What is the bird handler's disease

As exotic winged creatures grace our homes and hearts, a name that often takes flight in hushed tones within the veterinary world is "Bird Handler's Disease." This enigmatic affliction, a dance between human and avian health, demands attention. Let us unveil its enigmatic nature, explore the risks it poses, and illuminate the path towards prevention and containment.
What is Bird Handler's Disease (Psittacosis)?
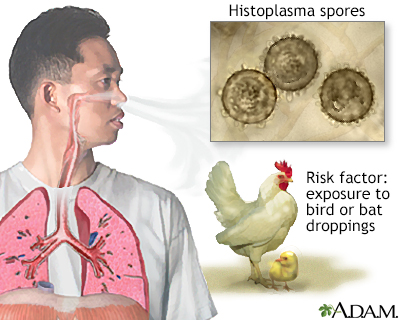
Bird handler's disease, also known as psittacosis or ornithosis, is a zoonotic disease caused by the bacterium Chlamydia psittaci. This means it can be transmitted from birds to humans. The bacteria are shed in the droppings, respiratory secretions, and feathers of infected birds, particularly parrots, parakeets, cockatoos, and other psittacine birds. Infection occurs primarily through inhalation of aerosolized bacteria, although direct contact with infected birds or their contaminated materials can also lead to transmission. Symptoms can range from mild to severe, and if left untreated, psittacosis can be life-threatening.
Symptoms of Bird Handler's Disease
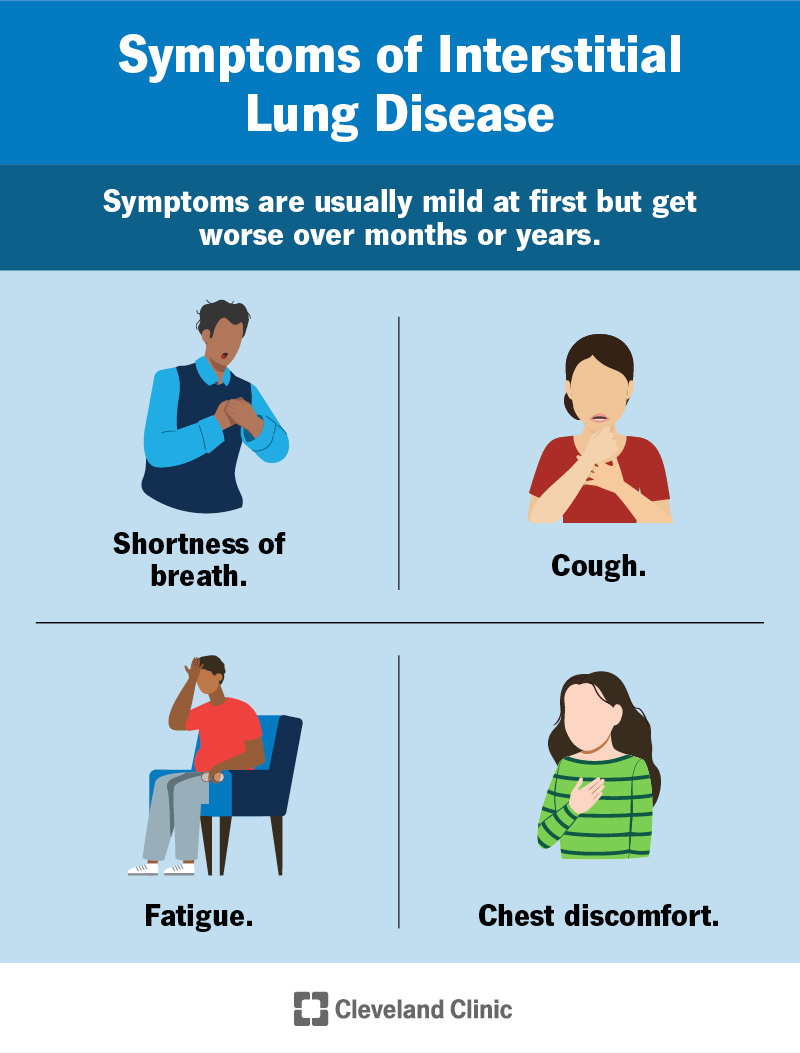
Symptoms of psittacosis can vary widely in severity and presentation. Some individuals may experience only mild flu-like symptoms, while others can develop a more serious pneumonia. Common symptoms include: fever, chills, headache, muscle aches, cough, shortness of breath, and fatigue. In more severe cases, pneumonia can develop, leading to difficulty breathing, chest pain, and potentially respiratory failure. It's crucial to note that the symptoms can mimic other respiratory illnesses, making diagnosis challenging.
