What can be mistaken for allergies

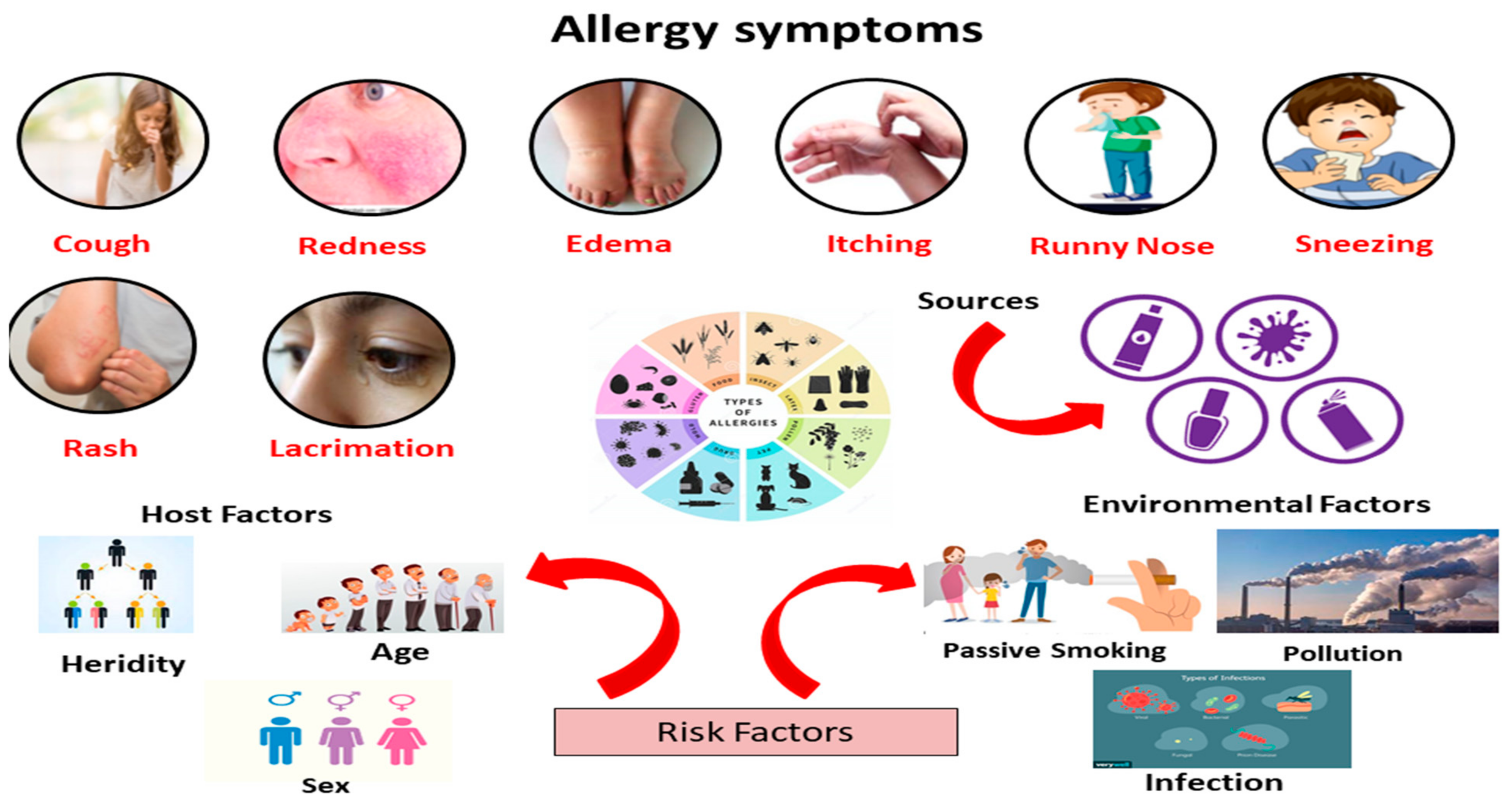
It's a hot summer day, and you're feeling a bit under the weather. Your nose is runny, your eyes are watery, and you're sneezing like crazy. You think you might have allergies, but what if you're wrong? Here are a few things that can be mistaken for allergies:
What Conditions Often Mimic Allergic Reactions?
