suddenly developed mouth ulcers, as various factors can trigger them. Often, it's a combination of contributing elements rather than a single culprit.
Stress and Anxiety
Stress and anxiety are commonly cited triggers for mouth ulcers. When you're stressed, your immune system can be weakened, making you more susceptible to infections and inflammation, including mouth ulcers. Managing stress through techniques like exercise, meditation, yoga, or sufficient sleep can be beneficial in reducing their frequency and severity. It's important to note that while stress is a common trigger, it doesn't directly cause the ulcers; it creates an environment where they're more likely to develop.
Minor Injuries to the Mouth
Even minor trauma to the inside of your mouth, such as accidentally biting your cheek, brushing too hard, or using harsh mouthwash, can initiate the formation of a mouth ulcer. The injury triggers an inflammatory response, leading to the characteristic painful sore. Being mindful of how you brush your teeth and avoiding sharp foods can help minimize the risk of accidental injuries.
Nutritional Deficiencies
Nutritional deficiencies, particularly in vitamin B12, iron, and folic acid, can sometimes contribute to the development of mouth ulcers. A deficiency weakens your immune system, making you more prone to various infections and inflammatory responses, including mouth ulcers. A balanced diet rich in these nutrients can help, but it's crucial to consult a doctor to rule out deficiencies if mouth ulcers are recurrent.
Certain Medications
Some medications can have mouth ulcers as a side effect. This is often seen with medications that affect the immune system or cause dryness in the mouth. Always consult your doctor or pharmacist if you suspect a medication might be contributing to your mouth ulcers. They may be able to suggest alternatives or adjustments to your treatment plan.
Hormonal Changes
Hormonal fluctuations, particularly those experienced during menstruation or pregnancy, can influence the immune system and potentially trigger mouth ulcers. The exact mechanism is not fully understood, but the changes in hormone levels seem to play a role in the increased susceptibility to mouth ulcers during these periods. While this is a potential contributing factor, it's important to remember that many women experience hormonal changes without developing mouth ulcers.
| Potential Cause | Description | Management |
|---|---|---|
| Stress | Weakened immune system, increased inflammation. | Stress management techniques (exercise, meditation, etc.) |
| Minor Injuries | Trauma to the mouth lining. | Gentle brushing, avoiding sharp foods. |
| Nutritional Deficiencies (B12, Iron, Folic Acid) | Weakened immune system. | Balanced diet, consult doctor for testing. |
| Medications | Side effect of certain drugs. | Consult doctor about medication alternatives. |
| Hormonal Changes | Fluctuations in hormone levels. | No specific management, usually resolves with hormonal balance. |
Why am I getting mouth ulcers all of a sudden?

The sudden onset of mouth ulcers, also known as aphthous ulcers or canker sores, can be frustrating and painful. There isn't one single cause, and it often depends on a combination of factors. Several possibilities exist, and pinpointing the exact reason requires a consultation with a healthcare professional. However, some common culprits include:
Stress
Stress is a significant trigger for many people. When you're stressed, your immune system can be weakened, making you more susceptible to infections and inflammation, including mouth ulcers. Managing stress through techniques like exercise, meditation, or yoga can be beneficial.
- Physical stress: Lack of sleep, intense exercise, or illness can all contribute.
- Emotional stress: Anxiety, depression, and major life changes can significantly impact your oral health.
- Consider stress reduction techniques: Explore methods like deep breathing exercises, mindfulness, or therapy.
Nutritional Deficiencies
A deficiency in certain vitamins and minerals, particularly vitamin B12, iron, and folic acid, can lead to a higher incidence of mouth ulcers. Ensuring a balanced diet rich in fruits, vegetables, and whole grains is crucial. If you suspect a deficiency, a blood test can help determine the extent and guide supplementation.
- Iron deficiency anemia is a common cause of mouth ulcers and fatigue.
- B vitamins (B12, B9 (folic acid)) play vital roles in cell growth and repair.
- Consult a doctor or dietitian to assess your nutritional status and address any deficiencies.