Transmission of Bird Handler's Disease
The primary mode of transmission is through the inhalation of aerosolized bacteria shed from infected birds. This can occur when cleaning cages, handling birds, or even being in close proximity to infected birds. Direct contact with infected bird droppings, feathers, or respiratory secretions can also transmit the bacteria. The bacteria can remain viable in the environment for extended periods, increasing the risk of transmission. Human-to-human transmission is rare but possible, primarily through close contact with respiratory secretions.
Diagnosis of Bird Handler's Disease
Diagnosing psittacosis involves a combination of clinical evaluation and laboratory testing. Doctors will consider the patient's symptoms, exposure history (contact with birds), and travel history. Laboratory tests, such as serological tests (detecting antibodies against C. psittaci) and PCR testing (detecting the bacterial DNA), are crucial for confirming the diagnosis. Early diagnosis is essential for effective treatment and to prevent severe complications.
Treatment of Bird Handler's Disease
Antibiotics, such as tetracycline or doxycycline, are the mainstay of treatment for psittacosis. Early initiation of antibiotic therapy is crucial to prevent severe complications and improve the outcome. The duration of treatment depends on the severity of the illness and the patient's response to therapy. Supportive care, including rest, fluids, and management of symptoms, is also important. Proper treatment significantly reduces the risk of serious complications.
Prevention of Bird Handler's Disease
Prevention strategies focus on minimizing exposure to infected birds and their contaminated environments. These include: good hygiene practices (handwashing), proper ventilation when handling birds, avoiding close contact with birds showing signs of illness, and regular cleaning and disinfection of bird cages and environments. If you work with birds, consider using personal protective equipment (PPE), such as masks and gloves. Early detection and treatment of infected birds are also critical to preventing the spread of the disease.
| Risk Factor | Description |
|---|---|
| Close contact with birds | Working with birds, especially psittacine birds, increases the risk of infection. |
| Poor hygiene | Insufficient handwashing and cleaning practices can facilitate transmission. |
| Exposure to aerosolized bacteria | Inhaling bacteria from bird droppings or respiratory secretions is a primary route of infection. |
| Immunocompromised individuals | People with weakened immune systems are more susceptible to severe illness. |
| Lack of ventilation | Poor ventilation can increase the concentration of airborne bacteria. |
What is Bird Handler's Disease (Psittacosis)?
Bird handler's disease, also known as psittacosis or ornithosis, is a zoonotic disease caused by the bacterium Chlamydia psittaci. This means it can be transmitted from birds to humans. The bacteria are shed in the droppings, respiratory secretions, and feathers of infected birds, particularly parrots, parakeets, cockatoos, and other psittacine birds. Infection occurs primarily through inhalation of aerosolized bacteria, although direct contact with infected birds or their contaminated materials can also lead to transmission. Symptoms can range from mild to severe, and if left untreated, psittacosis can be life-threatening.
Symptoms of Bird Handler's Disease
Symptoms of psittacosis can vary widely in severity and presentation. Some individuals may experience only mild flu-like symptoms, while others can develop a more serious pneumonia. Common symptoms include: fever, chills, headache, muscle aches, cough, shortness of breath, and fatigue. In more severe cases, pneumonia can develop, leading to difficulty breathing, chest pain, and potentially respiratory failure. It's crucial to note that the symptoms can mimic other respiratory illnesses, making diagnosis challenging.