Many conditions can present symptoms similar to allergies, making diagnosis challenging. It's crucial to see a doctor for proper evaluation to determine the underlying cause and receive appropriate treatment. Misdiagnosis can lead to ineffective or even harmful treatments. This is particularly true since many conditions share similar symptoms like skin rashes, sneezing, coughing, and breathing difficulties.
Food Intolerances
Unlike allergies, which involve the immune system, food intolerances are due to a digestive problem. Lactose intolerance, for example, causes symptoms like bloating, gas, and diarrhea after consuming dairy, but it doesn't involve an immune response like a milk allergy. Gluten sensitivity, another common example, can manifest as digestive issues, fatigue, and skin problems but is not a true allergy. The symptoms can overlap significantly with allergic reactions, making differentiation crucial.
Environmental Irritants
Exposure to certain environmental irritants, such as strong chemicals, dust, or pollutants, can trigger symptoms resembling allergies. These irritants cause direct inflammation and irritation of the respiratory tract or skin, leading to symptoms like coughing, sneezing, itchy eyes, and skin rashes. Unlike allergies, however, there's no immune system involvement. For example, irritant contact dermatitis is triggered by direct skin contact with a substance while allergic contact dermatitis involves an immune response.
Infections
Various infections, such as the common cold, influenza, or sinusitis, can mimic allergic reactions. These infections lead to inflammation in the respiratory tract causing similar symptoms such as runny nose, cough, congestion, and sneezing. Differentiating between allergies and infections is crucial for treatment, as allergies require different management strategies than infections.
Medication Side Effects
Many medications can cause allergic-like reactions as a side effect. These can range from mild skin rashes to severe reactions like anaphylaxis. These reactions are not true allergies, but rather a form of drug hypersensitivity. It's important to carefully note any medication side effects and report them to your doctor immediately. This includes over-the-counter drugs and herbal supplements.
Genetic and Autoimmune Conditions
Certain genetic and autoimmune conditions can present symptoms similar to allergies. For instance, eczema (atopic dermatitis) is a chronic inflammatory skin condition often associated with allergies but has a distinct underlying mechanism. Autoimmune conditions like lupus can also manifest with symptoms similar to allergic rhinitis (hay fever) due to inflammation in different body systems. Accurate diagnosis is critical to distinguish between these and implement appropriate management.
| Condition | Symptoms | Key Difference from Allergies |
|---|---|---|
| Food Intolerance | Bloating, gas, diarrhea | No immune system involvement |
| Environmental Irritants | Cough, sneezing, itchy eyes, rash | Direct irritation, no immune response |
| Infection (e.g., common cold) | Runny nose, cough, congestion | Caused by a pathogen |
| Medication Side Effects | Rash, hives, swelling | Drug hypersensitivity, not a true allergy |
| Autoimmune Conditions (e.g., Lupus) | Various, can mimic allergies | Dysfunctional immune system attacking the body |
https://youtube.com/watch?v=60-seconds-allergies
What Conditions Often Mimic Allergic Reactions?
Many conditions can present symptoms similar to allergies, making diagnosis challenging. It's crucial to see a doctor for proper evaluation to determine the underlying cause and receive appropriate treatment. Misdiagnosis can lead to ineffective or even harmful treatments. This is particularly true since many conditions share similar symptoms like skin rashes, sneezing, coughing, and breathing difficulties.
