Can allergies cause lung damage

Allergies are a common problem, affecting millions of people worldwide. They occur when the immune system overreacts to a foreign substance, such as pollen, pet dander, or dust. In most cases, allergies cause mild symptoms, such as sneezing, a runny nose, and itchy eyes. However, in some cases, allergies can lead to more serious health problems, such as asthma and lung damage.
Can Allergies Cause Lung Damage?
While allergies themselves don't directly cause permanent lung damage in most cases, they can significantly impact lung health and, in severe instances, contribute to conditions that do cause damage. The key lies in understanding the type of allergic reaction and its severity. Mild allergic reactions, such as sneezing and a runny nose, are unlikely to cause lasting lung harm. However, more severe reactions can trigger inflammation and other processes that, if repeated or untreated, could have long-term effects.
Asthma and Allergies
A significant link exists between allergies and asthma. Allergic asthma is triggered by allergens like pollen, dust mites, pet dander, or mold. When someone with an allergy inhales these allergens, their airways become inflamed, leading to wheezing, coughing, shortness of breath, and chest tightness. Chronic, poorly controlled allergic asthma can cause long-term damage to the airways, including thickening of the airway walls and increased mucus production. This chronic inflammation can lead to irreversible changes in lung function over time.
Allergic Bronchopulmonary Aspergillosis (ABPA)
ABPA is a rare but serious lung condition affecting individuals with asthma or cystic fibrosis. It's caused by an allergic reaction to Aspergillus fumigatus, a common fungus found in the environment. This allergic reaction leads to significant inflammation and damage within the lungs, potentially resulting in bronchiectasis (widening of the airways) and permanent lung scarring. Early diagnosis and treatment are crucial to prevent further lung damage.
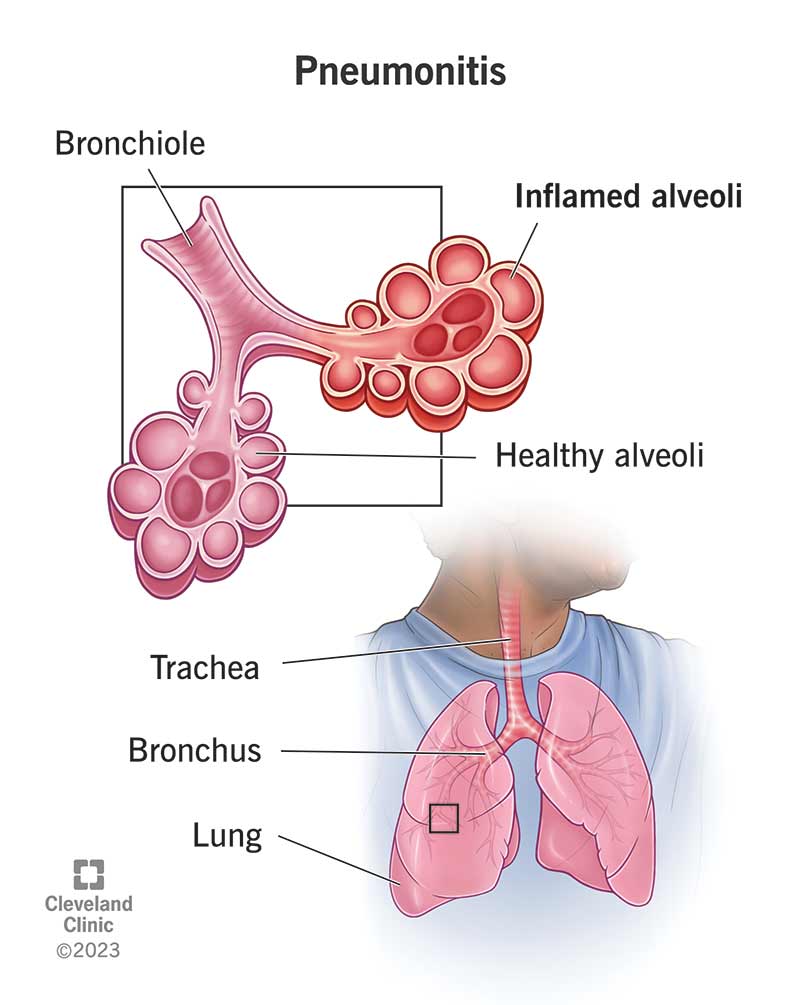
Hypersensitivity Pneumonitis
Hypersensitivity pneumonitis (HP) is an inflammatory lung disease triggered by inhaling specific organic dusts, such as mold spores, bird droppings, or dust from certain animals. The immune system's reaction to these inhalants causes inflammation in the alveoli (tiny air sacs in the lungs). If left untreated, HP can lead to fibrosis (scarring of the lung tissue), reduced lung function, and potentially respiratory failure. It's important to identify and avoid the offending allergen to prevent further damage.
