Does water flush out histamine

Does water flush out histamine? This is a question that has been asked by many people, as histamine is a compound that can cause a variety of symptoms, including sneezing, runny nose, itchy eyes, and headaches. While there is no definitive answer to this question, there is some evidence to suggest that drinking plenty of water may help to reduce histamine levels in the body.
Does Water Flush Out Histamine?
The simple answer is: no, water doesn't directly flush out histamine. Histamine is a molecule produced by your body, and it's involved in various bodily functions, most notably immune responses and inflammation. While drinking plenty of water is crucial for overall health and can indirectly support your body's processes for dealing with histamine, it doesn't directly remove histamine from your system the way a diuretic might remove excess sodium. Think of it like this: water helps your body function optimally, facilitating processes that indirectly manage histamine levels, but it's not a targeted removal mechanism.
How Histamine is Removed from the Body
Histamine is primarily broken down by an enzyme called histaminase. This enzyme is naturally present in the body and converts histamine into inactive metabolites that are then easily eliminated through the kidneys and urine. Factors like your diet, gut health, and overall health can influence the activity of histaminase. Therefore, while water itself doesn't directly remove histamine, adequate hydration supports kidney function, which is essential for the elimination of the histamine metabolites produced after the breakdown of histamine by histaminase. This means that staying hydrated is indirectly beneficial for histamine management.
The Role of Hydration in Histamine Management
Proper hydration is vital for overall health and contributes to efficient bodily functions. When you're well-hydrated, your kidneys can function optimally, filtering waste products, including the byproducts of histamine metabolism. Dehydration, on the other hand, can impair kidney function, potentially slowing down the elimination process. Therefore, adequate hydration supports the natural processes that clear histamine metabolites from the body. It doesn't remove histamine itself, but it supports the systems that do.
Dietary Factors Affecting Histamine Levels
Your diet significantly impacts histamine levels. High-histamine foods can trigger histamine release and exacerbate symptoms in individuals sensitive to it. These foods include fermented products, aged cheeses, cured meats, and certain fish. A diet low in histamine can help manage symptoms in those with histamine intolerance. Hydration plays a supporting role here, as efficient kidney function, supported by adequate water intake, helps remove histamine metabolites more effectively, regardless of dietary histamine intake. This doesn't remove histamine, just the aftereffects.
The Importance of Gut Health and Histamine
The gut microbiome plays a crucial role in histamine metabolism. A healthy gut microbiome with diverse bacterial populations helps regulate histamine production and breakdown. Probiotics, prebiotics, and a balanced diet all support a healthy gut. While water itself doesn't directly influence the gut microbiome, adequate hydration is crucial for overall gut function. A well-hydrated body ensures optimal gut motility and nutrient absorption, thus indirectly supporting a healthy gut microbiome that contributes to better histamine management.
| Factor | Effect on Histamine | Role of Water |
|---|---|---|
| Histaminase Enzyme | Breaks down histamine into metabolites | Water supports kidney function to eliminate metabolites |
| Kidney Function | Filters and eliminates histamine metabolites | Adequate hydration is essential for optimal kidney function |
| Gut Microbiome | Influences histamine production and breakdown | Hydration supports overall gut health |
| Diet | High-histamine foods increase histamine levels | Water helps eliminate histamine metabolites from high-histamine food consumption |
Does Water Flush Out Histamine?
The simple answer is: no, water doesn't directly flush out histamine. Histamine is a molecule produced by your body, and it's involved in various bodily functions, most notably immune responses and inflammation. While drinking plenty of water is crucial for overall health and can indirectly support your body's processes for dealing with histamine, it doesn't directly remove histamine from your system the way a diuretic might remove excess sodium. Think of it like this: water helps your body function optimally, facilitating processes that indirectly manage histamine levels, but it's not a targeted removal mechanism.
How Histamine is Removed from the Body
Histamine is primarily broken down by an enzyme called histaminase. This enzyme is naturally present in the body and converts histamine into inactive metabolites that are then easily eliminated through the kidneys and urine. Factors like your diet, gut health, and overall health can influence the activity of histaminase. Therefore, while water itself doesn't directly remove histamine, adequate hydration supports kidney function, which is essential for the elimination of the histamine metabolites produced after the breakdown of histamine by histaminase. This means that staying hydrated is indirectly beneficial for histamine management.