Food Intolerances
Unlike allergies, which involve the immune system, food intolerances are due to a digestive problem. Lactose intolerance, for example, causes symptoms like bloating, gas, and diarrhea after consuming dairy, but it doesn't involve an immune response like a milk allergy. Gluten sensitivity, another common example, can manifest as digestive issues, fatigue, and skin problems but is not a true allergy. The symptoms can overlap significantly with allergic reactions, making differentiation crucial.
Environmental Irritants
Exposure to certain environmental irritants, such as strong chemicals, dust, or pollutants, can trigger symptoms resembling allergies. These irritants cause direct inflammation and irritation of the respiratory tract or skin, leading to symptoms like coughing, sneezing, itchy eyes, and skin rashes. Unlike allergies, however, there's no immune system involvement. For example, irritant contact dermatitis is triggered by direct skin contact with a substance while allergic contact dermatitis involves an immune response.
Infections
Various infections, such as the common cold, influenza, or sinusitis, can mimic allergic reactions. These infections lead to inflammation in the respiratory tract causing similar symptoms such as runny nose, cough, congestion, and sneezing. Differentiating between allergies and infections is crucial for treatment, as allergies require different management strategies than infections.
Medication Side Effects
Many medications can cause allergic-like reactions as a side effect. These can range from mild skin rashes to severe reactions like anaphylaxis. These reactions are not true allergies, but rather a form of drug hypersensitivity. It's important to carefully note any medication side effects and report them to your doctor immediately. This includes over-the-counter drugs and herbal supplements.
Genetic and Autoimmune Conditions
Certain genetic and autoimmune conditions can present symptoms similar to allergies. For instance, eczema (atopic dermatitis) is a chronic inflammatory skin condition often associated with allergies but has a distinct underlying mechanism. Autoimmune conditions like lupus can also manifest with symptoms similar to allergic rhinitis (hay fever) due to inflammation in different body systems. Accurate diagnosis is critical to distinguish between these and implement appropriate management.
| Condition | Symptoms | Key Difference from Allergies |
|---|---|---|
| Food Intolerance | Bloating, gas, diarrhea | No immune system involvement |
| Environmental Irritants | Cough, sneezing, itchy eyes, rash | Direct irritation, no immune response |
| Infection (e.g., common cold) | Runny nose, cough, congestion | Caused by a pathogen |
| Medication Side Effects | Rash, hives, swelling | Drug hypersensitivity, not a true allergy |
| Autoimmune Conditions (e.g., Lupus) | Various, can mimic allergies | Dysfunctional immune system attacking the body |
What illness can mimic allergies?
Many illnesses can mimic allergies, making diagnosis challenging. Symptoms such as sneezing, coughing, itchy eyes, and a runny nose are common to both allergies and several other conditions. The key difference lies in the underlying cause: allergies are triggered by an immune system response to a harmless substance (allergen), while other illnesses have different origins. Accurate diagnosis requires careful consideration of symptoms, medical history, and potentially, further testing.
Respiratory Infections
Respiratory infections, such as the common cold, influenza (flu), and bronchitis, frequently share symptoms with allergies. These infections are caused by viruses or bacteria, leading to inflammation in the respiratory tract. While allergies cause a reaction to specific allergens, respiratory infections are caused by infectious agents. Distinguishing between them can be tricky, especially in the early stages.
- Symptoms overlap significantly: Both can present with sneezing, runny nose, cough, and congestion.
- Infections are typically self-limiting: They often resolve within a few days to weeks without specific treatment.
- Allergies often show seasonal patterns or are triggered by specific exposures: This can help differentiate them from infections.
Sinusitis
Sinusitis, an inflammation of the sinuses, can manifest with symptoms similar to allergies. However, sinusitis is caused by infection, inflammation, or structural issues within the sinuses, resulting in nasal congestion, facial pain or pressure, and post-nasal drip. Unlike allergic rhinitis (hay fever), sinusitis often involves more intense pain and pressure in the face.
- Facial pain and pressure: This is a key differentiating factor from allergies.
