Why do I keep getting mouth ulcers

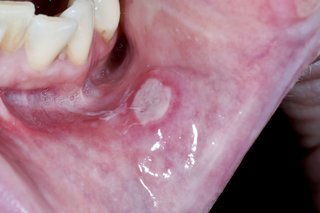
Mouth ulcers, also known as canker sores, are a common and often painful problem that can affect people of all ages. While they are usually harmless and will resolve on their own within a few weeks, they can be uncomfortable and interfere with everyday activities such as eating, drinking, and talking. If you frequently experience mouth ulcers, it is important to understand the potential causes and triggers to help prevent them from recurring.
Recurring Mouth Ulcers: Understanding the Causes
Mouth ulcers, also known as aphthous ulcers or canker sores, are small, painful sores that develop inside the mouth. While a single ulcer might heal within a week or two, recurring mouth ulcers can be frustrating and debilitating. Several factors contribute to their recurrence, and identifying the underlying cause is crucial for effective management.
Stress as a Trigger for Mouth Ulcers
Stress is a significant contributing factor to the development of mouth ulcers. When you're stressed, your body releases hormones that can weaken your immune system, making you more susceptible to infections, including those that might trigger mouth ulcers. Managing stress through techniques like yoga, meditation, or deep breathing exercises can help reduce the frequency of outbreaks. Furthermore, ensuring adequate sleep and incorporating stress-reducing activities into your daily routine are key.
Nutritional Deficiencies and Mouth Ulcers
Nutritional deficiencies, particularly in vitamin B12, folic acid, and iron, are strongly linked to recurrent mouth ulcers. These vitamins and minerals play a vital role in maintaining healthy tissues and a robust immune system. A balanced diet rich in fruits, vegetables, and whole grains is crucial. If you suspect a deficiency, consult a doctor for blood tests and potential supplementation. Paying attention to your diet is a proactive approach to reducing ulcer frequency.
Underlying Medical Conditions and Mouth Ulcers
Certain medical conditions can increase your risk of developing mouth ulcers. These include inflammatory bowel disease (IBD), Celiac disease, and Behçet's disease. If you experience frequent mouth ulcers alongside other symptoms, it's crucial to consult a doctor to rule out any underlying medical issues. Early diagnosis and treatment of these conditions can significantly improve your overall health and reduce mouth ulcer frequency.
Allergies and Irritants: A Cause of Mouth Ulcers
Food allergies or sensitivities, as well as exposure to irritants like acidic foods (e.g., citrus fruits), certain toothpastes, or mouthwashes containing chemicals like sodium lauryl sulfate (SLS), can trigger mouth ulcers. Identifying and eliminating these triggers from your diet and oral hygiene routine is vital. Keeping a food diary can help pinpoint specific culprits. Switching to SLS-free toothpaste or mouthwash can also be beneficial.
Trauma and Injury: Mouth Ulcer Triggers
Minor injuries to the inside of your mouth, such as accidental biting, burns from hot food or drinks, or even poorly fitting dentures, can cause mouth ulcers. Being mindful of what you eat and drink, avoiding harsh foods, and ensuring your dentures fit properly can help prevent these injuries and reduce the likelihood of developing ulcers. Gentle oral care is essential to minimize trauma.
| Potential Cause | Symptoms | Treatment/Prevention |
|---|---|---|
| Stress | Recurring mouth ulcers, often alongside other stress-related symptoms | Stress management techniques, adequate sleep |
| Nutritional Deficiencies | Mouth ulcers, fatigue, weakness | Dietary changes, supplementation (if needed) |
| Underlying Medical Conditions | Mouth ulcers, other symptoms related to the specific condition | Medical diagnosis and treatment |
| Allergies/Irritants | Mouth ulcers after consuming specific foods or using certain products | Identify and avoid triggers |
| Trauma | Mouth ulcers following injury to the mouth | Careful eating, proper dental care |
Recurring Mouth Ulcers: Understanding the Causes
Mouth ulcers, also known as aphthous ulcers or canker sores, are small, painful sores that develop inside the mouth. While a single ulcer might heal within a week or two, recurring mouth ulcers can be frustrating and debilitating. Several factors contribute to their recurrence, and identifying the underlying cause is crucial for effective management.