Eosinophilic Lung Diseases
Eosinophils are a type of white blood cell that plays a role in allergic reactions. Several lung conditions, such as eosinophilic pneumonia and eosinophilic granulomatosis with polyangiitis (EGPA), are characterized by an excessive number of eosinophils in the lungs. These conditions can cause significant lung inflammation and, if severe, permanent lung damage. Treatment focuses on reducing eosinophil levels and managing inflammation.
Chronic Obstructive Pulmonary Disease (COPD) and Allergies
While not directly caused by allergies, some studies suggest a link between allergies and an increased risk of developing COPD. Allergies can contribute to airway inflammation, which may exacerbate the underlying inflammation associated with COPD, potentially speeding up the progression of the disease and leading to more severe lung function decline. More research is needed to fully understand this relationship.
| Condition | Mechanism of Lung Damage | Potential Consequences |
|---|---|---|
| Allergic Asthma | Chronic airway inflammation | Airway remodeling, reduced lung function |
| ABPA | Allergic reaction to Aspergillus fumigatus | Bronchiectasis, lung scarring |
| Hypersensitivity Pneumonitis | Inflammation in response to inhaled organic dusts | Fibrosis, reduced lung function, respiratory failure |
| Eosinophilic Lung Diseases | Excessive eosinophils in the lungs | Lung inflammation, permanent lung damage |
| COPD (Exacerbated by Allergies) | Increased airway inflammation | Accelerated lung function decline |
Can Allergies Cause Lung Damage?
While allergies themselves don't directly cause permanent lung damage in most cases, they can significantly impact lung health and, in severe instances, contribute to conditions that do cause damage. The key lies in understanding the type of allergic reaction and its severity. Mild allergic reactions, such as sneezing and a runny nose, are unlikely to cause lasting lung harm. However, more severe reactions can trigger inflammation and other processes that, if repeated or untreated, could have long-term effects.
Asthma and Allergies
A significant link exists between allergies and asthma. Allergic asthma is triggered by allergens like pollen, dust mites, pet dander, or mold. When someone with an allergy inhales these allergens, their airways become inflamed, leading to wheezing, coughing, shortness of breath, and chest tightness. Chronic, poorly controlled allergic asthma can cause long-term damage to the airways, including thickening of the airway walls and increased mucus production. This chronic inflammation can lead to irreversible changes in lung function over time.
Allergic Bronchopulmonary Aspergillosis (ABPA)
ABPA is a rare but serious lung condition affecting individuals with asthma or cystic fibrosis. It's caused by an allergic reaction to Aspergillus fumigatus, a common fungus found in the environment. This allergic reaction leads to significant inflammation and damage within the lungs, potentially resulting in bronchiectasis (widening of the airways) and permanent lung scarring. Early diagnosis and treatment are crucial to prevent further lung damage.