- Thick, discolored nasal discharge: Allergies usually produce clear or whitish mucus.
- Longer duration of symptoms: Sinusitis symptoms typically last longer than allergic reactions.
Gastroesophageal Reflux Disease (GERD)
While not typically associated with respiratory symptoms, GERD can sometimes mimic allergies by causing a chronic cough or throat irritation. GERD occurs when stomach acid flows back into the esophagus, irritating the lining. The resulting cough can be mistaken for an allergic reaction, particularly if it occurs frequently.
- Heartburn and acid reflux: These are key symptoms that help distinguish GERD from allergies.
- Cough that worsens after eating or lying down: This pattern differs from the typically less time-dependent allergy symptoms.
- Sore throat and hoarseness: These are common symptoms of GERD, less common in allergic reactions.
Asthma
Asthma, a chronic respiratory condition, can overlap significantly with allergies. Many people with asthma are also allergic to certain substances (allergic asthma). However, asthma is characterized by airway inflammation and bronchospasm, leading to wheezing, shortness of breath, and chest tightness, which may or may not be triggered by an allergen.
- Wheezing and shortness of breath: These are distinguishing features of asthma that are less common in allergies.
- Chest tightness: A characteristic symptom of asthma.
- Response to asthma medications: Asthma symptoms are often relieved by inhalers and other asthma medications, whereas allergy symptoms may not respond to these treatments.
Chronic Obstructive Pulmonary Disease (COPD)
COPD, a progressive lung disease, shares some symptoms with allergies, such as chronic cough and increased mucus production. However, COPD is characterized by airflow limitation, typically due to long-term exposure to irritants like cigarette smoke. It's usually more severe and progressive than allergy-related symptoms.
- Progressive shortness of breath: This is a hallmark symptom of COPD, gradually worsening over time.
- Chronic cough with mucus production: The cough is often persistent and may produce large amounts of mucus.
- History of smoking or exposure to irritants: A significant risk factor for COPD.
What can be confused for allergies?
:max_bytes(150000):strip_icc()/how-do-you-know-if-you-have-allergies-5202927-FINAL-c74839b604b942b1ba9a658f0fc245d2.jpg)
Many conditions can mimic allergic reactions, making diagnosis challenging. Symptoms like sneezing, coughing, rash, and itching are common to both allergies and other health problems. Accurate diagnosis requires careful consideration of symptoms, their timing, and other factors such as family history and exposure to potential triggers. A healthcare professional can help differentiate between allergies and other conditions.
Non-Allergic Rhinitis
Non-allergic rhinitis is a condition causing similar symptoms to allergies, such as a runny nose, sneezing, and nasal congestion. However, unlike allergies, it's not triggered by an immune response to a specific allergen. Instead, it can be caused by various factors including:
- Irritants: Strong smells, fumes, and dust.
- Hormonal changes: Fluctuations in estrogen can trigger symptoms.
- Medications: Certain drugs can have nasal congestion as a side effect.
Food Intolerance
Food intolerance is often confused with food allergies. While both involve adverse reactions to food, the mechanisms differ significantly. Food allergies involve an immune response, causing potentially life-threatening reactions. Food intolerances, on the other hand, are not immune-mediated; they cause digestive discomfort like bloating, gas, or diarrhea. These symptoms are generally less severe than allergic reactions.
- Symptoms are often delayed compared to allergic reactions.
- Reactions tend to be less severe, typically limited to the digestive system.
- Testing differs significantly; food allergy testing involves blood or skin prick tests, while food intolerance testing may involve elimination diets.
Environmental Irritants
Exposure to certain environmental irritants can trigger symptoms similar to allergies. These irritants, unlike allergens, don't provoke an immune response, yet they can cause significant discomfort. Examples include:
- Air pollution: Smog, vehicle exhaust, and industrial emissions can trigger respiratory symptoms.