Stress as a Trigger for Mouth Ulcers
Stress is a significant contributing factor to the development of mouth ulcers. When you're stressed, your body releases hormones that can weaken your immune system, making you more susceptible to infections, including those that might trigger mouth ulcers. Managing stress through techniques like yoga, meditation, or deep breathing exercises can help reduce the frequency of outbreaks. Furthermore, ensuring adequate sleep and incorporating stress-reducing activities into your daily routine are key.
Nutritional Deficiencies and Mouth Ulcers
Nutritional deficiencies, particularly in vitamin B12, folic acid, and iron, are strongly linked to recurrent mouth ulcers. These vitamins and minerals play a vital role in maintaining healthy tissues and a robust immune system. A balanced diet rich in fruits, vegetables, and whole grains is crucial. If you suspect a deficiency, consult a doctor for blood tests and potential supplementation. Paying attention to your diet is a proactive approach to reducing ulcer frequency.
Underlying Medical Conditions and Mouth Ulcers
Certain medical conditions can increase your risk of developing mouth ulcers. These include inflammatory bowel disease (IBD), Celiac disease, and Behçet's disease. If you experience frequent mouth ulcers alongside other symptoms, it's crucial to consult a doctor to rule out any underlying medical issues. Early diagnosis and treatment of these conditions can significantly improve your overall health and reduce mouth ulcer frequency.
Allergies and Irritants: A Cause of Mouth Ulcers
Food allergies or sensitivities, as well as exposure to irritants like acidic foods (e.g., citrus fruits), certain toothpastes, or mouthwashes containing chemicals like sodium lauryl sulfate (SLS), can trigger mouth ulcers. Identifying and eliminating these triggers from your diet and oral hygiene routine is vital. Keeping a food diary can help pinpoint specific culprits. Switching to SLS-free toothpaste or mouthwash can also be beneficial.
Trauma and Injury: Mouth Ulcer Triggers
Minor injuries to the inside of your mouth, such as accidental biting, burns from hot food or drinks, or even poorly fitting dentures, can cause mouth ulcers. Being mindful of what you eat and drink, avoiding harsh foods, and ensuring your dentures fit properly can help prevent these injuries and reduce the likelihood of developing ulcers. Gentle oral care is essential to minimize trauma.
| Potential Cause | Symptoms | Treatment/Prevention |
|---|---|---|
| Stress | Recurring mouth ulcers, often alongside other stress-related symptoms | Stress management techniques, adequate sleep |
| Nutritional Deficiencies | Mouth ulcers, fatigue, weakness | Dietary changes, supplementation (if needed) |
| Underlying Medical Conditions | Mouth ulcers, other symptoms related to the specific condition | Medical diagnosis and treatment |
| Allergies/Irritants | Mouth ulcers after consuming specific foods or using certain products | Identify and avoid triggers |
| Trauma | Mouth ulcers following injury to the mouth | Careful eating, proper dental care |
Why am I getting mouth ulcers frequently?
Frequent mouth ulcers, also known as aphthous ulcers or canker sores, can be a frustrating and painful experience. The exact cause isn't always clear, but several factors can contribute to their recurrence. These range from minor irritations to underlying medical conditions. It's crucial to see a dentist or doctor if you experience frequent or unusually severe mouth ulcers to rule out any serious underlying issues. Self-treating may mask a more significant problem.
Stress and Anxiety
Stress and anxiety are significant triggers for many individuals. When the body is under duress, the immune system can become compromised, making it more susceptible to infections and inflammation, including the development of mouth ulcers. Managing stress through techniques like exercise, yoga, meditation, or therapy can be beneficial.
- Stress reduction techniques: Regular exercise, mindfulness practices, sufficient sleep.
- Professional help: Consider therapy or counseling to address underlying anxiety.
- Lifestyle adjustments: Prioritize activities that promote relaxation and well-being.
Nutritional Deficiencies
Deficiencies in certain vitamins and minerals, such as iron, vitamin B12, folic acid, and zinc, can weaken the immune system and increase the likelihood of mouth ulcer development. A balanced diet rich in these nutrients is crucial for preventing recurrences. If you suspect a deficiency, consider consulting a doctor for testing and potential supplementation.
- Iron-rich foods: Red meat, spinach, lentils.
- B12 sources: Meat, poultry, fish, dairy products.
- Folic acid sources: Leafy green vegetables, citrus fruits, beans.