Transmission of Bird Handler's Disease
The primary mode of transmission is through the inhalation of aerosolized bacteria shed from infected birds. This can occur when cleaning cages, handling birds, or even being in close proximity to infected birds. Direct contact with infected bird droppings, feathers, or respiratory secretions can also transmit the bacteria. The bacteria can remain viable in the environment for extended periods, increasing the risk of transmission. Human-to-human transmission is rare but possible, primarily through close contact with respiratory secretions.
Diagnosis of Bird Handler's Disease
Diagnosing psittacosis involves a combination of clinical evaluation and laboratory testing. Doctors will consider the patient's symptoms, exposure history (contact with birds), and travel history. Laboratory tests, such as serological tests (detecting antibodies against C. psittaci) and PCR testing (detecting the bacterial DNA), are crucial for confirming the diagnosis. Early diagnosis is essential for effective treatment and to prevent severe complications.
Treatment of Bird Handler's Disease
Antibiotics, such as tetracycline or doxycycline, are the mainstay of treatment for psittacosis. Early initiation of antibiotic therapy is crucial to prevent severe complications and improve the outcome. The duration of treatment depends on the severity of the illness and the patient's response to therapy. Supportive care, including rest, fluids, and management of symptoms, is also important. Proper treatment significantly reduces the risk of serious complications.
Prevention of Bird Handler's Disease
Prevention strategies focus on minimizing exposure to infected birds and their contaminated environments. These include: good hygiene practices (handwashing), proper ventilation when handling birds, avoiding close contact with birds showing signs of illness, and regular cleaning and disinfection of bird cages and environments. If you work with birds, consider using personal protective equipment (PPE), such as masks and gloves. Early detection and treatment of infected birds are also critical to preventing the spread of the disease.
| Risk Factor | Description |
|---|---|
| Close contact with birds | Working with birds, especially psittacine birds, increases the risk of infection. |
| Poor hygiene | Insufficient handwashing and cleaning practices can facilitate transmission. |
| Exposure to aerosolized bacteria | Inhaling bacteria from bird droppings or respiratory secretions is a primary route of infection. |
| Immunocompromised individuals | People with weakened immune systems are more susceptible to severe illness. |
| Lack of ventilation | Poor ventilation can increase the concentration of airborne bacteria. |
What is the life expectancy of someone with interstitial lung disease?
What is the life expectancy of someone with Interstitial Lung Disease?
The life expectancy of someone with interstitial lung disease (ILD) is highly variable and depends on several factors. There's no single answer, as the disease encompasses a wide range of conditions with different prognoses. The specific type of ILD, the stage of the disease at diagnosis, the patient's overall health, and their response to treatment all significantly impact survival rates. Some ILDs progress slowly, allowing individuals to live for many years with the condition, while others progress rapidly, leading to a shorter life expectancy. While some individuals may live for 10 years or more after diagnosis, others may have a much shorter life expectancy, even within a few years. It's crucial to consult with a pulmonologist for an accurate prognosis based on individual circumstances.
Factors Influencing Life Expectancy in ILD
Several key factors contribute to the variability in life expectancy for individuals with ILD. These factors often interact, making accurate prediction challenging. Early diagnosis and prompt treatment are crucial for improving outcomes. However, the nature of the disease itself plays a significant role. The rate of lung function decline varies greatly among different ILDs. Furthermore, the presence of comorbidities (other health conditions) can significantly impact life expectancy. Finally, the patient's overall health, including their response to treatment and ability to manage their symptoms, also plays a role.
- Type of ILD: Different ILDs have vastly different prognoses. Some, like idiopathic pulmonary fibrosis (IPF), are associated with a poorer prognosis compared to others.
- Disease Stage at Diagnosis: Earlier diagnosis typically leads to better management and improved outcomes. Advanced stages are often associated with shorter lifespans.
- Response to Treatment: Some individuals respond well to treatment, experiencing slowed disease progression and improved quality of life, while others may not respond as effectively.
Idiopathic Pulmonary Fibrosis (IPF) and Life Expectancy
Idiopathic pulmonary fibrosis (IPF) is one of the most common and severe forms of ILD. It's characterized by progressive scarring of the lungs. The median survival time for IPF patients is typically 2 to 5 years after diagnosis, although some individuals may live longer or shorter. The prognosis is influenced by factors such as age, severity of symptoms, and the presence of other health issues. New treatments have extended survival time, but IPF remains a life-limiting condition.