The Role of Hydration in Histamine Management
Proper hydration is vital for overall health and contributes to efficient bodily functions. When you're well-hydrated, your kidneys can function optimally, filtering waste products, including the byproducts of histamine metabolism. Dehydration, on the other hand, can impair kidney function, potentially slowing down the elimination process. Therefore, adequate hydration supports the natural processes that clear histamine metabolites from the body. It doesn't remove histamine itself, but it supports the systems that do.
Dietary Factors Affecting Histamine Levels
Your diet significantly impacts histamine levels. High-histamine foods can trigger histamine release and exacerbate symptoms in individuals sensitive to it. These foods include fermented products, aged cheeses, cured meats, and certain fish. A diet low in histamine can help manage symptoms in those with histamine intolerance. Hydration plays a supporting role here, as efficient kidney function, supported by adequate water intake, helps remove histamine metabolites more effectively, regardless of dietary histamine intake. This doesn't remove histamine, just the aftereffects.
The Importance of Gut Health and Histamine
The gut microbiome plays a crucial role in histamine metabolism. A healthy gut microbiome with diverse bacterial populations helps regulate histamine production and breakdown. Probiotics, prebiotics, and a balanced diet all support a healthy gut. While water itself doesn't directly influence the gut microbiome, adequate hydration is crucial for overall gut function. A well-hydrated body ensures optimal gut motility and nutrient absorption, thus indirectly supporting a healthy gut microbiome that contributes to better histamine management.
| Factor | Effect on Histamine | Role of Water |
|---|---|---|
| Histaminase Enzyme | Breaks down histamine into metabolites | Water supports kidney function to eliminate metabolites |
| Kidney Function | Filters and eliminates histamine metabolites | Adequate hydration is essential for optimal kidney function |
| Gut Microbiome | Influences histamine production and breakdown | Hydration supports overall gut health |
| Diet | High-histamine foods increase histamine levels | Water helps eliminate histamine metabolites from high-histamine food consumption |
Does drinking water help get rid of histamine?