- Zinc-rich foods: Oysters, red meat, nuts, seeds.
Immune System Issues
A weakened or compromised immune system may make you more prone to developing mouth ulcers. This can be due to various factors, including autoimmune diseases, HIV/AIDS, or even prolonged stress. If mouth ulcers are accompanied by other symptoms of immune deficiency, it's important to seek medical attention for proper diagnosis and management.
- Underlying medical conditions: Regular check-ups with your doctor are vital.
- Immune system support: A healthy lifestyle contributes to a strong immune response.
- Medication review: Certain medications can suppress the immune system.
Oral Hygiene and Trauma
Poor oral hygiene can contribute to the development of mouth ulcers, as bacteria and irritants accumulate. Similarly, accidental injuries to the mouth, such as biting your cheek or lip, can also trigger ulcer formation. Maintaining excellent oral hygiene and avoiding mouth injuries are essential preventative measures.
- Regular brushing and flossing: At least twice a day.
- Gentle brushing: Avoid harsh scrubbing.
- Mouthwash use (as directed): Can help reduce bacteria.
- Avoid hard foods: Protect the delicate tissues in your mouth.
Certain Medications and Allergies
Some medications, particularly those that affect the immune system or cause dry mouth, may increase the risk of mouth ulcers. Likewise, allergies to certain foods or substances can trigger an inflammatory response in the mouth, resulting in ulcer formation. If you suspect a medication or food allergy is contributing to your mouth ulcers, consult a doctor or allergist.
- Medication review: Discuss potential side effects with your prescribing physician.
- Allergy testing: Identify and avoid potential triggers.
- Dietary adjustments: Eliminate suspected allergenic foods from your diet.
What am I deficient in if I keep getting mouth ulcers?

Recurring mouth ulcers, also known as aphthous ulcers or canker sores, can be a sign of several underlying deficiencies. While the exact cause isn't always clear, several nutritional deficiencies are frequently linked to their development. It's crucial to note that this is not an exhaustive list, and other factors like stress, injury, or certain medical conditions can also play a role. A proper diagnosis from a healthcare professional is essential to determine the underlying cause of your recurring mouth ulcers.
Vitamin B12 Deficiency
Vitamin B12 is crucial for healthy cell growth and function, including the cells lining your mouth. A deficiency can manifest in various ways, and recurring mouth ulcers are one potential symptom. Without sufficient B12, your body struggles to repair damaged tissues, leading to prolonged healing times and increased susceptibility to ulcers. Other symptoms of B12 deficiency can include fatigue, anemia, and neurological problems. A blood test can easily confirm a B12 deficiency.
- Fatigue and Weakness: Feeling constantly tired and lacking energy.
- Pernicious Anemia: A type of anemia caused by the body's inability to absorb B12.
- Neurological Symptoms: Numbness, tingling, or even cognitive difficulties.
Iron Deficiency
Iron is a vital component of hemoglobin, which carries oxygen throughout the body. Iron deficiency anemia can impair the body's ability to repair tissues, increasing the likelihood of mouth ulcers. The lack of sufficient iron can also weaken the immune system, making you more vulnerable to infections that might exacerbate the ulcers. Symptoms beyond mouth ulcers include fatigue, pale skin, shortness of breath, and brittle nails.
- Pale Skin and Mucous Membranes: Noticeably lighter than usual skin tone.
- Shortness of Breath: Difficulty breathing, even with minimal exertion.
- Brittle Nails: Nails that are easily broken or cracked.
Folic Acid Deficiency
Folic acid, a B vitamin, is essential for cell growth and development. A deficiency can interfere with the body's ability to repair damaged tissues, including those in the mouth, leading to recurrent ulcers. Folic acid is crucial during cell division, and a deficiency can impact the healing process of mouth ulcers. Other deficiency symptoms can include fatigue, anemia, and neurological problems.
- Megaloblastic Anemia: A type of anemia characterized by abnormally large red blood cells.
- Gastrointestinal Issues: Diarrhea, constipation, or other digestive problems.
- Developmental Issues: In pregnant women, a deficiency can cause neural tube defects in the developing fetus.
Zinc Deficiency
Zinc plays a vital role in immune function and wound healing. A deficiency can impair the body's ability to fight infections and repair damaged tissues, potentially leading to more frequent and persistent mouth ulcers. Zinc also supports the integrity of the mucous membranes lining the mouth, making a deficiency a possible contributor to ulcer formation. Other symptoms can include hair loss, skin rashes, and impaired taste and smell.