- Advanced Age: Older individuals may experience faster disease progression and poorer outcomes.
- Severity of Symptoms: The intensity of symptoms at diagnosis impacts survival rate.
- Comorbidities: The presence of other diseases, such as heart disease or diabetes, can negatively affect life expectancy.
Impact of Treatment on Life Expectancy
While ILD is currently incurable, various treatment options can significantly impact the disease's progression and improve quality of life. These treatments may slow disease progression, reduce symptoms, and extend survival. However, the effectiveness of treatments varies among individuals, and some patients may not respond well. Treatment plans are often individualized to account for the specific type of ILD, disease severity, and the patient's overall health.
- Medication: Anti-fibrotic drugs have shown some success in slowing disease progression for certain types of ILD.
- Oxygen Therapy: Supplemental oxygen can help improve breathing and reduce shortness of breath.
- Pulmonary Rehabilitation: This program helps improve lung function and overall fitness.
Other Factors Affecting Prognosis
Beyond the specific ILD type and treatment, several additional factors can influence a patient's prognosis. Lifestyle choices, such as smoking cessation and maintaining a healthy weight, can be beneficial. Furthermore, access to quality healthcare and supportive care services plays a vital role in improving outcomes. Psychological support and regular monitoring by healthcare professionals are essential aspects of managing ILD.
- Smoking: Smoking significantly worsens ILD progression and should be avoided.
- Nutritional Status: Maintaining good nutrition is important for overall health and managing the disease.
- Social Support: Strong social support networks can improve coping mechanisms and quality of life.
Importance of Early Diagnosis and Management
Early diagnosis is crucial for effective management of ILD and improving prognosis. Early intervention allows for prompt implementation of treatment strategies that can help slow disease progression. Regular monitoring of lung function and symptom management are essential for those with ILD. The involvement of a multidisciplinary team, including pulmonologists, respiratory therapists, and other healthcare professionals, is highly beneficial for comprehensive care. This team approach ensures that all aspects of the patient's health are addressed, promoting improved quality of life and extended survival.
- Regular Checkups: Routine monitoring allows for early detection of changes in lung function.
- Prompt Treatment: Immediate treatment initiation can slow the disease progression.
- Multidisciplinary Care: A coordinated care team provides comprehensive management.
Is bird fancier's lung curable?

Bird fancier's lung, also known as avian-protein induced hypersensitivity pneumonitis, is not curable in the sense that the underlying lung damage cannot be completely reversed. However, it is a manageable condition. The key to successful management is avoiding exposure to the causative avian antigens, which are typically found in bird droppings, feathers, and dander. With prompt diagnosis and avoidance of exposure, the progression of the disease can be halted, and symptoms can significantly improve. If the disease is caught early and exposure is eliminated, complete recovery is possible, although some scarring may remain.
What are the treatment options for Bird Fancier's Lung?
Treatment for bird fancier's lung focuses primarily on managing symptoms and preventing further lung damage. This involves:
- Avoiding exposure to birds and their droppings: This is the most crucial step in managing the condition. It often necessitates giving up bird keeping or significantly altering how birds are handled and their environment is managed.
- Medication: Corticosteroids are often prescribed to reduce inflammation in the lungs and alleviate symptoms. Bronchodilators can help to open up the airways and improve breathing. In severe cases, immunosuppressants may be used.
- Supportive care: This may include oxygen therapy if breathing difficulties are severe, pulmonary rehabilitation to improve lung function, and monitoring for potential complications.
How is Bird Fancier's Lung Diagnosed?
Diagnosing bird fancier's lung involves a combination of:
- Detailed medical history: This includes information about your exposure to birds and your symptoms.
- Physical examination: The doctor will listen to your lungs and check your breathing.
