Do allergies mean a weak immune system

Do allergies mean a weak immune system? It's a common misconception that people with allergies have a compromised immune system. In fact, allergies are a sign that your immune system is working too well. When you come into contact with an allergen, your body produces antibodies to fight it off. This reaction can cause symptoms such as sneezing, runny nose, and watery eyes. While allergies can be annoying and uncomfortable, they're not a sign that your immune system is weak. In fact, people with allergies may be more likely to fight off infections and other diseases.
Do Allergies Mean a Weak Immune System?
The simple answer is no, allergies do not necessarily indicate a weak immune system. In fact, it's quite the opposite. Allergies are a result of an overactive, not a weak, immune system. A healthy immune system protects the body from harmful invaders like bacteria and viruses. However, in individuals with allergies, the immune system mistakenly identifies harmless substances, called allergens (like pollen, pet dander, or peanuts), as threats. This triggers an exaggerated immune response, leading to allergic symptoms.
What is an Allergic Reaction?
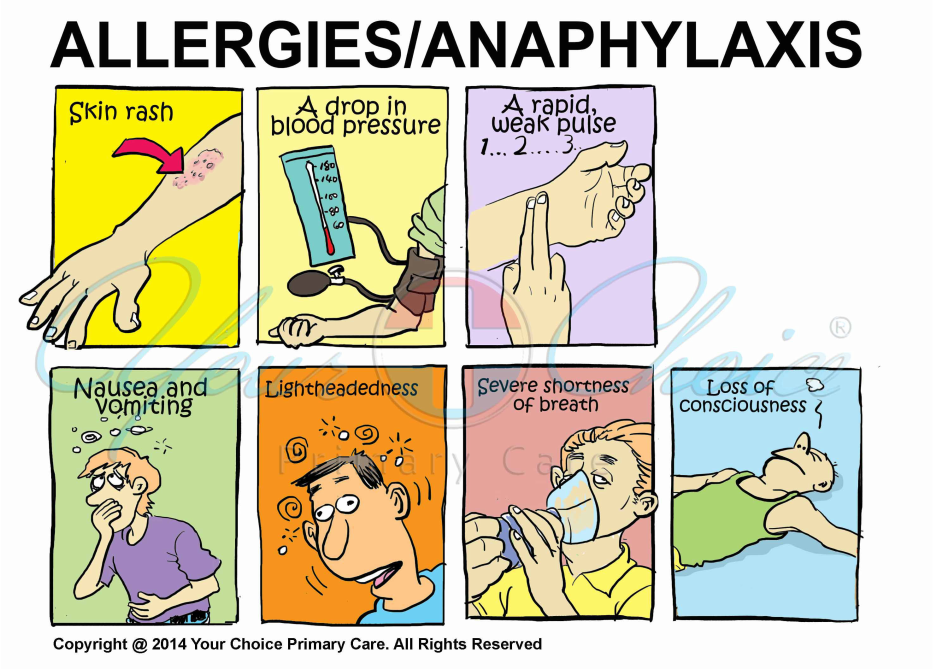
An allergic reaction occurs when the body's immune system releases histamine and other chemicals in response to an allergen. These chemicals cause the characteristic symptoms of allergies, such as sneezing, itching, runny nose, rash, and in severe cases, anaphylaxis. The intensity of the reaction varies depending on the individual, the allergen, and the amount of exposure. The immune system's response is targeted at eliminating the perceived threat, even though the allergen poses no real danger.
The Role of IgE Antibodies
Immunoglobulin E (IgE) antibodies play a central role in allergic reactions. When the body encounters an allergen for the first time, it produces IgE antibodies specific to that allergen. These antibodies bind to mast cells and basophils, which are types of white blood cells. Upon subsequent exposure to the same allergen, the IgE antibodies trigger the release of histamine and other inflammatory mediators from these cells, leading to the allergic symptoms.
The Difference Between Allergies and Immunodeficiency
It's crucial to distinguish between allergies and immunodeficiency. Immunodeficiency refers to a weakened immune system that is unable to fight off infections effectively. Individuals with immunodeficiency are more susceptible to various infections and illnesses. Allergies, on the other hand, involve an overactive immune response to harmless substances, not a deficient one. They are distinct conditions with different underlying mechanisms.