- Impaired Wound Healing: Slower than usual healing of cuts and scrapes.
- Loss of Appetite: Reduced desire to eat.
- Delayed Growth and Development: Especially in children.
Vitamin C Deficiency
Vitamin C is an essential antioxidant and plays a vital role in collagen production, crucial for tissue repair and maintaining the integrity of blood vessels. While not as strongly linked to mouth ulcers as other deficiencies, a severe Vitamin C deficiency (scurvy) can lead to impaired wound healing, increased susceptibility to infections, and the development of mouth ulcers. Other symptoms include bleeding gums, easy bruising, and fatigue.
- Bleeding Gums: Gums that bleed easily during brushing or flossing.
- Joint Pain: Aches and pains in the joints.
- Easy Bruising: Bruising with minimal trauma.
Do mouth ulcers mean you are run down?
Mouth ulcers, also known as aphthous ulcers or canker sores, are small, shallow lesions that develop on the soft tissues in your mouth. While a common occurrence, their exact cause remains unclear. However, a weakened immune system, often associated with being "run down" or experiencing physical or emotional stress, is frequently linked to their appearance. A run-down state can manifest in various ways, impacting your body's ability to fight off infections and heal minor injuries, like those causing mouth ulcers. This doesn't mean that everymouth ulcer indicates being run down, but it's a factor often cited in their formation. Other potential triggers include nutritional deficiencies, hormonal changes, and even certain foods or dental appliances. Therefore, while a correlation exists, it's crucial to consider other potential causes before solely attributing mouth ulcers to being run down.
What is "being run down"?
Being "run down" is a general term describing a state of low energy, fatigue, and reduced overall well-being. It signifies that your body is not functioning optimally. This can stem from various factors, including:
- Lack of sleep: Chronic sleep deprivation weakens the immune system, making you more susceptible to infections and slower to heal.
- Poor diet: Insufficient intake of essential vitamins and minerals can impact immune function and overall health.
- Stress: Both physical and emotional stress can significantly weaken the immune response, potentially leading to the development of mouth ulcers.
The Link Between Immune System and Mouth Ulcers
Your immune system plays a crucial role in wound healing and fighting off infections, including those that might contribute to mouth ulcer formation. When you're run down, your immune system may be compromised, making you more prone to developing these ulcers. This is because the body's resources are diverted to other tasks, leaving less capacity to address the minor trauma that triggers mouth ulcers.
- A weakened immune system struggles to effectively combat minor infections or inflammation in the mouth.
- Delayed healing processes can lead to the formation and persistence of mouth ulcers.
- Underlying health conditions can compromise immunity, increasing the likelihood of mouth ulcers.
Other Potential Causes of Mouth Ulcers
It's important to remember that mouth ulcers aren't always solely caused by being run down. Several other factors can contribute to their development. These include:
- Nutritional deficiencies: Lack of iron, vitamin B12, or folic acid can increase the risk.
- Allergies or sensitivities: Certain foods, ingredients, or even dental products can trigger allergic reactions and mouth ulcers.
- Dental appliances: Ill-fitting dentures or braces can cause irritation, leading to ulcer formation.
When to Seek Medical Advice for Mouth Ulcers
Most mouth ulcers are harmless and resolve on their own within a week or two. However, persistent, unusually painful, or large ulcers should prompt a visit to a doctor or dentist. These could indicate an underlying medical condition that requires attention.
- Ulcers that don't heal after two weeks.
- Ulcers accompanied by fever, fatigue, or swollen lymph nodes.
- Recurrent ulcers that significantly impact your quality of life.
Managing Mouth Ulcers When Run Down
If you suspect your mouth ulcers are related to being run down, focusing on improving your overall health is crucial. This involves:
- Getting enough sleep: Aim for 7-9 hours of quality sleep per night.
- Eating a balanced diet: Include plenty of fruits, vegetables, and whole grains.
- Managing stress: Practice relaxation techniques like yoga, meditation, or deep breathing exercises.
What autoimmune disease causes mouth ulcers?