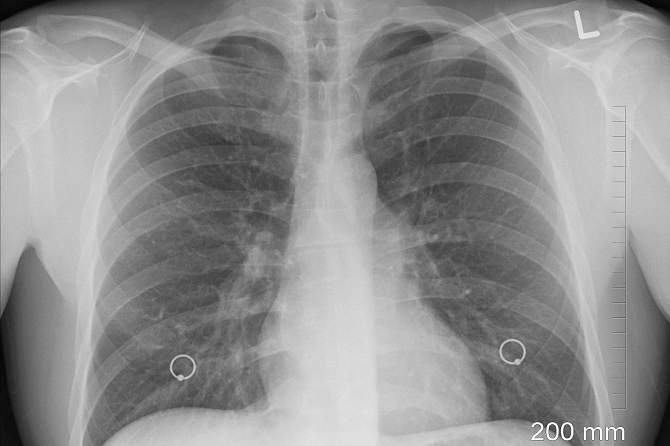
- Chest X-ray or CT scan: These imaging tests can reveal characteristic lung abnormalities associated with bird fancier's lung.
- Blood tests: These may show elevated inflammatory markers. Specific antibody tests to detect sensitization to bird proteins are helpful.
- Pulmonary function tests: These tests assess your lung capacity and airflow.
What are the long-term effects of Bird Fancier's Lung?
The long-term effects of bird fancier's lung depend on several factors including:
- Severity of the initial disease: Individuals with severe disease at diagnosis are at higher risk of long-term complications.
- Duration of exposure: Prolonged exposure to birds increases the risk of permanent lung damage.
- Adherence to treatment and avoidance of exposure: Individuals who effectively avoid exposure and follow their prescribed treatment plans tend to have better outcomes.
- Potential for other complications: There is a possibility of developing other respiratory illnesses or complications, such as chronic obstructive pulmonary disease (COPD) or pulmonary fibrosis.
What is the prognosis for Bird Fancier's Lung?
The prognosis for bird fancier's lung is generally good if the condition is diagnosed early and exposure to birds is avoided. With appropriate treatment and avoidance of exposure, many individuals experience a significant improvement in their symptoms and lung function. However, some individuals may experience persistent symptoms or develop long-term lung damage, especially if the disease is severe or exposure continues.
- Early diagnosis and treatment are crucial: This helps prevent progression to more serious stages and long-term lung damage.
- Complete avoidance of exposure is vital: Continued exposure can lead to recurrence and worsening of the disease.
- Regular monitoring is recommended: This allows for early detection of any recurrence or complications.
Can Bird Fancier's Lung be prevented?
Preventing bird fancier's lung involves reducing exposure to avian proteins. This can be achieved through:
- Good ventilation in bird-keeping environments: This helps to dilute the concentration of avian proteins in the air.
- Regular cleaning of bird cages and surrounding areas: This removes droppings and other sources of avian antigens.
- Use of personal protective equipment (PPE): Wearing masks and gloves when cleaning cages or handling birds can reduce exposure.
- Limiting exposure to birds: Reducing the number of birds kept and minimizing close contact can lower the risk.
- Regular health check-ups if you handle birds: Early detection is key to improved management of the condition.
What is the life expectancy of hypersensitivity pneumonitis?
There isn't a single definitive answer to the question of life expectancy for hypersensitivity pneumonitis (HP). The prognosis for HP is highly variable and depends on several crucial factors. Early diagnosis and avoidance of the offending antigen are critical for a favorable outcome. If the disease is detected early and the causative agent is identified and eliminated, many individuals can achieve complete resolution of symptoms and experience a normal lifespan. However, if the condition progresses to a more severe, chronic form, the outlook can be significantly impacted. The severity of lung damage, the presence of complications like pulmonary fibrosis, and the individual's overall health all influence their long-term prognosis. In advanced cases, HP can lead to significant respiratory impairment, reducing life expectancy. Therefore, predicting life expectancy for an individual with HP is complex and necessitates considering the specific clinical presentation and response to treatment.