The relationship between water intake and histamine levels is complex and not fully understood. While drinking water itself doesn't directly break down or eliminate histamine from the body, it plays a crucial role in several processes that indirectly influence histamine levels. Adequate hydration supports the body's natural detoxification processes, including the efficient functioning of the kidneys and liver, which are involved in removing waste products, including some histamine metabolites. However, it's important to note that water alone isn't a treatment for histamine intolerance or allergies. Other factors like diet and medication play a much larger role.
How the Body Processes Histamine
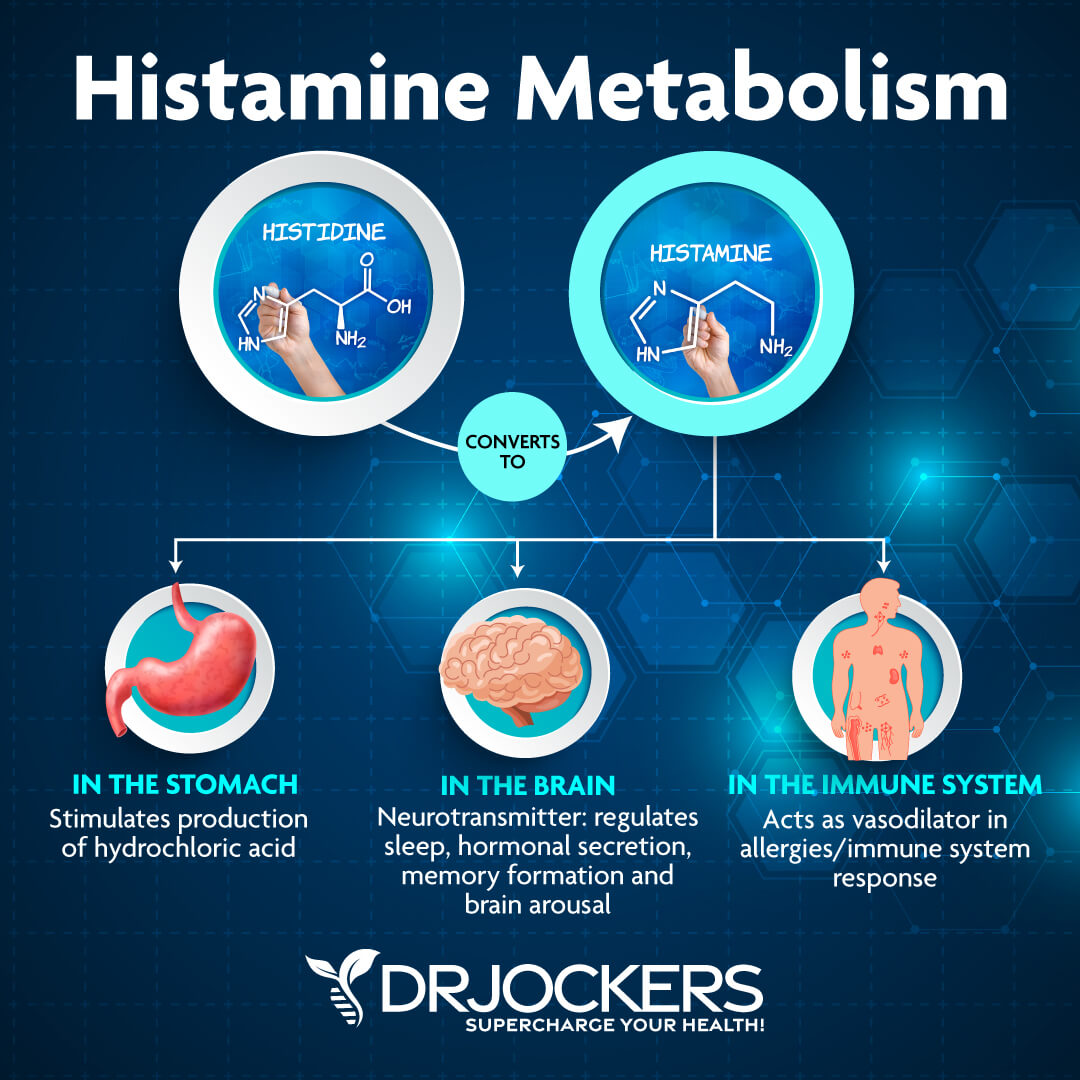
Histamine is a crucial molecule in the body with various functions, including immune response and digestion. After serving its purpose, it needs to be broken down and excreted. This process involves enzymes like diamine oxidase (DAO) and histamine methyltransferase (HNMT). Sufficient water intake contributes to overall bodily function, including the processes that involve these enzymes. However, water doesn't directly impact the enzyme activity itself.
- Enzyme activity: DAO and HNMT are crucial for histamine breakdown.
- Kidney function: Kidneys play a role in filtering and eliminating histamine metabolites.
- Liver function: The liver is involved in metabolizing histamine.
Water's Role in Detoxification
The body's detoxification pathways rely heavily on efficient fluid balance. Water helps flush out waste products, including some metabolites of histamine, through urine. This contributes to reducing the overall burden of these compounds. While this is an indirect effect, it's still a beneficial aspect of staying properly hydrated.
- Improved kidney filtration: Sufficient hydration enhances the kidneys' ability to filter waste.
- Enhanced liver function: Proper hydration supports optimal liver function in metabolic processes.
- Reduced waste buildup: Efficient elimination minimizes potential histamine metabolite buildup.
Histamine Intolerance and Hydration
Individuals with histamine intolerance often experience symptoms due to their body's inability to properly metabolize histamine. While water alone can't solve this underlying issue, adequate hydration is part of a holistic approach to managing the condition. Maintaining proper hydration can aid in overall health and support normal bodily functions, potentially mitigating some symptoms associated with histamine intolerance. But it should not be considered a primary treatment strategy.
- Symptom management: Hydration may help alleviate some symptoms related to histamine buildup.
- Supporting overall health: Good hydration helps maintain optimal body function.