Hypersensitivity Pneumonitis
Hypersensitivity pneumonitis (HP) is an inflammatory lung disease triggered by inhaling specific organic dusts, such as mold spores, bird droppings, or dust from certain animals. The immune system's reaction to these inhalants causes inflammation in the alveoli (tiny air sacs in the lungs). If left untreated, HP can lead to fibrosis (scarring of the lung tissue), reduced lung function, and potentially respiratory failure. It's important to identify and avoid the offending allergen to prevent further damage.
Eosinophilic Lung Diseases
Eosinophils are a type of white blood cell that plays a role in allergic reactions. Several lung conditions, such as eosinophilic pneumonia and eosinophilic granulomatosis with polyangiitis (EGPA), are characterized by an excessive number of eosinophils in the lungs. These conditions can cause significant lung inflammation and, if severe, permanent lung damage. Treatment focuses on reducing eosinophil levels and managing inflammation.
Chronic Obstructive Pulmonary Disease (COPD) and Allergies
While not directly caused by allergies, some studies suggest a link between allergies and an increased risk of developing COPD. Allergies can contribute to airway inflammation, which may exacerbate the underlying inflammation associated with COPD, potentially speeding up the progression of the disease and leading to more severe lung function decline. More research is needed to fully understand this relationship.
| Condition | Mechanism of Lung Damage | Potential Consequences |
|---|---|---|
| Allergic Asthma | Chronic airway inflammation | Airway remodeling, reduced lung function |
| ABPA | Allergic reaction to Aspergillus fumigatus | Bronchiectasis, lung scarring |
| Hypersensitivity Pneumonitis | Inflammation in response to inhaled organic dusts | Fibrosis, reduced lung function, respiratory failure |
| Eosinophilic Lung Diseases | Excessive eosinophils in the lungs | Lung inflammation, permanent lung damage |
| COPD (Exacerbated by Allergies) | Increased airway inflammation | Accelerated lung function decline |
Can allergies permanently damage lungs?
Can Allergies Permanently Damage Lungs?
While allergies themselves don't directly cause permanent lung damage in most cases, severe and prolonged allergic reactions, particularly asthma triggered by allergies, can lead to long-term lung problems. The damage isn't a direct result of the allergen itself, but rather the body's inflammatory response. Repeated inflammation and bronchoconstriction can gradually affect lung structure and function, potentially leading to conditions like chronic obstructive pulmonary disease (COPD) or irreversible airway damage. The extent of the damage depends on several factors, including the severity and frequency of allergic reactions, the individual's genetic predisposition, and the effectiveness of treatment.
The Role of Asthma in Allergic Lung Damage
Asthma is a common condition often triggered by allergies. Untreated or poorly managed asthma can cause significant lung damage over time. Chronic inflammation in the airways leads to thickening of the airway walls, increased mucus production, and narrowing of the airways, making breathing difficult. This can result in permanent changes to lung function, including a reduction in lung capacity and increased susceptibility to respiratory infections.
- Airway Remodeling: Long-term inflammation leads to changes in the structure of the airways, including thickening of the walls and increased collagen deposition.
- Reduced Lung Function: The narrowing of the airways reduces airflow and decreases lung capacity, leading to shortness of breath and wheezing.
- Increased Susceptibility to Infections: Chronic inflammation weakens the lung's defense mechanisms, increasing the risk of respiratory infections like pneumonia and bronchitis.
Allergic Bronchopulmonary Aspergillosis (ABPA)
ABPA is a rare but serious allergic reaction to the fungus Aspergillus, often seen in individuals with asthma or cystic fibrosis. ABPA can cause significant lung damage, including bronchiectasis (permanent widening and scarring of the airways), and even lung tissue damage. Early diagnosis and treatment are crucial to minimize long-term lung damage. This condition highlights the potential for severe allergic responses to cause irreversible lung changes.
- Inflammation and Eosinophilia: The allergic response involves significant inflammation and an increase in eosinophils (a type of white blood cell).
- Bronchiectasis: Permanent dilation and scarring of the airways lead to chronic cough, excessive mucus production, and recurrent respiratory infections.
- Lung Function Decline: The damage to the airways and lung tissue results in a progressive decline in lung function.