While many factors can cause mouth ulcers, there isn't one single autoimmune disease specifically and solely attributed to causing them. However, several autoimmune conditions can increase the likelihood or severity of mouth ulcers as a symptom. Behçet's disease is perhaps the most strongly associated autoimmune condition with recurrent and severe mouth ulcers. Other autoimmune diseases can indirectly contribute to mouth ulcers through inflammation or medication side effects.
Behçet's Disease and Mouth Ulcers
Behçet's disease is a rare, chronic inflammatory disorder that primarily affects blood vessels. A hallmark symptom of Behçet's disease is the development of recurrent and painful aphthous ulcers (mouth ulcers) in the mouth and genitals. These ulcers can be extremely painful and debilitating. The exact cause of Behçet's disease is unknown, but it's believed to have an autoimmune component where the body's immune system mistakenly attacks its own tissues. The frequency and severity of mouth ulcers are key diagnostic indicators of Behçet's disease.
- Recurrent Aphthous Stomatitis (RAS): While not strictly an autoimmune disease itself, RAS is characterized by recurrent mouth ulcers and some research suggests a possible autoimmune component in a subset of patients.
- Genetic predisposition: Behçet's disease has a strong genetic component, suggesting an underlying susceptibility to the immune system's misdirected attack.
- Diagnostic criteria: The diagnosis of Behçet's disease relies on a combination of symptoms including recurrent mouth ulcers, genital ulcers, and eye inflammation (uveitis).
Other Autoimmune Diseases and Mouth Ulcers
While not as directly linked as Behçet's disease, other autoimmune diseases can sometimes present with mouth ulcers as a symptom or a side effect of treatment. These include conditions like inflammatory bowel disease (IBD) (Crohn's disease and ulcerative colitis), systemic lupus erythematosus (SLE), and rheumatoid arthritis (RA). The ulcers in these cases are usually less severe and frequent compared to those seen in Behçet's disease, and are often overshadowed by the other symptoms of the primary disease.
- Inflammation: Systemic inflammation characteristic of many autoimmune diseases can affect the mucous membranes of the mouth, leading to ulcer formation.
- Medication side effects: Some medications used to treat autoimmune diseases can have mouth ulcers as a side effect.
- Immune dysregulation: The underlying immune dysfunction in these autoimmune diseases can contribute to a higher susceptibility to oral infections which can exacerbate ulcer formation.
The Role of Immune System Dysfunction
In autoimmune diseases, the immune system mistakenly attacks healthy tissues in the body. In the context of mouth ulcers, this can manifest as inflammation and damage to the oral mucosa. The precise mechanisms by which immune system dysfunction causes mouth ulcers vary depending on the specific autoimmune disease and its pathophysiology. However, a common feature is the presence of chronic inflammation that disrupts the integrity of the oral tissues.
- T-cell involvement: T-cells, a type of immune cell, are often implicated in the pathogenesis of autoimmune diseases and contribute to inflammation in various tissues, including the mouth.
- Cytokine release: Immune cells release cytokines, signaling molecules that contribute to inflammation and tissue damage in the mouth.
- Genetic factors: Genetic variations can influence the susceptibility to both autoimmune diseases and the development of mouth ulcers.
Diagnosing Autoimmune Disease-Related Mouth Ulcers
Diagnosing autoimmune disease-related mouth ulcers requires a comprehensive medical evaluation. This involves a thorough review of the patient's medical history, a physical examination, and various diagnostic tests. The diagnosis hinges on identifying the underlying autoimmune condition and determining if the mouth ulcers are a primary manifestation or a secondary symptom.
- Blood tests: Blood tests can help identify markers of inflammation and detect specific autoantibodies associated with various autoimmune diseases.
- Biopsies: In some cases, a biopsy of the ulcer may be necessary to rule out other conditions or confirm the diagnosis.
- Imaging studies: Imaging techniques such as ultrasound or MRI may be utilized to evaluate the extent of disease involvement in certain organs.
Treatment Options for Autoimmune Disease-Related Mouth Ulcers
Treatment focuses on managing the underlying autoimmune disease and alleviating the symptoms, including the mouth ulcers. This may involve various medications such as corticosteroids, immunosuppressants, or biologics. Treatment choices depend heavily on the specific diagnosis and severity of the condition. In addition to medication, supportive measures such as pain relief, mouthwashes, and dietary modifications can help manage the discomfort associated with mouth ulcers.
- Topical corticosteroids: These can reduce inflammation and pain in the mouth.