- Part of a comprehensive approach: Hydration is only one piece of managing histamine intolerance.
The Importance of a Balanced Diet
Dietary factors heavily influence histamine levels. Consuming foods high in histamine or those that inhibit DAO can worsen symptoms for individuals sensitive to histamine. While hydration supports overall body function, focusing on a low-histamine diet is far more impactful in managing histamine levels than simply increasing water intake. Therefore, diet plays a critical role that shouldn't be overlooked.
- Low-histamine diet: Limiting foods high in histamine is key to managing symptoms.
- DAO-inhibiting foods: Avoiding foods that block DAO activity is crucial.
- Balanced nutrition: A well-rounded diet supports overall health and the body's ability to process histamine.
Other Factors Affecting Histamine Levels
Many factors beyond hydration and diet can influence histamine levels. These include stress, medications, gut health, and underlying medical conditions. Addressing these factors is essential for comprehensive histamine management. Relying solely on increased water intake to control histamine levels is unlikely to be effective.
- Stress management: Stress can impact histamine release.
- Medication interactions: Certain medications can affect histamine metabolism.
- Gut microbiome: Gut health plays a significant role in histamine production and breakdown.
How do you flush out histamines from your body?
There's no single, quick way to "flush out" histamines from your body. Histamine is a vital neurotransmitter and part of the body's natural immune response. The body naturally breaks down and eliminates histamines. However, when the body releases excessive histamine (e.g., during an allergic reaction), managing the symptoms and supporting the body's natural processes becomes crucial. This involves addressing the underlying cause of the histamine release and employing strategies to mitigate its effects. It's important to understand that actively removing histamine is not the goal; rather, the focus is on reducing its effects and supporting your body's ability to regulate it.
Dietary Changes to Reduce Histamine Levels
Modifying your diet can significantly impact histamine levels. Avoiding high-histamine foods is key. This isn't about removing histamine entirely, but reducing the intake of foods that can trigger excessive histamine release or inhibit its breakdown. Consuming foods rich in antioxidants can also help support your body's natural detoxification processes. Finally, introducing foods that support the gut microbiome is essential as a healthy gut plays a significant role in immune function and histamine regulation.
- Avoid high-histamine foods: Fermented foods (e.g., aged cheeses, sauerkraut, kimchi), cured meats, spinach, tomatoes, avocados, chocolate, alcohol.
- Consume antioxidant-rich foods: Berries, leafy greens, citrus fruits, artichokes.
- Support gut health: Consume prebiotic and probiotic-rich foods like yogurt, kefir, and asparagus.
Hydration and Detoxification Support
Staying properly hydrated is crucial for overall health and supporting your body's natural detoxification processes. Water helps flush out toxins, including metabolic byproducts. While not directly removing histamine, proper hydration assists in the overall process of eliminating waste products from the body. Consider incorporating natural diuretics like watermelon and dandelion tea (always consult with a healthcare professional before introducing new diuretics to your diet) to gently support fluid balance.
- Drink plenty of water: Aim for at least 8 glasses a day.
- Consider natural diuretics: Watermelon and dandelion tea can help with fluid balance, but consult a doctor before use.
- Avoid caffeine and alcohol: These can dehydrate you and exacerbate histamine issues.
Managing Allergic Reactions and Triggers
Identifying and avoiding allergens is paramount. Accurate allergen identification is best achieved through allergy testing. Once identified, diligently avoiding these allergens prevents future histamine release. This is a crucial preventative measure rather than a "flush-out" method. For immediate relief during an allergic reaction, antihistamines (taken as directed by a doctor) can block the effects of histamine.
- Allergy testing: Identify specific allergens through proper testing.
- Allergen avoidance: Strictly avoid identified allergens.
- Antihistamine medication: Use antihistamines as directed by a healthcare professional for immediate relief.
Supplements for Histamine Intolerance
Certain supplements may offer support for individuals with histamine intolerance, but they should always be used under the guidance of a healthcare professional. Some supplements that have shown potential in managing symptoms are DAO (diamine oxidase) supplements, which aid in histamine breakdown, and quercetin, a natural antihistamine. However, these supplements are not a substitute for medical advice or treatment, and potential interactions with other medications must be considered.