The Impact of Allergic Rhinitis on Lung Health
While primarily affecting the nose and sinuses, allergic rhinitis (hay fever) can have indirect effects on the lungs. Chronic inflammation and nasal congestion associated with rhinitis may contribute to increased airway reactivity and worsen existing asthma. Although not directly causing lung damage, it can exacerbate pre-existing lung conditions and make individuals more susceptible to respiratory infections. The interplay between upper and lower airway inflammation is an important consideration.
- Increased Airway Reactivity: Inflammation in the nose and sinuses can increase the sensitivity of the airways, making them more likely to constrict in response to triggers.
- Exacerbation of Asthma: Allergic rhinitis can worsen asthma symptoms and increase the frequency of asthma attacks.
- Postnasal Drip: Mucus dripping down the back of the throat can irritate the airways and trigger coughing and wheezing.
The Importance of Allergy Management in Preventing Lung Damage
Effective management of allergies is critical in preventing long-term lung damage. This involves strategies such as allergen avoidance, medication (such as antihistamines, corticosteroids, and leukotriene modifiers), and immunotherapy (allergy shots). Early diagnosis and treatment of allergic conditions, particularly asthma, are essential to minimize inflammation and prevent irreversible changes to the lungs. Regular monitoring of lung function and prompt treatment of exacerbations are also vital.
- Allergen Avoidance: Identifying and avoiding allergens is a fundamental approach to reducing exposure and minimizing inflammation.
- Medication: Various medications can help control allergic symptoms and reduce inflammation, thereby protecting the lungs.
- Immunotherapy: Allergy shots can desensitize the immune system to allergens, reducing the severity of allergic reactions.
How long does it take for lungs to recover from allergies?
:max_bytes(150000):strip_icc()/respiratory-allergies-symptoms-causes-and-treatment-5206183-5205177-final-7af9eb5916eb4a8dacf8b9bd516cad85.jpg)
The time it takes for lungs to recover from an allergic reaction varies greatly depending on several factors. There's no single definitive answer. The severity of the allergic reaction, the individual's overall health, the type of allergen, and the promptness and effectiveness of treatment all play significant roles. A mild allergic reaction, like some sneezing and a runny nose, might resolve within a few hours to a day or two. However, more severe reactions, such as asthma attacks triggered by allergies, can take much longer to subside. In cases of severe allergic reactions requiring medical intervention, such as anaphylaxis, recovery can take days, weeks, or even longer depending on the extent of lung involvement and the complications that arise. It's crucial to remember that even seemingly minor allergic reactions can have lingering effects on lung function if left unmanaged.
Severity of the Allergic Reaction
The severity of the allergic reaction significantly impacts recovery time. Mild allergic reactions, characterized by minor symptoms like sneezing, a runny nose, and mild coughing, usually resolve quickly. However, more severe reactions involving wheezing, shortness of breath, and difficulty breathing can necessitate medical intervention and take considerably longer to heal. The lungs' ability to fully recover depends on the extent of inflammation and the body's response to treatment. Severe allergic reactions, particularly anaphylaxis, might cause lasting lung damage requiring extended recovery and ongoing management.
- Mild reactions (sneezing, runny nose): Recovery in hours to days.
- Moderate reactions (wheezing, shortness of breath): Recovery in days to weeks.
- Severe reactions (anaphylaxis): Recovery can take weeks or even longer, possibly with lasting effects.
Type of Allergen
Different allergens can trigger varied responses in the lungs. Some allergens, like pollen, can cause relatively short-lived symptoms, while others, like certain mold spores or pet dander, may lead to more persistent lung irritation and inflammation. The specific allergen involved influences the duration and intensity of the inflammatory response, directly affecting recovery time. Identifying the specific allergen and minimizing exposure are crucial for managing symptoms and promoting faster recovery.
- Pollen allergies: Typically cause shorter-lived reactions.
- Mold allergies: Often lead to more persistent inflammation.