Genetics and Environmental Factors in Allergies
The development of allergies is influenced by a complex interplay of genetic and environmental factors. A family history of allergies increases the risk of developing allergies. Environmental exposures, such as pollution, early exposure to certain allergens, and hygiene hypothesis (reduced exposure to microbes in early childhood) also contribute to the development of allergies.
Can Allergies Coexist with Other Immune Conditions?
Yes, it is possible to have allergies and other immune conditions simultaneously. For example, some individuals with allergies may also have autoimmune diseases, where the immune system attacks the body's own tissues. While allergies represent an overactive immune response, autoimmune diseases represent a misdirected immune response. The presence of one condition doesn't preclude the other.
| Condition | Immune System State | Characteristics |
|---|---|---|
| Allergies | Overactive | Exaggerated response to harmless substances; release of histamine; IgE antibodies involved. |
| Immunodeficiency | Weakened | Increased susceptibility to infections; impaired ability to fight off pathogens. |
| Autoimmune Disease | Misdirected | Immune system attacks the body's own tissues; chronic inflammation. |
Do Allergies Mean a Weak Immune System?
The simple answer is no, allergies do not necessarily indicate a weak immune system. In fact, it's quite the opposite. Allergies are a result of an overactive, not a weak, immune system. A healthy immune system protects the body from harmful invaders like bacteria and viruses. However, in individuals with allergies, the immune system mistakenly identifies harmless substances, called allergens (like pollen, pet dander, or peanuts), as threats. This triggers an exaggerated immune response, leading to allergic symptoms.
What is an Allergic Reaction?
An allergic reaction occurs when the body's immune system releases histamine and other chemicals in response to an allergen. These chemicals cause the characteristic symptoms of allergies, such as sneezing, itching, runny nose, rash, and in severe cases, anaphylaxis. The intensity of the reaction varies depending on the individual, the allergen, and the amount of exposure. The immune system's response is targeted at eliminating the perceived threat, even though the allergen poses no real danger.
The Role of IgE Antibodies
Immunoglobulin E (IgE) antibodies play a central role in allergic reactions. When the body encounters an allergen for the first time, it produces IgE antibodies specific to that allergen. These antibodies bind to mast cells and basophils, which are types of white blood cells. Upon subsequent exposure to the same allergen, the IgE antibodies trigger the release of histamine and other inflammatory mediators from these cells, leading to the allergic symptoms.
The Difference Between Allergies and Immunodeficiency
It's crucial to distinguish between allergies and immunodeficiency. Immunodeficiency refers to a weakened immune system that is unable to fight off infections effectively. Individuals with immunodeficiency are more susceptible to various infections and illnesses. Allergies, on the other hand, involve an overactive immune response to harmless substances, not a deficient one. They are distinct conditions with different underlying mechanisms.
Genetics and Environmental Factors in Allergies
The development of allergies is influenced by a complex interplay of genetic and environmental factors. A family history of allergies increases the risk of developing allergies. Environmental exposures, such as pollution, early exposure to certain allergens, and hygiene hypothesis (reduced exposure to microbes in early childhood) also contribute to the development of allergies.
Can Allergies Coexist with Other Immune Conditions?
Yes, it is possible to have allergies and other immune conditions simultaneously. For example, some individuals with allergies may also have autoimmune diseases, where the immune system attacks the body's own tissues. While allergies represent an overactive immune response, autoimmune diseases represent a misdirected immune response. The presence of one condition doesn't preclude the other.
| Condition | Immune System State | Characteristics |
|---|---|---|
| Allergies | Overactive | Exaggerated response to harmless substances; release of histamine; IgE antibodies involved. |
| Immunodeficiency | Weakened | Increased susceptibility to infections; impaired ability to fight off pathogens. |
| Autoimmune Disease | Misdirected | Immune system attacks the body's own tissues; chronic inflammation. |
Do allergies make your immune system weak?
No, allergies do not make your immune system weak. Instead, allergies represent a misdirected immune response. A healthy immune system is capable of differentiating between harmful substances (pathogens) and harmless substances (allergens). In individuals with allergies, the immune system mistakenly identifies a harmless substance, like pollen or pet dander, as a threat. This triggers an immune response that is disproportionate to the actual threat, leading to allergic symptoms. The immune system itself is functioning, perhaps even over-functioning, but it is doing so incorrectly. While experiencing allergy symptoms may leave you feeling unwell, the underlying immune system is not fundamentally weak. In fact, a weakened immune system might be less likely to produce a strong allergic response. This is because it is less capable of mounting an immune reaction of any kind, whether appropriate or inappropriate.