- DAO supplements: Support histamine breakdown (consult a doctor before use).
- Quercetin: Acts as a natural antihistamine (consult a doctor before use).
- Consult a healthcare professional: Never self-medicate; seek professional guidance before starting any new supplement.
Lifestyle Modifications for Histamine Regulation
Stress management techniques are vital as stress can exacerbate histamine release. Practicing relaxation techniques like yoga, meditation, or deep breathing exercises can help regulate the body's stress response. Adequate sleep is also crucial for overall health and immune function, further influencing histamine regulation. Finally, maintaining a healthy lifestyle with regular exercise also aids overall well-being.
- Stress reduction: Practice yoga, meditation, or deep breathing.
- Prioritize sleep: Aim for 7-9 hours of quality sleep per night.
- Regular exercise: Engage in regular physical activity.
Does histamine dissolve in water?

Histamine's solubility in water is complex and depends heavily on the pH of the solution. Histamine is a weak base, meaning it can accept a proton (H+). In aqueous solutions, histamine exists in equilibrium between its protonated (charged) form and its unprotonated (neutral) form. The proportion of each form depends on the pH relative to histamine's pKa (approximately 5.8). At physiological pH (around 7.4), a significant portion of histamine exists in its charged, water-soluble form. However, at lower pH values (more acidic), a larger proportion will exist in the uncharged form, which is less soluble in water. Therefore, while it is generally considered soluble in water, its solubility isn't absolute and is greatly influenced by the solution's acidity.
Histamine's Chemical Structure and Polarity
Histamine's structure contributes significantly to its solubility. It possesses several polar functional groups, including an amino group (-NH2) and an imidazole ring. These polar groups can form hydrogen bonds with water molecules, facilitating dissolution. However, the imidazole ring can also exist in different protonation states, influencing its overall polarity and, hence, solubility. The presence of a nonpolar aliphatic side chain influences hydrophobicity and interactions with lipids, further complicating the behavior of histamine in aqueous solutions.
- Polar functional groups enhance water solubility through hydrogen bonding.
- Imidazole ring protonation state influences polarity and solubility.
- Aliphatic side chain introduces some hydrophobicity.
The Effect of pH on Histamine Solubility
The pH of the aqueous solution plays a crucial role in determining histamine's solubility. At low pH (acidic conditions), the amino group becomes protonated, reducing the overall polarity and hence the solubility in water. Conversely, at high pH (alkaline conditions), the imidazole ring becomes deprotonated, increasing the overall polarity which is conducive to increased solubility. The pKa of histamine's imidazole ring is crucial, representing the pH where half of the histamine molecules are protonated and half are unprotonated. At pH values above the pKa, solubility increases significantly.
- Acidic conditions (low pH) decrease solubility.
- Alkaline conditions (high pH) increase solubility.
- pKa of imidazole ring (approx. 5.8) is the key point of transition.
Factors Affecting Histamine Solubility Beyond pH
Besides pH, other factors can subtly influence histamine's solubility. The presence of other ions or molecules in the solution can impact solubility through various interactions (e.g., ion pairing, complex formation). Temperature also affects solubility; generally, increasing temperature tends to increase solubility for many substances, including potentially histamine, though the effect might be minor. The concentration of histamine itself plays a role; at higher concentrations, solubility might decrease due to saturation effects, which is a common phenomenon.
- Presence of other ions or molecules can affect solubility.
- Temperature generally increases solubility (though the effect may be subtle).
- Concentration of histamine can limit solubility at higher levels.
Solubility in Different Solvents
While water is the most relevant solvent considering physiological contexts, histamine's solubility in other solvents is also relevant for analytical or pharmaceutical purposes. Histamine is less soluble in nonpolar solvents (e.g., organic solvents like hexane or chloroform) because of the hydrophobic interactions. However, it might exhibit higher solubility in polar aprotic solvents (e.g., DMSO), which can solvate polar molecules effectively without participating in extensive hydrogen bonding. Solubility in different solvents is determined by the balance between solute-solvent interactions and internal interactions within the histamine molecule itself.