- Chemical fumes: Cleaning products, paints, and solvents can irritate the eyes, nose, and throat.
- Dust and other particles: These can irritate the respiratory tract, even in individuals without allergies.
Infections
Various infections can mimic allergic symptoms. Viral infections, such as the common cold, frequently cause sneezing, runny nose, and congestion – often mistaken for allergies. Similarly, some bacterial infections can lead to symptoms that overlap with allergic reactions. Careful consideration of symptoms and timing is crucial to differentiate between allergies and infection.
- Infections often involve additional symptoms like fever, cough, or body aches, not typically seen in allergies.
- The duration is different; allergies often have seasonal patterns while infections are typically shorter lived.
- Infections often respond to antibiotics or antiviral medications, whereas allergies may not.
Autoimmune Diseases
Certain autoimmune diseases can share symptoms with allergies, adding to the diagnostic challenge. Autoimmune disorders, where the body's immune system attacks its own tissues, can manifest with various symptoms including skin rashes, respiratory issues, and digestive problems. Correct diagnosis is crucial, as treatment for autoimmune diseases differs significantly from allergy management.
- Autoimmune diseases often involve systemic symptoms affecting multiple organ systems.
- Diagnosis often involves blood tests to identify specific autoantibodies.
- Treatment focuses on managing the immune response, often with immunosuppressant medications.
What autoimmune disease mimics allergies?
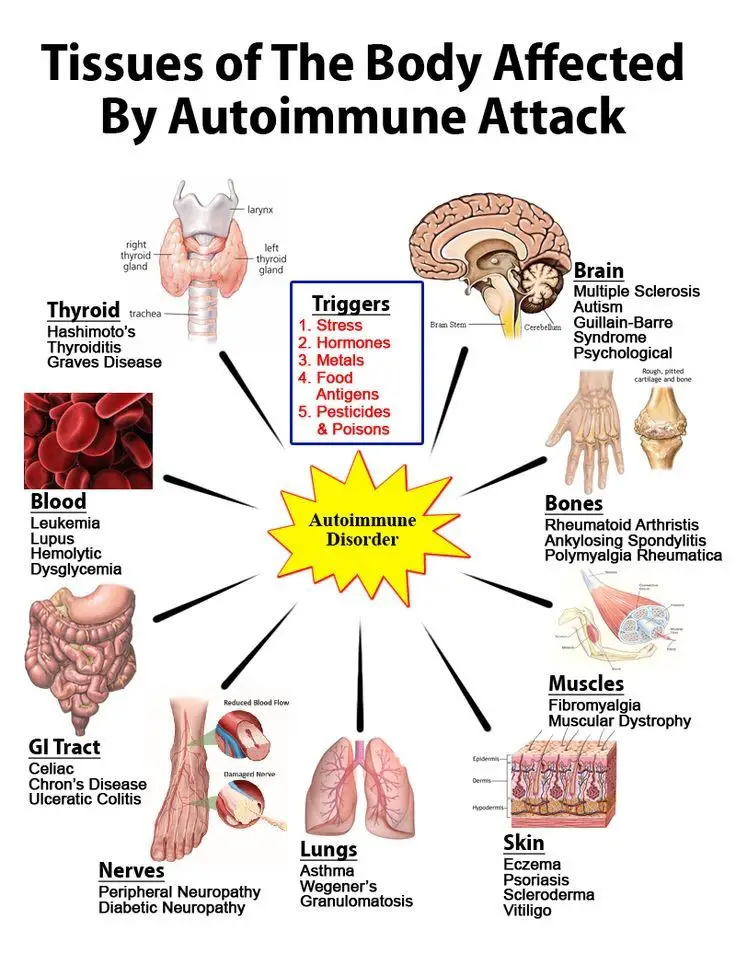
Several autoimmune diseases can mimic allergic reactions due to overlapping symptoms. The most common culprit is autoimmune urticaria (chronic spontaneous urticaria). This condition causes hives (urticaria) and angioedema (swelling) similar to allergic reactions, but it's triggered by the immune system attacking its own tissues, not an external allergen. Other autoimmune conditions, while less frequently presenting like allergies, can share some symptoms, leading to diagnostic challenges. The key difference lies in the underlying cause: allergies involve a reaction to a foreign substance, while autoimmune diseases involve the immune system malfunctioning and attacking the body's own cells.