Factors Affecting Life Expectancy in Hypersensitivity Pneumonitis
Several factors contribute to the variability in life expectancy among individuals with hypersensitivity pneumonitis. The key factors include the severity of lung involvement at the time of diagnosis, the success of allergen avoidance, and the development of complications. The earlier the diagnosis and the more effectively the allergen is removed from the individual's environment, the better the chance for a positive outcome. Conversely, the development of complications such as pulmonary fibrosis can significantly worsen the prognosis. Effective management of these factors can play a pivotal role in improving the life expectancy for individuals with HP.
- Severity of Lung Damage: The extent of inflammation and fibrosis in the lungs at diagnosis directly correlates with prognosis. Mild cases may resolve completely, while severe cases may lead to irreversible lung damage.
- Effectiveness of Allergen Avoidance: Consistent avoidance of the offending antigen is crucial. Continued exposure can lead to disease progression and worsening of symptoms.
- Presence of Complications: Pulmonary fibrosis is a major concern. Its development significantly reduces lung function and can lead to respiratory failure.
Impact of Chronic Hypersensitivity Pneumonitis on Life Expectancy
Chronic hypersensitivity pneumonitis represents a more severe form of the disease, characterized by persistent inflammation and progressive fibrosis. Chronic HP significantly impacts life expectancy. Individuals with this form may experience a progressive decline in lung function, leading to shortness of breath, reduced exercise capacity, and eventually respiratory failure. The severity of the lung damage, often irreversible, determines the extent of the impact on survival. Supportive care becomes crucial in managing symptoms and improving quality of life.
- Progressive Lung Fibrosis: The hallmark of chronic HP is the development of extensive pulmonary fibrosis, leading to irreversible lung scarring and reduced lung capacity.
- Respiratory Failure: Advanced cases can lead to respiratory failure, requiring supplemental oxygen or mechanical ventilation.
- Reduced Quality of Life: The progressive nature of chronic HP significantly impacts an individual's quality of life, limiting physical activity and overall well-being.
Treatment and its Influence on Prognosis
Early and appropriate treatment significantly influences the prognosis of hypersensitivity pneumonitis. Avoiding exposure to the causative antigen is paramount. Treatment strategies may include corticosteroids to reduce inflammation, immunosuppressants in severe cases, and supportive measures such as oxygen therapy. While treatment cannot reverse existing lung damage, it can help manage symptoms, slow disease progression, and potentially improve life expectancy. Regular monitoring of lung function is essential for early detection of disease progression.
- Corticosteroids: Used to reduce inflammation and improve lung function.
- Immunosuppressants: Employed in severe cases to suppress the immune response driving the disease.
- Supportive Care: Includes oxygen therapy, pulmonary rehabilitation, and management of respiratory infections.
Role of Early Diagnosis in Improving Outcomes
Early diagnosis is crucial for a favorable outcome in hypersensitivity pneumonitis. Early intervention allows for prompt removal of the causative antigen, reducing further lung damage and preventing the development of chronic disease. Early diagnosis significantly increases the likelihood of a complete resolution or at least slowing the progression of the disease. A delay in diagnosis can lead to irreversible lung damage and a poorer prognosis.
- Prompt Allergen Avoidance: Immediate removal of the offending agent minimizes further lung damage.
- Effective Treatment Initiation: Early treatment can help prevent disease progression and manage symptoms more effectively.
- Improved Quality of Life: Early intervention contributes to maintaining a better quality of life by slowing the progression of the disease.
Individual Variation and Prognostic Uncertainty
It is important to understand that the prognosis of hypersensitivity pneumonitis is not uniform across all individuals. Individual responses to treatment and the severity of underlying conditions contribute to the variability in outcomes. Genetic predisposition, co-morbidities, and patient compliance with treatment all influence the course of the disease. Therefore, precise prediction of life expectancy for a specific individual remains challenging and requires a careful evaluation of their particular circumstances.
- Genetic Factors: Genetic variations may influence individual susceptibility and response to treatment.
- Co-morbidities: The presence of other health conditions can affect the overall prognosis.
- Patient Compliance: Adherence to treatment recommendations is crucial for positive outcomes.
What is the bird disease in the human lungs?