Injury or Irritation
Accidental biting or injury to the mouth's lining, such as from sharp tooth edges, ill-fitting dentures, or even aggressive brushing, can easily trigger a mouth ulcer. Similarly, irritation from certain foods (e.g., acidic fruits, spicy foods) or mouthwashes can also contribute. Identifying and avoiding these irritants can be a simple solution.
- Examine your toothbrush: Make sure the bristles aren't too hard.
- Check your dentures or braces: Ensure they fit properly and aren't causing trauma.
- Avoid irritating foods: Pay attention to foods that seem to worsen the ulcers.
Underlying Medical Conditions
In some cases, mouth ulcers can be a symptom of an underlying medical condition such as inflammatory bowel disease (IBD), celiac disease, or certain autoimmune disorders. While less common, it's important to rule out more serious causes if the ulcers are recurrent, persistent, or accompanied by other symptoms. Medical evaluation may be necessary.
- Recurrent or persistent ulcers warrant a visit to a doctor.
- Other symptoms (fatigue, weight loss, digestive issues) should be reported.
- Medical testing may be required to diagnose underlying conditions.
Certain Medications
Some medications, particularly those that affect the immune system, can increase your susceptibility to mouth ulcers. Certain chemotherapy drugs or immunosuppressants are examples. If you suspect a medication side effect, consult your doctor or pharmacist to discuss alternative options or management strategies. It's crucial to never discontinue a medication on your own.
- Review your current medications with a pharmacist or doctor.
- Discuss potential side effects and strategies for managing them.
- Never stop taking prescribed medications without consulting a healthcare provider.
Are mouth ulcers caused by stress?
The relationship between stress and mouth ulcers (aphthous ulcers) is complex and not fully understood. While stress is not directly causative of mouth ulcers, it's widely considered a significant trigger or exacerbating factor for many individuals. The exact mechanism isn't clear, but stress can weaken the immune system, making individuals more susceptible to various infections and inflammations, including mouth ulcers. Furthermore, stress can lead to changes in oral hygiene practices and habits (such as neglecting brushing or biting nails), which can further contribute to the development or worsening of ulcers. It's important to note that other factors, such as nutritional deficiencies, hormonal changes, and certain medical conditions, also play a role in causing mouth ulcers. Therefore, while stress might not be the root cause in all cases, it frequently plays a significant role in their onset and severity.
Stress and the Immune System's Role in Mouth Ulcers
The body's immune response plays a crucial role in the development and healing of mouth ulcers. Stress significantly impacts the immune system, often suppressing its function. A weakened immune system is less effective at fighting off infections and inflammation, making individuals more vulnerable to mouth ulcer development. This immune suppression isn't a direct cause of the ulcers themselves, but it's a significant factor influencing their likelihood and severity.
- Immune suppression: Stress hormones like cortisol can suppress immune cell activity.
- Increased vulnerability: A compromised immune system is more susceptible to various infections and inflammation.
- Delayed healing: A weakened immune system can lead to slower healing of existing ulcers.
Stress-Induced Behaviors and Mouth Ulcers
Stress can lead to behavioral changes that directly affect oral health and increase the risk of mouth ulcers. Many people under stress exhibit behaviors such as neglecting oral hygiene, biting their nails, or clenching their jaws. These actions can directly damage the delicate tissues in the mouth, creating lesions or exacerbating existing ulcers.
- Neglect of oral hygiene: Insufficient brushing and flossing allow bacteria to thrive.
- Nail-biting: Introduces bacteria and causes direct trauma to the mouth.
- Jaw clenching: Creates friction and irritation, potentially leading to ulcer formation.
The Link Between Stress and Other Mouth Ulcer Triggers
Stress can indirectly influence other factors known to trigger mouth ulcers. For example, stress can disrupt sleep patterns, leading to nutritional deficiencies that weaken the immune system. Similarly, stress can exacerbate existing conditions like vitamin B12 deficiency or iron deficiency, which are known to be linked to an increased susceptibility to mouth ulcers. Therefore, stress isn't just a direct trigger but also influences many contributing factors.
- Sleep deprivation: Affects immune function and overall health.
- Nutritional deficiencies: Stress can lead to poor dietary habits and nutrient imbalances.
- Exacerbation of existing conditions: Stress can worsen underlying health issues.