Autoimmune Urticaria: The Master Mimic
Autoimmune urticaria is a prime example of an autoimmune disease mimicking allergies. The characteristic symptom, hives, can be indistinguishable from those caused by an allergic response. However, unlike allergic urticaria, which is triggered by a specific allergen, autoimmune urticaria is caused by autoantibodies targeting the mast cells, leading to histamine release and consequent inflammation. This can manifest as:
- Itchy welts or hives that appear and disappear unpredictably.
- Angioedema, or swelling beneath the skin, particularly affecting the face, lips, and throat.
- Symptoms lasting longer than six weeks, a key differentiator from acute allergic reactions.
Systemic Lupus Erythematosus (SLE) and Allergic Manifestations
Systemic lupus erythematosus (SLE) is a complex autoimmune disease that can impact multiple organ systems. While not directly mimicking allergies, SLE can present with symptoms such as rashes and skin lesions that resemble allergic reactions. The skin involvement in SLE can be triggered by various factors, including sun exposure, making it challenging to differentiate from photosensitivity reactions associated with allergies.
- Skin rashes, ranging from mild to severe, often appearing on sun-exposed areas.
- Joint pain and inflammation, similar to symptoms experienced in some allergic reactions.
- Fatigue, a non-specific symptom also seen in allergic reactions.
Rheumatoid Arthritis and its Overlapping Symptoms
Although primarily affecting joints, rheumatoid arthritis (RA) can sometimes exhibit symptoms that overlap with allergic manifestations. While not directly causing hives or typical allergic reactions, the inflammation associated with RA can lead to skin conditions that may be mistaken for allergy-induced skin issues. Accurate diagnosis relies on identifying the underlying autoimmune process, not just focusing on similar skin symptoms.
- Joint pain and swelling often mistaken for inflammation caused by allergies.
- Skin rashes in certain RA patients may resemble allergic dermatitis.
- Fatigue and malaise, common to both RA and some allergic reactions.
Vasculitis and its Cutaneous Manifestations
Vasculitis encompasses various conditions involving inflammation of blood vessels. Certain types of vasculitis can cause skin lesions and rashes reminiscent of allergic reactions. However, vasculitis is an autoimmune condition, with the immune system attacking the blood vessel walls instead of responding to an allergen. Differentiating between vasculitis and allergic reactions requires careful evaluation of symptoms and diagnostic testing.
- Purpura, a type of rash characterized by purple discoloration of the skin.
- Ulcers or sores on the skin or mucous membranes.
- Systemic symptoms, like fever, fatigue, and weight loss, which are uncommon in typical allergic reactions.
Hashimoto's Thyroiditis and its Indirect Link to Allergies
Hashimoto's thyroiditis, an autoimmune disease targeting the thyroid gland, doesn't directly mimic allergic reactions. However, there's a notable association between autoimmune conditions and a higher prevalence of allergies. Individuals with Hashimoto's might exhibit a heightened sensitivity to certain substances due to an overall compromised immune system. This doesn't mean Hashimoto's causes allergic-like symptoms directly; rather, it highlights the complex interplay between the immune system and the propensity for both autoimmune disorders and allergies.
- Thyroid dysfunction can lead to symptoms like fatigue and skin changes, which can sometimes be mistaken for allergic symptoms.
- Increased sensitivity to certain environmental factors may be present but is not a direct mimic of allergic reactions.
- Underlying immune dysregulation in Hashimoto's might predispose individuals to developing allergies.