- Systemic corticosteroids: These are used for more severe cases of autoimmune disease and can suppress the immune system to reduce inflammation throughout the body.
- Immunosuppressants: These medications help to regulate the immune system and reduce its attack on healthy tissues.
What causes mouth ulcers?
Mouth ulcers, also known as aphthous ulcers or canker sores, are small, painful sores that develop inside the mouth. The exact cause of mouth ulcers remains unclear, but several factors are thought to contribute to their development. Stress is a commonly cited trigger, as are minor injuries to the mouth such as biting your cheek or accidentally scraping your gums. Certain foods, like acidic or spicy foods, can also irritate the mouth and trigger an outbreak. Nutritional deficiencies, particularly in iron, vitamin B12, and folic acid, have been linked to an increased risk of mouth ulcers. Some people experience mouth ulcers due to allergic reactions to certain foods or dental products, while others may have a genetic predisposition that makes them more susceptible. Hormonal changes, such as those experienced during menstruation, can also play a role. Finally, some underlying medical conditions, including inflammatory bowel disease, celiac disease, and Behçet's disease, are associated with a higher frequency of mouth ulcers. It's important to note that often, the precise trigger remains elusive, and many individuals experience recurrent ulcers without identifying a specific cause.
Why do I keep getting mouth ulcers, even when I think I’ve identified the cause and avoided it?
Even when you believe you’ve pinpointed a trigger for your mouth ulcers and taken steps to avoid it, they may still reappear. This is because the relationship between potential causes and the onset of mouth ulcers isn't always straightforward. While some people find that eliminating certain foods or managing stress significantly reduces their frequency, for others, the connection is less clear. Multiple factors may be at play simultaneously, making it difficult to isolate a single cause and eliminate it completely. For instance, even if you've avoided spicy food, stress or hormonal fluctuations could still trigger an outbreak. The body's immune response also plays a significant role. Even a minor irritation, seemingly unrelated to previous triggers, can cause an ulcer to form if your immune system is already somewhat compromised or experiencing a temporary imbalance. Furthermore, some underlying medical conditions might be contributing, even if they haven't been diagnosed. Therefore, while identifying and avoiding potential triggers is helpful, persistence of mouth ulcers despite such efforts doesn't necessarily indicate a failure to address the cause, but rather the complex nature of the condition itself.
How can I prevent recurring mouth ulcers?
Preventing recurrent mouth ulcers often involves a multi-pronged approach targeting several potential contributing factors. Stress management is crucial, as stress is strongly linked to the occurrence of mouth ulcers. Techniques such as yoga, meditation, or deep breathing exercises can help. Maintaining a healthy diet rich in essential vitamins and minerals, including iron, vitamin B12, and folic acid, can also minimize the risk. Consider incorporating foods known to be rich in these nutrients into your diet. Avoiding foods and drinks that irritate the mouth, such as acidic or spicy foods, along with hard or crunchy foods that might cause injury, can be helpful. Good oral hygiene, including regular brushing and flossing, helps prevent minor injuries and keeps the mouth clean and healthy, reducing the chance of infection. Gentle rinsing with a salt-water solution can sometimes soothe existing ulcers and might help prevent new ones. If you suspect a possible allergy to a particular food or dental product, eliminating it from your routine may reduce the frequency of ulcers. Finally, consulting a dentist or doctor is important, especially if the mouth ulcers are severe, persistent, or accompanied by other symptoms. They can rule out any underlying medical conditions and suggest appropriate treatment options.
When should I see a doctor about my mouth ulcers?
While many mouth ulcers resolve on their own within a few weeks, there are certain situations where it's essential to seek professional medical attention. Consult a doctor or dentist if your mouth ulcers are extremely painful, large in size, or bleed excessively. If the ulcers persist for longer than two weeks without showing any signs of healing, it's crucial to get them checked. Similarly, if you experience numerous ulcers simultaneously, it warrants a medical evaluation. If the ulcers are accompanied by other symptoms such as fever, swollen lymph nodes, fatigue, or joint pain, it’s vital to seek medical attention as these could indicate a more serious underlying condition. Finally, if you have a compromised immune system, or are experiencing a change in the characteristics of your mouth ulcers, consulting a doctor is necessary. Prompt medical evaluation can help identify and treat any underlying medical issue, ensuring appropriate and timely management of the condition.

Deja una respuesta