Managing Stress to Reduce Mouth Ulcer Frequency
While stress might not be the sole cause, managing stress levels can significantly reduce the frequency and severity of mouth ulcers for many people. Strategies like regular exercise, mindfulness practices, sufficient sleep, and stress-reduction techniques can positively impact both overall health and the immune system, potentially lessening the incidence of mouth ulcer occurrences.
- Exercise: Physical activity improves immune function and reduces stress hormones.
- Mindfulness and meditation: Help manage stress and promote relaxation.
- Adequate sleep: Crucial for immune function and overall well-being.
When to Seek Medical Advice for Mouth Ulcers
While many mouth ulcers resolve on their own, it’s important to seek medical attention if ulcers are unusually large, persistent (lasting longer than two weeks), painful, or accompanied by other symptoms such as fever, swollen lymph nodes, or difficulty swallowing. A healthcare professional can properly diagnose the cause of the ulcers and recommend appropriate treatment, particularly if the ulcers are recurring or unusually severe. They can also assess if underlying health conditions are contributing to the problem.
- Persistent ulcers: Ulcers lasting longer than two weeks warrant medical attention.
- Severe pain or discomfort: Intense pain may indicate an underlying condition.
- Accompanying symptoms: Fever, swollen glands, and difficulty swallowing require medical evaluation.
Do mouth ulcers mean you are run down?
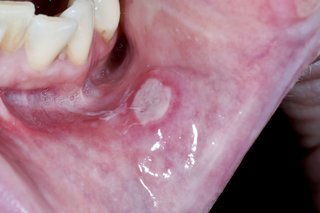
Mouth ulcers, also known as aphthous ulcers or canker sores, are small, painful sores that develop inside the mouth. While a correlation exists between mouth ulcers and feeling run down, it's not a direct cause-and-effect relationship. Feeling run down, or experiencing reduced physical and mental energy, often reflects an underlying issue, and this can sometimes weaken the immune system, making you more susceptible to various infections, including those leading to mouth ulcers. However, many factors can trigger mouth ulcers, and being tired is only one of them. The exact cause of mouth ulcers is still not fully understood, but several contributing factors are frequently identified, including stress, nutritional deficiencies (especially iron, vitamin B12, and folic acid), hormonal changes, and even minor trauma to the mouth. Therefore, while having mouth ulcers mightindicate you're run down, it's not a definitive diagnosis. It's crucial to consider other symptoms and consult a doctor or dentist for a proper assessment.
What are the typical symptoms of being run down?
Feeling run down is a subjective experience, but common symptoms can include persistent fatigue, lack of energy, difficulty concentrating, impaired memory, irritability, mood changes, and a weakened immune system, leading to frequent infections. These symptoms can be a sign of several underlying conditions, such as chronic stress, inadequate sleep, poor diet, underlying medical conditions, or even depression and anxiety. It's important to note that experiencing some of these symptoms occasionally isn't necessarily a cause for concern, but persistent symptoms should prompt a visit to a healthcare professional for assessment and diagnosis.
- Persistent Fatigue: A feeling of tiredness that doesn't improve with rest.
- Impaired Concentration: Difficulty focusing or remembering things.
- Weakened Immune System: Increased susceptibility to colds, flu, and other infections.
What are the different types of mouth ulcers?
Mouth ulcers come in various forms, depending on their size, location, and duration. Minor aphthous ulcers are the most common type, small (less than 1cm), and heal within 1-2 weeks. Major aphthous ulcers are larger (more than 1cm), deeper, and take longer to heal (often several weeks). Herpetiform ulcers are tiny and numerous, resembling cold sores but are not caused by the herpes simplex virus. The type of mouth ulcer can offer clues to potential underlying issues. However, proper diagnosis requires professional examination.
- Minor Aphthous Ulcers: Small, shallow sores that heal quickly.
- Major Aphthous Ulcers: Larger, deeper sores that take longer to heal.
- Herpetiform Ulcers: Numerous small sores that may be clustered.
What other factors can trigger mouth ulcers?
Beyond being run down, many other factors can contribute to the development of mouth ulcers. Stress is a significant trigger for many individuals, as are nutritional deficiencies, particularly in iron, B vitamins, and folic acid. Hormonal changes, especially in women, can also influence ulcer formation. Minor injuries to the mouth, such as biting your cheek or tongue, can also initiate ulcer development. Certain medical conditions and medications can also be associated with mouth ulcers. Identifying these contributing factors can help manage future occurrences.