What can be mistaken for an allergic reaction?

What Can Be Mistaken for an Allergic Reaction?
Many conditions can mimic the symptoms of an allergic reaction, making accurate diagnosis crucial. This is because allergic reactions involve the body's immune system overreacting to a harmless substance, leading to a range of symptoms. However, several other medical issues can produce similar symptoms, potentially leading to misdiagnosis and inappropriate treatment. It's essential to consult a healthcare professional for proper evaluation and diagnosis if you experience symptoms suggestive of an allergic reaction.
Viral Infections
Viral infections, such as the common cold or the flu, can cause symptoms that overlap significantly with allergic reactions. These include runny nose, sneezing, coughing, and sometimes even skin rashes. The key difference often lies in the duration and accompanying symptoms. Allergic reactions are typically triggered by exposure to a specific allergen and may resolve upon avoidance, while viral infections have a more defined course of illness, usually resolving within a certain timeframe.
- Runny nose and congestion are common in both viral infections and allergies.
- Coughing can be present in both.
- Fever is more characteristic of a viral infection, not typically seen in allergies.
Food Intolerance
Food intolerance differs from a true allergic reaction. While both can cause gastrointestinal distress, food intolerance involves difficulty digesting a specific food, leading to symptoms like bloating, gas, and diarrhea. These symptoms often appear more slowly than those of an allergic reaction, and are generally less severe. True allergic reactions to food can be life-threatening, causing anaphylaxis, while intolerances are typically less severe.
- Digestive symptoms are common in both, but the onset and severity differ significantly.
- Food intolerance often involves digestive discomfort rather than immune system response.
- Anaphylaxis is a life-threatening allergic reaction, not usually associated with food intolerance.
Medication Side Effects
Many medications can trigger reactions that resemble allergic reactions. These side effects can manifest as rashes, itching, swelling, or even difficulty breathing. However, unlike true allergies, these reactions are not caused by the body's immune system. Instead, they are a direct effect of the medication on the body. Careful review of medication history is important in distinguishing these from true allergic reactions.
- Rashes and hives are common side effects of some medications.
- Swelling may occur as a side effect, especially with certain drugs.
- Identifying the medication is crucial for determining the cause of the reaction.
Environmental Irritants
Exposure to environmental irritants such as smoke, dust, or strong chemicals can cause respiratory symptoms like coughing, sneezing, and shortness of breath. These symptoms can mimic those of an allergic reaction, but they are not mediated by the immune system. Instead, they are caused by direct irritation of the airways or skin. Avoiding the irritant usually resolves the symptoms.
- Irritant-induced reactions are not immune-mediated.
- Symptoms often resolve upon removal of the irritant.
- No specific antibody response is involved.
Autoimmune Diseases
Autoimmune diseases, where the body's immune system attacks its own tissues, can present with symptoms overlapping with allergic reactions. For example, certain autoimmune conditions can cause skin rashes, joint pain, or fatigue. The key is identifying the underlying autoimmune disorder, which often requires more extensive testing and a different treatment approach than that used for allergies.
- Systemic symptoms such as fatigue and joint pain are more common in autoimmune diseases.
- Specific autoantibodies may be present in autoimmune disorders, absent in allergies.
- Chronic and progressive nature is common in autoimmune diseases.
What are some common conditions often mistaken for allergies?