- Pet dander allergies: May cause chronic lung irritation.
Effectiveness of Treatment
Prompt and effective treatment is crucial in accelerating lung recovery from allergic reactions. Early intervention with antihistamines, decongestants, or bronchodilators can significantly reduce symptom duration and severity. For more severe reactions, corticosteroids or other medications may be necessary to control inflammation and improve lung function. The effectiveness of the chosen treatment directly impacts the speed of recovery and reduces the risk of long-term lung damage.
- Antihistamines: Help reduce inflammation and alleviate symptoms.
- Decongestants: Relieve nasal congestion and improve breathing.
- Corticosteroids: Control inflammation in severe cases.
Individual Health and Pre-existing Conditions
An individual's overall health and any pre-existing conditions, especially respiratory illnesses like asthma, significantly influence recovery time. Individuals with compromised immune systems or pre-existing lung conditions may experience more prolonged and severe allergic reactions. Their lungs may take longer to recover compared to healthy individuals. Managing underlying health conditions effectively is crucial for promoting faster recovery from allergic reactions.
- Asthma: Pre-existing asthma can worsen allergic reactions and prolong recovery.
- Compromised immune system: Weakened immunity can lead to more intense and prolonged reactions.
- Other respiratory illnesses: Existing lung issues can hinder recovery from allergic reactions.
How do you treat lung inflammation from allergies?
Treating lung inflammation (bronchitis or even, in severe cases, asthma) stemming from allergies focuses on reducing inflammation and managing allergy symptoms. This is a multi-pronged approach involving medication, lifestyle changes, and sometimes, allergy testing and immunotherapy. The severity of the inflammation dictates the treatment intensity. Mild inflammation might only require over-the-counter medications, while severe cases necessitate prescription drugs and potentially specialized medical care.
1. Identifying and Avoiding Allergens
The cornerstone of allergy-induced lung inflammation treatment is identifying and minimizing exposure to allergens. This requires pinpointing the specific substances triggering your reaction. Common culprits include pollen, dust mites, pet dander, mold, and certain foods. Once identified, you can take steps to reduce contact. This can involve significant lifestyle modifications.
- Allergy testing: Skin prick tests or blood tests can identify specific allergens.
- Environmental control: Regularly cleaning your home, using air purifiers with HEPA filters, encasing mattresses and pillows in allergen-proof covers, and avoiding exposure to pets or specific plants can minimize exposure.
- Dietary changes: If food allergies are suspected, an elimination diet guided by an allergist may be necessary.
2. Medication for Allergy Symptoms
Over-the-counter (OTC) and prescription medications play a vital role in managing allergy symptoms and reducing lung inflammation. These medications aim to suppress the immune system’s response to allergens.
- Antihistamines: These block the effects of histamine, a chemical released during an allergic reaction, reducing symptoms like sneezing, itching, and runny nose. They can also help with mild lung inflammation.
- Decongestants: These relieve nasal congestion. However, prolonged use can lead to rebound congestion.
- Corticosteroids (Inhaled or Oral): These potent anti-inflammatory drugs, available as inhalers (for asthma) or oral medications, are used for more severe lung inflammation. Inhaled corticosteroids are preferred for targeting the lungs directly, minimizing systemic side effects.
- Leukotriene modifiers: These medications block the action of leukotrienes, chemicals that contribute to inflammation and airway constriction in asthma and allergies.
3. Inhaled Medications for Lung Inflammation
For individuals with allergy-induced asthma or bronchitis, inhaled medications offer targeted relief. They deliver medication directly to the lungs, minimizing side effects compared to oral medications. Proper inhaler technique is crucial for effectiveness.
- Inhaled corticosteroids: These are the mainstay of asthma treatment, reducing inflammation in the airways.
- Bronchodilators: These relax the muscles around the airways, making breathing easier, particularly during an acute attack. They are often used in combination with corticosteroids.
- Combination inhalers: Many inhalers combine a corticosteroid and a bronchodilator for convenient, effective management.