The Misguided Immune Response in Allergies
Allergies are a result of the immune system's inappropriate response to otherwise harmless substances known as allergens. When exposed to an allergen, the body's immune system, specifically the IgE antibodies, mistakenly identifies it as a threat. This leads to the release of histamine and other inflammatory chemicals, resulting in allergic symptoms. This is a hyperactive, rather than a weakened, immune response.
- IgE antibodies bind to mast cells and basophils.
- Upon re-exposure to the allergen, it cross-links with the IgE antibodies.
- This triggers the release of inflammatory mediators like histamine, causing allergy symptoms.
Allergic Symptoms and Immune Function
The symptoms experienced during an allergic reaction – such as sneezing, itching, rash, or difficulty breathing – are a direct consequence of this overactive immune response. These symptoms are not indicators of an overall weak immune system. Instead, they signify an immune system that is reacting excessively to a non-threatening substance. A truly weakened immune system would struggle to mount anysignificant immune response, allergic or otherwise.
- Sneezing and runny nose are attempts to expel the allergen.
- Itching and rash result from the release of histamine.
- Difficulty breathing can be caused by bronchoconstriction in the lungs.
Differentiating Allergy from Immune Deficiency
It's crucial to distinguish between an allergic reaction and an actual immune deficiency. An immune deficiency means the immune system is compromised and unable to effectively fight off infections. Individuals with immune deficiencies are more susceptible to various infections, whereas individuals with allergies primarily experience symptoms related to exposure to specific allergens.
- Immune deficiency leads to increased susceptibility to infections.
- Allergies cause reactions to specific harmless substances.
- Treatment strategies differ significantly between the two conditions.
The Role of Genetics and Environment in Allergies
The development of allergies is complex and influenced by both genetic predisposition and environmental factors. A family history of allergies increases an individual's risk. However, this increased risk does not equate to a weaker immune system; rather, it indicates a genetic tendency towards an overactive immune response to specific allergens. Environmental exposures also play a significant role in triggering allergic reactions.
- Genetic factors influence the production of IgE antibodies.
- Environmental factors like exposure to pollutants and certain foods can trigger allergic reactions.
- Hygiene hypothesis suggests that reduced exposure to microbes in early childhood may increase allergy risk.
Managing Allergies vs. Boosting Immunity
Managing allergies focuses on reducing exposure to specific allergens and mitigating the effects of allergic reactions through medications like antihistamines or immunotherapy. Strengthening a healthy immune system, on the other hand, involves practices such as maintaining a healthy lifestyle, getting enough sleep, eating a balanced diet, and engaging in regular exercise. These practices support the overall immune system's ability to effectively fight infections, but they do not address the misdirected immune response characteristic of allergies.
- Allergy management focuses on avoiding allergens and symptom relief.
- Immune system boosting involves lifestyle changes to support overall immune function.
- These are distinct strategies addressing different aspects of health.
Are you weak if you have allergies?

No, having allergies does not inherently make you weak. Allergies are a result of your immune system overreacting to a harmless substance, like pollen or pet dander. This overreaction causes symptoms like sneezing, itching, runny nose, and potentially more severe reactions. While these symptoms can be debilitating and significantly impact your quality of life, they don't indicate underlying physical weakness. The severity of allergic reactions varies greatly from person to person, and some individuals manage their allergies effectively with medication or lifestyle changes, leading to a normal, active life. The presence of allergies is a medical condition, not a measure of overall physical strength or fitness.
Severity of Allergic Reactions
The severity of allergic reactions plays a crucial role in how allergies impact daily life. Mild allergies, like seasonal hay fever, might cause minor discomfort but rarely affect overall strength or energy levels. However, severe allergic reactions, such as anaphylaxis, can be life-threatening and require immediate medical attention. These severe reactions are certainly debilitating, but again, this is due to the intense immune response, not an inherent weakness. The intensity of the allergic response, not the presence of the allergy itself, determines any potential impact on physical ability.