Many conditions share similar symptoms with allergies, leading to misdiagnosis. Viral infections, like the common cold or the flu, frequently cause sneezing, runny nose, and congestion – symptoms often associated with allergic rhinitis (hay fever). However, unlike allergies, viral infections usually involve fever, body aches, and potentially coughing. Furthermore, the duration of symptoms differs; viral infections typically resolve within a week or two, while allergy symptoms can persist for weeks or even months during allergen exposure. Another common culprit is non-allergic rhinitis, also known as vasomotor rhinitis. This condition causes similar nasal symptoms (stuffy nose, runny nose, sneezing) but isn't triggered by an immune response to allergens. Instead, it's often related to irritants like perfumes, smoke, or changes in temperature and humidity. Sinusitis, an inflammation of the sinuses, can also mimic allergy symptoms, presenting with facial pain, pressure, and nasal congestion. Differentiating sinusitis from allergies often requires a thorough examination by a healthcare professional to assess for signs of infection. Finally, certain medications can have side effects that mimic allergic reactions, such as a stuffy or runny nose. It is crucial to review your medications with your doctor if you suspect a reaction. Understanding these potential sources of confusion is vital for accurate diagnosis and treatment.
How can I tell if my symptoms are due to allergies or something else?
Distinguishing between allergies and other conditions requires careful consideration of several factors. The timing and duration of symptoms are key indicators. Allergic reactions often occur predictably when exposed to a specific allergen (e.g., pollen in spring, pet dander year-round). Symptoms typically improve or disappear when exposure ceases. In contrast, symptoms from other illnesses may appear randomly and persist for varying lengths. The type and severity of symptoms also provide valuable clues. Allergies commonly cause itchy eyes, nose, and throat, alongside nasal congestion and sneezing. Other conditions, such as viral infections, may include fever, body aches, and cough. A thorough medical history helps narrow down the possibilities. Detailing your symptoms, their timing, and any known triggers (e.g., specific foods, environments, pets) is crucial for diagnosis. Additionally, conducting allergy testing (skin prick test or blood test) can definitively determine if you have allergies and what you're allergic to. It's important to note that self-diagnosis can be misleading. Consulting a doctor or allergist is essential for accurate diagnosis and appropriate treatment.
What are some examples of conditions that mimic food allergies?
Several conditions can manifest as symptoms resembling food allergies, making accurate diagnosis challenging. Food intolerances are a common source of confusion. While food allergies trigger an immune response, food intolerances involve difficulty digesting specific foods, often due to enzyme deficiencies. Symptoms like bloating, gas, and diarrhea are common with food intolerances, but usually less severe than the anaphylaxis that can occur with food allergies. Gastrointestinal infections, caused by viruses or bacteria, can also cause symptoms similar to food allergies, including nausea, vomiting, diarrhea, and abdominal cramps. These infections are usually self-limiting and often accompanied by fever or other systemic symptoms. Eosinophilic esophagitis (EoE) is a chronic inflammatory condition affecting the esophagus. It can cause difficulty swallowing, heartburn, and abdominal pain, which might be mistaken for food allergies. However, unlike allergies, EoE is not typically associated with immediate reactions. Finally, certain medications, especially those with gastrointestinal side effects, can cause digestive problems that mimic food allergy symptoms. Accurate differentiation between these conditions and true food allergies requires a comprehensive evaluation by a medical professional including potentially elimination diets, endoscopy or allergy testing.
When should I seek medical attention for symptoms I think might be allergies?
While many allergy symptoms are manageable at home, it's crucial to seek medical attention under certain circumstances. If you experience symptoms consistent with a severe allergic reaction (anaphylaxis), including difficulty breathing, swelling of the throat or face, dizziness, or loss of consciousness, seek immediate emergency medical care. This is a life-threatening condition requiring prompt treatment. If your allergy symptoms are severe or persistent, despite over-the-counter medication, consulting a doctor is important. This is especially true if symptoms interfere with your daily activities or sleep. If you suspect a new allergy, or if your symptoms change significantly, a visit to your doctor or allergist is recommended for proper diagnosis and management. They can perform tests to confirm the allergen(s) and develop a personalized treatment plan. Also, if your allergy symptoms are accompanied by other unusual symptoms, such as fever, persistent cough, or unexplained weight loss, seeking medical attention is essential to rule out other potential conditions. Regular checkups and open communication with your healthcare provider are crucial for managing allergies effectively and avoiding potential complications.
Deja una respuesta