There is no single "bird disease" that directly infects human lungs. However, several diseases carried by birds can affect humans, primarily through respiratory transmission. The most significant of these is avian influenza (bird flu). While many avian influenza viruses don't infect humans, some subtypes, like H5N1 and H7N9, can cause severe respiratory illness, including pneumonia. The virus infects the respiratory tract, causing inflammation and fluid buildup in the lungs, leading to difficulty breathing and potentially death. Transmission usually occurs through direct contact with infected birds or contaminated surfaces. Other avian-borne pathogens can also affect the lungs, though less commonly and usually with less severe respiratory symptoms.
What are the Avian Influenza Viruses that can infect humans?
Several subtypes of avian influenza viruses are zoonotic, meaning they can spread from animals to humans. H5N1 and H7N9 are two of the most concerning subtypes known for causing severe human illness. While outbreaks can occur sporadically, the risk to human populations is relatively low compared to other respiratory infections. However, the potential for these viruses to mutate and become more easily transmissible between humans is a significant concern for public health officials. Understanding the viral characteristics and potential for pandemic spread is an ongoing area of research.
- H5N1 (Highly Pathogenic Avian Influenza): Often associated with severe illness and high mortality rates in humans.
- H7N9 (Low Pathogenic Avian Influenza): Can cause milder illness, but still poses a risk, especially to vulnerable populations.
- Other subtypes exist, but their zoonotic potential and transmissibility to humans are generally lower.
How is Avian Influenza Transmitted to Humans?
Transmission of avian influenza to humans typically happens through direct contact with infected birds or their droppings. This includes handling infected poultry, cleaning their cages, or coming into contact with contaminated surfaces. Indirect transmission is also possible, but less common. For example, it might occur if a person inhales airborne virus particles from a highly contaminated environment, though usually, this requires close proximity to infected birds. Human-to-human transmission is rare with most avian influenza subtypes, but it can occur, particularly with more easily transmitted strains.
- Direct contact with infected birds (live or dead).
- Contact with bird droppings or contaminated surfaces.
- Inhaling virus particles in a highly contaminated environment (rare).
What are the Symptoms of Avian Influenza in Humans?
Symptoms of avian influenza in humans can vary widely, from mild to severe. Many cases initially present with flu-like symptoms such as fever, cough, sore throat, muscle aches, and fatigue. However, severe cases can quickly develop into pneumonia, leading to respiratory distress, shortness of breath, and potentially organ failure. Prompt medical attention is crucial for those experiencing severe symptoms, as the disease can be fatal. Early diagnosis and antiviral treatment are essential for improving outcomes.
- Fever and chills.
- Cough (often severe).
- Shortness of breath or difficulty breathing (severe cases).
- Muscle aches.
- Fatigue.
- Pneumonia.
How is Avian Influenza Diagnosed and Treated?
Diagnosis of avian influenza often involves a combination of clinical assessment, laboratory testing of respiratory samples (like nasal swabs), and epidemiological investigation. Rapid diagnostic tests can provide preliminary results, while more definitive testing using PCR (polymerase chain reaction) is used to confirm the presence of the virus and identify the specific subtype. Treatment typically involves supportive care to manage symptoms, such as oxygen therapy for respiratory distress. Antiviral medications, such as oseltamivir (Tamiflu), may be used to reduce the severity and duration of illness, but their effectiveness is influenced by factors such as early administration and the specific virus strain.
- Clinical examination of symptoms.
- Laboratory testing (PCR, rapid tests).
- Epidemiological investigation (tracing contacts, identifying potential sources).
- Supportive care (oxygen therapy, fluids).
- Antiviral medications (oseltamivir).
What are the Prevention Measures for Avian Influenza?
Preventing the spread of avian influenza requires a multi-pronged approach. Strict hygiene practices are crucial, including frequent handwashing, avoiding contact with potentially infected birds, and practicing respiratory etiquette (covering coughs and sneezes). Proper handling and cooking of poultry are also important. For those working with poultry or in areas with known outbreaks, personal protective equipment (PPE) may be necessary. Surveillance and rapid response systems are vital for monitoring outbreaks and containing the spread of the virus.
- Frequent handwashing.
- Avoiding contact with birds (especially sick or dead birds).