- Low solubility in nonpolar solvents due to lack of favorable interactions.
- Higher solubility in polar aprotic solvents due to effective solvation.
- Solubility depends on the balance of interactions between solute and solvent.
Applications and Relevance of Histamine Solubility
Understanding histamine's solubility in water and other solvents is critical in various contexts. In pharmacology and drug delivery, its solubility dictates bioavailability and formulation strategies. In analytical chemistry, its solubility influences extraction, separation, and quantification methods. In food science and technology, its solubility is related to food preservation and stability. The knowledge of histamine solubility guides effective storage and handling of histamine-containing substances in various applications, from medicine to food products.
- Pharmacology: Solubility dictates bioavailability and drug formulation.
- Analytical chemistry: Solubility influences extraction and quantification.
- Food science: Solubility impacts food preservation and stability.
Does dehydration increase histamine?
Does Dehydration Increase Histamine?
The relationship between dehydration and histamine levels is complex and not fully understood. While there isn't a direct, causal link definitively proven, evidence suggests dehydration can indirectly influence histamine levels and related symptoms. Dehydration leads to a thicker, more concentrated blood volume. This can impact the body's ability to effectively clear out histamine and other inflammatory mediators from the system. Additionally, dehydration can exacerbate existing inflammatory conditions, potentially leading to increased histamine release. However, it's important to note that dehydration itself doesn't directly causethe body to produce more histamine. The effect is more about altered clearance and potentially triggering pre-existing inflammatory responses.
Mechanisms of Dehydration's Indirect Effect on Histamine
Dehydration's impact on histamine is largely indirect, influencing factors that modulate histamine levels rather than directly stimulating its production. Reduced blood volume and increased blood viscosity, hallmarks of dehydration, can impede the efficient circulation and clearance of histamine. This impaired clearance may lead to a relative increase in histamine levels, resulting in enhanced allergic symptoms. Furthermore, dehydration can stress the body, activating the sympathetic nervous system and potentially triggering the release of other inflammatory mediators that indirectly affect histamine activity.
- Impaired histamine clearance: Dehydration thickens blood, hindering the efficient removal of histamine.
- Increased blood viscosity: Slows circulation, preventing rapid dispersal of histamine.
- Stress response activation: Dehydration can trigger stress responses that may indirectly influence histamine.
Dehydration and Mast Cell Activation
Mast cells are key players in the immune system, responsible for releasing histamine in response to allergens or injury. While dehydration doesn't directly activate mast cells, indirect effects may play a role. For instance, if dehydration contributes to an inflammatory state, it may create a more sensitive environment making mast cells more likely to respond to even minor stimuli. Consequently, even a normal level of allergen exposure might trigger a stronger histamine response in a dehydrated individual. This, however, is still under investigation, lacking comprehensive research directly linking dehydration to significant mast cell degranulation.
- Increased inflammatory state: Dehydration might sensitize the body, making mast cells more reactive.
- Indirect activation: Dehydration's inflammatory effect can create a more receptive environment for mast cell activation.
- Limited direct evidence: Research directly linking dehydration to significant mast cell degranulation is sparse.
Dehydration and Allergic Reactions
Individuals prone to allergies often experience worsened symptoms when dehydrated. This is likely not due to a direct increase in histamine production by dehydration itself, but rather an impaired ability to regulate the inflammatory response. The already heightened inflammatory state associated with allergies becomes exacerbated by dehydration, potentially leading to more pronounced symptoms like itching, sneezing, and congestion. This is because the body's mechanisms for clearing histamine become less effective under conditions of dehydration.
- Exacerbated allergic symptoms: Dehydration worsens symptoms in individuals with allergies.
- Impaired inflammatory response regulation: Dehydration hinders the body’s ability to control inflammation.
- Reduced histamine clearance: Dehydration slows the body's ability to clear histamine from the system.
Dehydration and Histamine Intolerance
Histamine intolerance is a condition where individuals have difficulty metabolizing histamine, leading to symptoms similar to allergies, even without exposure to allergens. Dehydration can exacerbate symptoms in people with histamine intolerance as the already compromised histamine metabolism becomes even less efficient in a dehydrated state. The slower clearance of histamine due to reduced blood flow and increased blood viscosity contributes to a build-up of histamine, worsening existing symptoms. More research is needed to solidify this link.