- Mild allergies: Usually manageable with over-the-counter medications.
- Moderate allergies: May require prescription medications and lifestyle adjustments.
- Severe allergies: Can cause life-threatening reactions and require emergency medical care.
Impact on Energy Levels
While allergies themselves don't cause weakness, the symptoms they produce can significantly impact energy levels. Sleep disruption due to nighttime allergy symptoms, such as coughing or sneezing, can lead to fatigue. Similarly, daytime symptoms can make it difficult to focus and participate in physical activities. Lack of sleep and persistent discomfort can certainly drain energy, but this is a consequence of the allergy symptoms, not a fundamental weakness.
- Sleep deprivation: A common consequence of allergy symptoms like nighttime coughing and sneezing.
- Reduced physical activity: Discomfort and fatigue can limit participation in exercise and daily activities.
- Medication side effects: Some allergy medications can cause drowsiness or other side effects that impact energy levels.
Allergies and the Immune System
It's important to understand that allergies are a sign of an overactive, not a weak, immune system. The immune system's role is to protect the body from harmful substances. In people with allergies, the immune system mistakenly identifies harmless substances as threats, triggering an inflammatory response. This response, while causing unpleasant symptoms, demonstrates the immune system's vigorous activity, not weakness.
- Overactive immune response: Allergies are characterized by an excessive immune response to harmless substances.
- Misidentification of allergens: The immune system mistakenly identifies harmless substances as threats.
- Inflammatory response: The body's attempt to fight off the perceived threat, causing allergy symptoms.
Managing Allergies and Maintaining Strength
Effective allergy management is key to maintaining energy levels and overall health. This may involve various strategies, including medication, immunotherapy, and lifestyle changes. Proper management of allergies allows individuals to live active, healthy lives, unburdened by debilitating symptoms. While managing allergies may require effort, it doesn't signify weakness; it demonstrates proactive health management.
- Medication: Antihistamines, decongestants, and other medications can alleviate allergy symptoms.
- Immunotherapy: Allergy shots or sublingual immunotherapy can help desensitize the immune system to allergens.
- Lifestyle changes: Avoiding allergens and maintaining good hygiene practices can minimize exposure.
Allergies and Physical Fitness
While allergy symptoms can temporarily hinder physical activity, allergies themselves do not inherently impair physical fitness. Individuals with allergies can achieve and maintain a high level of physical fitness with appropriate allergy management. Regular exercise, even with allergies, is beneficial for overall health and well-being. The key is to find strategies to manage allergy symptoms during workouts, such as timing activities to avoid peak pollen hours or using appropriate medications.
- Exercise planning: Scheduling workouts to avoid peak allergen exposure times.
- Medication timing: Taking allergy medications before exercise to minimize symptom interference.
- Appropriate attire: Wearing protective clothing, like masks or sunglasses, to limit allergen exposure during workouts.
How can I strengthen my immune system against allergies?

How Can I Strengthen My Immune System Against Allergies?
Strengthening your immune system to better manage allergies is a multifaceted approach that focuses on reducing inflammation and modulating your immune response. It's crucial to understand that you can't completely eliminate allergies, but you can significantly reduce their severity and frequency. This involves a combination of lifestyle changes, dietary adjustments, and in some cases, medical interventions guided by your doctor or allergist.
Reduce Inflammation
Chronic inflammation plays a significant role in allergic reactions. Reducing inflammation throughout your body can help lessen the severity of allergic responses. This is achieved through various methods focusing on a holistic approach to health.
- Eat an anti-inflammatory diet: Focus on fruits, vegetables, whole grains, and lean proteins. Avoid processed foods, sugary drinks, and saturated fats.
- Manage stress: Chronic stress can exacerbate inflammation. Practice stress-reducing techniques like yoga, meditation, or deep breathing exercises.
- Get enough sleep: Adequate sleep is crucial for immune function and overall health. Aim for 7-9 hours of quality sleep per night.
Optimize Gut Health
The gut microbiome plays a crucial role in immune function. A healthy gut, teeming with beneficial bacteria, can help regulate immune responses and reduce inflammation. Maintaining a balanced gut flora is therefore a key strategy in allergy management.
- Consume probiotics: Incorporate foods rich in probiotics, such as yogurt, kefir, and sauerkraut, or consider probiotic supplements.