4. Allergy Immunotherapy (Allergy Shots)
For persistent, severe allergies that significantly impact lung health, allergy immunotherapy (allergy shots) might be considered. This treatment gradually desensitizes the immune system to specific allergens over time, reducing allergic reactions.
- Subcutaneous immunotherapy (SCIT): This involves regular injections of increasing doses of allergen extracts administered by a healthcare professional.
- Sublingual immunotherapy (SLIT): This involves placing allergen extracts under the tongue daily. This is a newer method.
- Success rates: Immunotherapy is generally well-tolerated and effective in reducing the severity and frequency of allergic reactions, including those impacting the lungs.
5. Lifestyle Modifications and Supportive Measures
Beyond medication and allergy testing, lifestyle adjustments play a critical role in managing allergy-induced lung inflammation. These measures aim to reduce exposure to triggers and support respiratory health.
- Regular exercise: Improves lung function and overall health.
- Quit smoking: Smoking significantly worsens lung inflammation and respiratory health.
- Hydration: Drinking plenty of fluids helps thin mucus and makes it easier to clear from the lungs.
- Stress management: Stress can exacerbate allergic reactions, and techniques like yoga or meditation can help manage stress levels.
What are the symptoms of pulmonary allergies?
:max_bytes(150000):strip_icc()/respiratory-allergies-symptoms-causes-and-treatment-5206183-5205177-final-7af9eb5916eb4a8dacf8b9bd516cad85.jpg)
Pulmonary allergies, also known as allergic airway diseases, encompass a range of conditions where the lungs react to allergens. Symptoms vary widely in severity and presentation, depending on the specific allergen, the individual's sensitivity, and the type of allergic response. They can range from mild irritation to life-threatening reactions. Common symptoms often overlap with other respiratory illnesses, making accurate diagnosis crucial.
1. Cough
A persistent cough is a hallmark symptom of pulmonary allergies. It can be dry or produce mucus (phlegm), often described as being thick and sticky. The cough may be worse at night or in the early morning, triggered by exposure to allergens or irritants. The severity of the cough can range from a mild tickle to a severe, debilitating episode. This cough is often not relieved by typical cough suppressants.
- Persistent, dry or productive cough
- Worse at night or early morning
- Not relieved by over-the-counter cough medications
2. Wheezing and Shortness of Breath
Wheezing, a whistling sound during breathing, is a characteristic sign of airway narrowing often associated with asthma, a common pulmonary allergy. This narrowing is caused by inflammation and constriction of the airways in response to allergens. Shortness of breath (dyspnea) can accompany wheezing, making it difficult to get enough air. Severe wheezing and shortness of breath can be a medical emergency.
- Whistling sound during breathing (wheezing)
- Difficulty catching your breath (dyspnea)
- Tightness in the chest
3. Chest Tightness and Discomfort
A feeling of tightness or pressure in the chest is another common symptom, often accompanying wheezing and shortness of breath. This sensation results from the inflammation and constriction of the airways, making it difficult to fully expand the lungs. The discomfort can range from mild to severe, making breathing uncomfortable or painful. Chest tightness can be a warning sign of a worsening allergic reaction.
- Sensation of pressure or tightness in the chest
- Discomfort during breathing
- Pain in the chest (in some cases)
4. Increased Mucus Production
Allergic reactions in the lungs can lead to increased production of mucus. This mucus is often thicker and more difficult to clear than normal, leading to congestion and further airway obstruction. The color of the mucus may vary, sometimes appearing clear, white, or even yellow or green, depending on the severity and duration of the allergic response. Excessive mucus production can further impair breathing.
- Increased production of thick mucus (phlegm)
- Difficulty clearing mucus from the airways
- Changes in mucus color (clear, white, yellow, or green)
5. Repeated Respiratory Infections
Individuals with pulmonary allergies may experience more frequent respiratory infections, such as colds, bronchitis, or pneumonia. This is because the underlying inflammation and irritation in the airways make them more susceptible to infections. The weakened immune response in the respiratory tract, due to chronic inflammation, increases the risk of developing these infections more often and with potentially greater severity. Recurring respiratory infections may indicate an underlying pulmonary allergy.