- Proper cooking of poultry.
- Use of personal protective equipment (PPE) in high-risk settings.
- Surveillance and rapid response systems.
What is bird handler's disease?
Bird handler's disease, also known as psittacosis or ornithosis, is a zoonotic disease caused by infection with the bacterium Chlamydophila psittaci. This bacterium is found in a variety of birds, including parrots, pigeons, ducks, chickens, and turkeys, but it can also infect other animals and, importantly, humans. The disease is transmitted through contact with infected birds, their droppings, or contaminated environments. Infection typically occurs through inhalation of airborne particles containing the bacteria, but it can also occur through direct contact with infected tissues or fluids. Symptoms can vary widely, ranging from mild flu-like illness to severe pneumonia. The severity of the illness depends on a number of factors, including the individual's immune system, the dose of bacteria inhaled, and the specific strain of Chlamydophila psittaci involved. Early diagnosis and treatment with antibiotics are crucial to preventing severe complications and ensuring a full recovery. Without treatment, psittacosis can lead to serious and potentially life-threatening conditions, including respiratory failure, liver damage, and even death.
What are the symptoms of bird handler's disease?
The symptoms of bird handler's disease are quite variable and can range from mild to severe. In many cases, the illness begins with flu-like symptoms, such as fever, headache, muscle aches, and fatigue. These symptoms can be accompanied by a dry cough that may eventually produce phlegm. Some individuals may also experience chills, sweating, and loss of appetite. More serious cases can develop pneumonia, which presents with chest pain, shortness of breath, and difficulty breathing. In severe cases, liver and spleen enlargement, jaundice, and neurological complications, such as confusion and delirium, can occur. The incubation period, the time between exposure and the onset of symptoms, can range from a few days to several weeks, with an average of about one to two weeks. It’s important to note that many individuals infected with Chlamydophila psittaci are asymptomatic or experience only mild symptoms, making diagnosis challenging. If you suspect you may have been exposed to Chlamydophila psittaci and experience any of these symptoms, it's crucial to seek medical attention immediately.
How is bird handler's disease diagnosed?
Diagnosing bird handler's disease requires a combination of clinical evaluation, patient history, and laboratory testing. A thorough medical history, including recent contact with birds or bird droppings, is essential for the physician to suspect the disease. The physical examination may reveal findings consistent with pneumonia or other respiratory infections. However, these findings are not specific to psittacosis, making laboratory testing crucial for confirmation. Laboratory testing typically involves serological tests, such as complement fixation tests and enzyme-linked immunosorbent assays (ELISAs), which detect antibodies to Chlamydophila psittaci in the blood. These tests can help determine if a person has been infected, but they may not be positive in the early stages of the illness. PCR (polymerase chain reaction) tests can detect the bacterial DNA directly in respiratory samples, providing a more rapid diagnosis. Chest X-rays may also be performed to assess the lungs for signs of pneumonia. The combination of clinical presentation, epidemiological history, and laboratory testing results provides the most reliable means of diagnosing bird handler's disease. The exact methodology and tests used can vary depending on the availability and resources of the healthcare facility.
How is bird handler's disease treated?
The treatment for bird handler's disease involves antibiotics, specifically those effective against Chlamydophila psittaci. Tetracyclines, such as doxycycline, are typically the drugs of choice. Other antibiotics, such as erythromycin and azithromycin, can also be used, particularly if the patient is allergic to tetracyclines. The duration of antibiotic treatment usually ranges from several weeks, depending on the severity of the infection and the patient's response to therapy. Treatment should be started as early as possible to prevent severe complications. Supportive care, including rest, fluids, and symptomatic treatment for fever and cough, is also an important part of managing the illness. Hospitalization may be necessary for severe cases, especially those with pneumonia requiring oxygen therapy or other intensive respiratory support. Monitoring the patient's response to treatment is crucial to ensure the effectiveness of the therapy. Regular follow-up visits with the physician are essential to evaluate the progress and to address any potential complications. In many cases, a complete recovery can be expected with prompt diagnosis and appropriate treatment.
Deja una respuesta