- Impaired histamine metabolism: Dehydration might hinder the already impaired histamine metabolism in affected individuals.
- Symptom exacerbation: Dehydration can worsen symptoms in individuals with histamine intolerance.
- Further research needed: More studies are needed to understand the exact nature of this relationship.
Does drinking water help flush out histamine?
While drinking plenty of water is generally good for your health and overall body function, it doesn't directly "flush out" histamine in the way some people might think. Histamine isn't a toxin that needs to be actively removed from the body like a foreign substance. It's a chemical messenger naturally produced by your body and plays crucial roles in various bodily functions, including immune responses, digestion, and nerve transmission. When your body releases histamine in response to an allergen or irritant (like a food intolerance), it triggers the symptoms associated with allergic reactions, such as sneezing, itching, and inflammation. Drinking water helps to maintain hydration, which is important for overall health, but it doesn't specifically target or eliminate histamine. In fact, excessive water intake might not significantly alter histamine levels and could even dilute other essential electrolytes. The best way to manage histamine-related issues is to address the underlying cause, whether it's food allergies, environmental triggers, or other medical conditions. This might involve working with an allergist or other healthcare professional to develop an appropriate management plan that could include dietary changes, medication, or other therapies. So, while hydration is essential, it's not a primary method for reducing histamine levels.
Can water help reduce histamine symptoms?
While water itself doesn't directly remove histamine, adequate hydration can indirectly help mitigate some histamine-related symptoms. Dehydration can worsen symptoms like headaches, fatigue, and digestive issues, which are often associated with histamine release. By staying properly hydrated, you can support your body's overall function and potentially lessen the severity of some symptoms. For example, maintaining optimal hydration helps your kidneys function efficiently, which in turn can improve the body's natural process of eliminating waste products. However, it's important to remember that this is an indirect effect, and water won't resolve the underlying cause of the histamine release. If you're experiencing significant histamine-related symptoms, you should consult a healthcare professional for a proper diagnosis and treatment plan. This plan might involve antihistamines, avoidance of histamine-rich foods, or other strategies depending on the cause and severity of your condition. Focusing solely on water intake might not be sufficient to manage severe allergic reactions or other histamine-related problems.
Does flushing out the system with water affect histamine levels?
The concept of "flushing out your system" is often misunderstood. Your body has sophisticated mechanisms for managing substances like histamine. While your kidneys and liver play crucial roles in filtering and eliminating various waste products and toxins, they don't primarily work to reduce histamine levels in a way that's significantly influenced by water intake. Drinking more water will help maintain hydration and support your body's overall functioning, but it won't dramatically alter the production or breakdown of histamine itself. Histamine production and breakdown are regulated by complex enzymatic processes within the body, and these are largely independent of simple water consumption. If you're concerned about high histamine levels, consult a healthcare professional. They can help determine if you have a condition causing excessive histamine release or if you're experiencing symptoms unrelated to histamine. They can then guide you toward appropriate tests and treatment strategies rather than relying on unproven methods like simply increasing water intake.
What are better ways to manage histamine than drinking more water?
While staying hydrated is important for overall health, there are far more effective strategies for managing histamine levels and symptoms than just increasing water intake. The most important step is to identify and address the underlying cause of elevated histamine or histamine-related symptoms. This could involve identifying and avoiding allergens or trigger foods high in histamine, consulting an allergist or immunologist for testing and diagnosis, and potentially taking medication like antihistamines to block histamine receptors and reduce symptoms. In some cases, a specialized diet low in histamine may be recommended. This diet often requires careful planning and may involve restricting certain foods. Furthermore, managing stress levels is crucial, as stress can exacerbate histamine release. Techniques like meditation, yoga, or other stress-reducing practices can be beneficial. A comprehensive approach that includes identifying the root cause, dietary changes, medication if needed, and stress management techniques is much more effective than relying solely on increasing water consumption.

Deja una respuesta