- Frequent colds or upper respiratory infections
- Recurrent bronchitis or pneumonia
- Slower recovery from respiratory infections
Can allergies cause permanent lung damage?
While allergies themselves don't directly cause permanent lung damage in most cases, severe and long-term allergic reactions can contribute to conditions that do. Asthma, often triggered by allergies, is a prime example. Untreated or poorly managed asthma can lead to chronic inflammation and airway remodeling, resulting in irreversible lung damage over time. This damage can manifest as reduced lung function, increased susceptibility to infections, and difficulty breathing. Similarly, allergic reactions can exacerbate existing lung conditions like chronic obstructive pulmonary disease (COPD), accelerating their progression and increasing the severity of symptoms. Another key factor is the development of allergic bronchopulmonary aspergillosis (ABPA), a fungal infection often seen in individuals with asthma and allergies. ABPA can lead to significant lung damage, including bronchiectasis (widening of the airways) and the formation of lung lesions. Therefore, while allergies aren't a direct cause of permanent lung damage for most people, the associated respiratory problems and complications can significantly increase the risk if not properly managed.
Can seasonal allergies damage my lungs?
Seasonal allergies, while often inconvenient, typically don't directly cause permanent lung damage. The inflammation and irritation experienced during allergy season primarily affect the upper airways, such as the nose and throat. However, the inflammation can trigger an asthma exacerbation in individuals with pre-existing asthma. This can lead to temporary airway constriction, wheezing, and shortness of breath. While these episodes are uncomfortable and can impact lung function temporarily, they usually resolve once the allergen exposure decreases and treatment is administered. However, repeatedly experiencing severe allergic reactions or poorly managing asthma triggered by seasonal allergies could contribute to long-term lung damage over many years. It's crucial to manage seasonal allergies effectively through medication, allergen avoidance, and by following a physician's advice to mitigate potential risks. Ignoring symptoms or inadequate treatment can increase the risk of complications and potential longer-term consequences.
What types of allergies are most likely to cause lung problems?
Allergies to airborne substances are most likely to cause lung problems. Dust mites, pet dander, mold spores, and pollen are common culprits that can directly trigger respiratory symptoms. These allergens can trigger inflammation in the airways, leading to symptoms like coughing, wheezing, and shortness of breath. Individuals with allergies to these substances are at higher risk of developing or exacerbating conditions like asthma and other respiratory illnesses. In addition, food allergies, while not directly affecting the lungs in the same way, can cause anaphylaxis, a severe allergic reaction that can lead to airway constriction and difficulty breathing, potentially causing significant short-term, and in rare cases, long-term lung issues if severe enough. Therefore, while any allergy can potentially trigger respiratory issues in sensitive individuals, those involving airborne allergens tend to pose the greatest risk to lung health.
How can I protect my lungs from allergy-related damage?
Protecting your lungs from allergy-related damage involves a multi-pronged approach focused on preventing and managing allergic reactions. Firstly, identifying and avoiding known allergens is crucial. This involves regular allergy testing to pinpoint specific triggers and making lifestyle adjustments to minimize exposure. Secondly, effective allergy management is paramount. This includes using prescribed medications such as antihistamines, nasal corticosteroids, and inhalers as directed by a physician. For severe allergies, immunotherapy (allergy shots) can be considered to desensitize the immune system over time. Maintaining good overall health is equally important, as a strong immune system is better equipped to handle allergic reactions. This includes a balanced diet, regular exercise, and adequate sleep. Regular check-ups with your doctor and a specialist, if necessary, are essential for monitoring lung health and ensuring timely intervention should any problems arise. Early diagnosis and prompt treatment of any respiratory symptoms associated with allergies are crucial to preventing long-term complications and potential lung damage.
Deja una respuesta