- Stress: Both physical and emotional stress can trigger mouth ulcers.
- Nutritional Deficiencies: Lack of essential vitamins and minerals.
- Minor Trauma: Accidental injuries inside the mouth.
When should you see a doctor about mouth ulcers?
While most mouth ulcers heal on their own within a couple of weeks, it's essential to seek medical attention under certain circumstances. Persistent or recurring ulcers that don't improve with over-the-counter treatments warrant a consultation. Large or deep ulcers, accompanied by fever or other systemic symptoms, also require prompt medical evaluation. Ulcers that are resistant to home treatment or are causing significant pain or discomfort are further reasons to seek professional advice. A doctor or dentist can provide a proper diagnosis and rule out more serious conditions.
- Persistent or recurring ulcers: Ulcers that last for more than two weeks or keep reappearing.
- Large or deep ulcers: Ulcers that are unusually large or extend deep into the tissue.
- Accompanying symptoms: Fever, fatigue, or other systemic symptoms.
How are mouth ulcers treated?
Treatment for mouth ulcers often focuses on pain relief and promoting healing. Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help manage pain and inflammation. Topical treatments, including mouthwashes and gels containing corticosteroids or anesthetics, can provide additional relief and accelerate healing. In some cases, a doctor might prescribe stronger medications. Maintaining good oral hygiene is crucial for preventing infection and promoting healing. Addressing underlying conditions, like nutritional deficiencies or stress, is also vital in managing recurring ulcers.
- Over-the-counter pain relievers: To manage pain and inflammation.
- Topical treatments: Gels, mouthwashes, and creams to relieve pain and promote healing.
- Good oral hygiene: Regular brushing and flossing to maintain oral health.
What causes mouth ulcers to flare up?

What Causes Mouth Ulcers to Flare Up?
Mouth ulcers, also known as aphthous ulcers or canker sores, are small, painful sores that develop inside the mouth. While the exact cause isn't fully understood, several factors can trigger a flare-up. These range from minor irritations to underlying medical conditions. The interplay of these factors often contributes to the development of mouth ulcers, making it difficult to pinpoint a single cause in many cases. Stress, dietary deficiencies, and certain medical conditions are frequently implicated, highlighting the complexity of this common oral problem.
Stress and Anxiety
Stress and anxiety are frequently cited triggers for mouth ulcer flare-ups. While the exact mechanism isn't fully elucidated, the body's stress response can impact the immune system, potentially making individuals more susceptible to ulcer development. Chronic stress seems to be particularly problematic. Managing stress levels through techniques such as yoga, meditation, or regular exercise might help reduce the frequency of outbreaks.
- Increased cortisol levels associated with stress can weaken the immune system.
- Stress can disrupt the balance of beneficial bacteria in the mouth.
- Stress can lead to changes in sleep patterns and habits, potentially affecting immune function.
Dietary Factors
Certain foods and deficiencies can contribute to mouth ulcer flare-ups. Dietary deficiencies, especially in iron, vitamin B12, folate, and zinc, are linked to an increased risk. Also, some individuals find that acidic or spicy foods trigger their ulcers. Keeping a food diary can help identify potential triggers. Maintaining a balanced and nutritious diet is crucial in preventing recurrences.
- Iron deficiency is often associated with recurrent mouth ulcers.
- Vitamin B12 deficiency can also lead to increased vulnerability.
- Consuming plenty of fruits and vegetables rich in vitamins and minerals is important.
Immune System Dysfunction
Mouth ulcers are often associated with changes in the immune system. While not always directly causal, a compromised immune system may make individuals more vulnerable to ulcer development. This might be due to underlying conditions or even just temporary immune suppression. Addressing any underlying immune deficiencies is essential for long-term management.
- Autoimmune diseases can sometimes be linked to recurrent mouth ulcers.
- Certain medications that suppress the immune system can increase the risk.
- Infections can also weaken the immune system, leading to increased susceptibility.