- Eat prebiotic foods: Prebiotics feed beneficial bacteria in your gut. Good sources include onions, garlic, bananas, and oats.
- Limit antibiotic use: Antibiotics can disrupt the gut microbiome. Only use them when necessary and as prescribed by a doctor.
Boost Your Antioxidant Intake
Antioxidants combat oxidative stress, a process linked to inflammation and allergic reactions. By increasing your antioxidant intake, you can help protect your cells from damage and reduce inflammation.
- Eat antioxidant-rich foods: Include berries, dark leafy greens, nuts, and seeds in your diet.
- Consider antioxidant supplements: Talk to your doctor before taking any supplements, especially if you have underlying health conditions.
- Limit exposure to environmental toxins: Toxins contribute to oxidative stress. Minimize exposure to pollutants, smoke, and other environmental hazards.
Maintain a Healthy Lifestyle
A healthy lifestyle contributes significantly to a robust immune system. This is not just about diet but also encompasses physical activity and avoidance of harmful habits. A holistic approach yields the best results.
- Regular exercise: Physical activity boosts immune function and reduces inflammation.
- Avoid smoking: Smoking weakens the immune system and exacerbates allergies.
- Limit alcohol consumption: Excessive alcohol consumption can negatively impact immune function.
Consult with a Healthcare Professional
It's crucial to consult with your doctor or allergist before making significant dietary changes or starting any new supplements, especially if you have pre-existing health conditions. They can assess your specific needs, diagnose allergies accurately, and recommend appropriate treatments. Professional guidance is invaluable in managing allergies effectively.
- Allergy testing: Undergo appropriate allergy testing to identify your specific allergens.
- Immunotherapy: Discuss immunotherapy options with your allergist, such as allergy shots or sublingual immunotherapy.
- Medication management: Work with your doctor to manage your allergy symptoms with medications such as antihistamines or corticosteroids.
Why do I have allergies all the time?
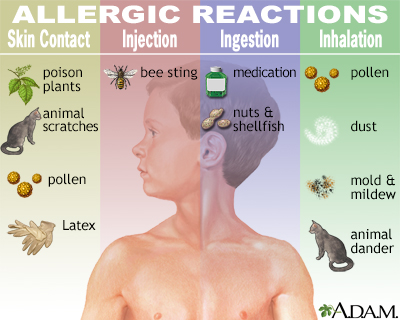
Experiencing allergies constantly can be incredibly frustrating and disruptive. There isn't a single, simple answer to why some people have persistent allergies, as it's a complex interplay of genetic predisposition, environmental factors, and immune system responses. Your immune system, in essence, mistakenly identifies harmless substances as dangerous invaders, triggering a cascade of reactions that manifest as allergy symptoms. These substances, known as allergens, can include pollen, dust mites, pet dander, mold, certain foods, insect stings, and medications. The severity and frequency of your allergies depend on several contributing factors.
Genetic Predisposition
A family history of allergies significantly increases your risk. If your parents, siblings, or other close relatives suffer from allergies, asthma, or eczema, you are more likely to develop them yourself. This doesn't guarantee you'll have allergies, but it substantially raises your probability. Genes influence how your immune system develops and responds to environmental stimuli. While not all genes responsible for allergic tendencies are identified, research continues to unveil the genetic basis of allergic diseases.
- Inherited immune system characteristics can make you more prone to overreacting to allergens.
- Family history often indicates a pattern of heightened immune sensitivity.
- Genetic testing can sometimes help identify specific predispositions, but it's not always conclusive.
Environmental Exposure
Constant exposure to allergens plays a crucial role in the persistence of your allergy symptoms. Living in an area with high pollen counts, keeping pets indoors, residing in a damp environment conducive to mold growth, or frequently encountering specific food allergens can continuously trigger your allergic reactions. The more exposure, the more likely your immune system will remain sensitized and reactive.
- High pollen counts in spring and fall can trigger prolonged allergy seasons.
- Dust mites thrive in warm, humid environments, often found in bedding and carpets.
- Mold exposure in homes or workplaces can lead to year-round allergic responses.
Immune System Dysregulation
Your immune system's response is central to allergies. In allergic individuals, the immune system overreacts to harmless substances by producing IgE antibodies. These antibodies then trigger the release of histamine and other inflammatory chemicals, leading to symptoms like sneezing, itching, and inflammation. This overactive immune response can become chronic in some people.