Trauma to the Mouth
Minor injuries to the mouth, such as accidental biting, brushing too hard, or ill-fitting dentures can all irritate the oral mucosa and lead to the formation of ulcers. Protecting the mouth from such trauma is crucial. This is especially important for people who tend to develop mouth ulcers frequently. Using a soft-bristled toothbrush and avoiding sharp foods can help.
- Accidental biting of the cheek or lip is a common cause.
- Poorly fitting dentures can cause constant irritation.
- Using a mouthwash with alcohol can dry out the mouth and increase irritation.
Certain Medical Conditions
Some underlying medical conditions, such as inflammatory bowel disease (IBD), Crohn's disease, and celiac disease, are often associated with recurrent mouth ulcers. These conditions involve chronic inflammation throughout the body, which may increase the susceptibility to ulcer development in the mouth. It’s important to consult a doctor if mouth ulcers are frequent or severe, as they may be a sign of a more serious underlying health problem.
- Inflammatory bowel disease (IBD) is strongly linked to mouth ulcer development.
- Crohn's disease shares similar associations with mouth ulcer frequency.
- Celiac disease can also trigger recurrent mouth ulcers due to its systemic inflammatory nature.
Why have I suddenly developed mouth ulcers?
The sudden appearance of mouth ulcers, also known as aphthous ulcers or canker sores, can be frustrating and painful. There's no single, definitive answer, as several factors can contribute to their development. Stress is a very common trigger. When you're stressed, your immune system can be weakened, making you more susceptible to these sores. Minor trauma to the mouth, such as biting your cheek accidentally or irritating your mouth with rough food or a toothbrush, can also initiate an ulcer. Dietary deficiencies, particularly in iron, vitamin B12, and folic acid, can play a role. Certain medical conditions, including inflammatory bowel disease (IBD) and celiac disease, are associated with a higher incidence of mouth ulcers. Furthermore, some individuals are simply genetically predisposed to developing them more frequently. Finally, some medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or chemotherapy drugs, can cause mouth ulcers as a side effect. If you're experiencing recurrent or unusually severe mouth ulcers, it's advisable to consult a dentist or doctor to rule out underlying medical conditions and receive appropriate treatment.
What can I do to treat a sudden mouth ulcer?
While many mouth ulcers heal on their own within a week or two, there are several things you can do to ease the discomfort and speed up the healing process. Over-the-counter pain relievers like ibuprofen or acetaminophen can help manage the pain. Rinsing your mouth several times a day with a warm saltwater solution (1/2 teaspoon of salt in 8 ounces of warm water) can help clean the area and reduce inflammation. Avoid acidic, spicy, or excessively hot foods and drinks, as these can irritate the ulcer. Applying a topical anesthetic gel or mouthwash containing benzocaine or lidocaine can provide temporary pain relief. Using a soft-bristled toothbrush and being gentle when brushing your teeth is crucial to avoid further irritation. Some individuals find relief from applying a topical corticosteroid cream or gel, but this should only be done after consulting a healthcare professional. For persistent or severe ulcers, a doctor or dentist can provide stronger treatments, such as prescription-strength mouthwashes or topical corticosteroids.
Are mouth ulcers contagious?
No, mouth ulcers are not contagious. They are not caused by viruses or bacteria that can spread from person to person. Unlike cold sores (which are caused by the herpes simplex virus), canker sores are a result of various factors, including stress, trauma, and underlying health conditions, as explained previously. Therefore, you don't need to worry about spreading them to others through kissing or sharing utensils. However, it's always good practice to maintain good hygiene habits, such as regular handwashing, to prevent the spread of other infections.
When should I see a doctor about my mouth ulcer?
While many mouth ulcers heal without medical intervention, there are certain circumstances where seeking professional help is crucial. If your ulcer is extremely painful, persists for more than two weeks, is unusually large, or occurs frequently, you should consult a doctor or dentist. This is particularly important if you also experience fever, swollen lymph nodes, or other symptoms. Your doctor can help determine the underlying cause of your mouth ulcers and rule out more serious conditions. They may conduct tests to check for deficiencies or other health issues. A doctor can also provide more aggressive treatments if necessary, and ensure that the cause of the ulcers is properly addressed.
Deja una respuesta