- IgE antibody production is a key element in the allergic response.
- Histamine release causes many of the characteristic symptoms of allergies.
- Chronic inflammation can contribute to persistent allergic symptoms.
The Hygiene Hypothesis
The hygiene hypothesis suggests that increased hygiene and reduced exposure to certain microbes in early childhood might contribute to a higher risk of allergies. Exposure to diverse microorganisms in the environment can help train the immune system to distinguish between harmful and harmless substances. Lack of such exposure may lead to an imbalanced immune response, making it more prone to allergies.
- Limited exposure to diverse microbes might lead to an under-developed immune system.
- Early childhood exposure to pets or farm animals can reduce allergy risk in some children.
- Reducing exposure to excessive hygiene products might promote a more balanced immune response.
Underlying Medical Conditions
Certain medical conditions can exacerbate allergies or cause similar symptoms. For example, some individuals with asthma experience allergies as a comorbidity, meaning they frequently occur together. Other conditions can also play a role, so it's vital to discuss any persistent allergic symptoms with a doctor to rule out any underlying health issues that may be contributing factors. Proper diagnosis is crucial for appropriate management.
- Asthma and allergies often share underlying mechanisms and frequently occur together.
- Other autoimmune disorders can sometimes influence allergy symptoms.
- Consulting a doctor is essential to rule out underlying medical conditions that mimic allergies.
Do allergies mean I have a weak immune system?
No, allergies don't necessarily indicate a weak immune system. In fact, it's quite the opposite. Allergies are a sign of an overactive immune system. Your immune system is designed to protect you from harmful substances like bacteria and viruses. When you have an allergy, your immune system mistakenly identifies a harmless substance, such as pollen, pet dander, or certain foods, as a threat. This triggers an exaggerated response, releasing histamine and other chemicals that cause allergic symptoms like sneezing, itching, rash, and swelling. A truly weak immune system would be less likely to overreact to harmless substances; it would struggle to fight off actual infections. Therefore, while allergies are a sign of immune system dysfunction, they demonstrate hypersensitivity rather than weakness. The immune system is working, but it's working incorrectly.
My child has lots of allergies. Does this mean their immune system is weak?
Similar to the adult case, multiple allergies in children don't signify a weak immune system, but rather a hyperactive one. The immune system of a child is still developing, and this developmental process can sometimes lead to a higher likelihood of allergic reactions. While some children might have a predisposition to allergies due to genetics, the body's response is still an overreaction, not an under-reaction. The presence of many allergies might prompt a doctor to investigate for underlying conditions, but the allergies themselves are a sign of an immune system that is overly sensitive, not deficient. A weak immune system would manifest in more frequent and severe infections, not primarily allergic reactions.
I have allergies and frequent colds. Does this indicate a weakened immune system?
Experiencing both allergies and frequent colds can be confusing, as they seem contradictory. While allergies show an overactive immune response to harmless substances, frequent colds suggest a potentially compromised immune system's ability to fight off infections. However, these two conditions don't necessarily indicate a universally weakened immune system. The allergies are a separate issue of immune system dysregulation, not necessarily a complete failure. It's possible to have an immune system that overreacts to harmless allergens while simultaneously struggling to effectively combat viruses. In this scenario, the frequent colds could be due to various factors, such as exposure to many viruses or underlying health conditions, unrelated to the allergic response itself. Consulting a doctor is crucial to determine the underlying causes of both the allergies and the frequent colds.
Can strengthening my immune system help with allergies?
While strengthening your immune system through healthy habits like diet, exercise, and sufficient sleep is beneficial for overall health, it won't directly "cure" allergies. The issue with allergies isn't that your immune system is weak, but that it's overly reactive to specific substances. Strengthening it won't change the way it identifies these harmless substances as threats. While a healthy lifestyle can support your body's ability to manage allergy symptoms and potentially reduce their severity by improving overall health, it won't address the root cause of the allergic reaction. Allergy management typically involves strategies like allergy shots (immunotherapy), medication to control symptoms, and avoidance of allergens. Therefore, focusing on improving general health is helpful but not a direct solution for allergies.
Deja una respuesta