Can allergies damage your lungs

Allergies are a common problem that can cause a variety of symptoms, from sneezing and a runny nose to itchy eyes and skin. In some cases, allergies can also affect the lungs, causing wheezing, coughing, and shortness of breath. While allergies are not typically life-threatening, they can be a significant source of discomfort and can lead to other health problems.
Can Allergies Damage Your Lungs?
Allergies, while often inconvenient and uncomfortable, don't typically cause permanent lung damage in the way a chronic lung disease like COPD or cystic fibrosis might. However, they can significantly impact lung health and function, leading to various issues that, if left unmanaged, could have long-term consequences. The severity of the impact depends largely on the type of allergy, the individual's sensitivity, and the frequency and intensity of exposure to allergens. Untreated allergies can exacerbate underlying lung conditions and even increase the risk of developing respiratory problems.
Asthma and Allergies: A Close Relationship
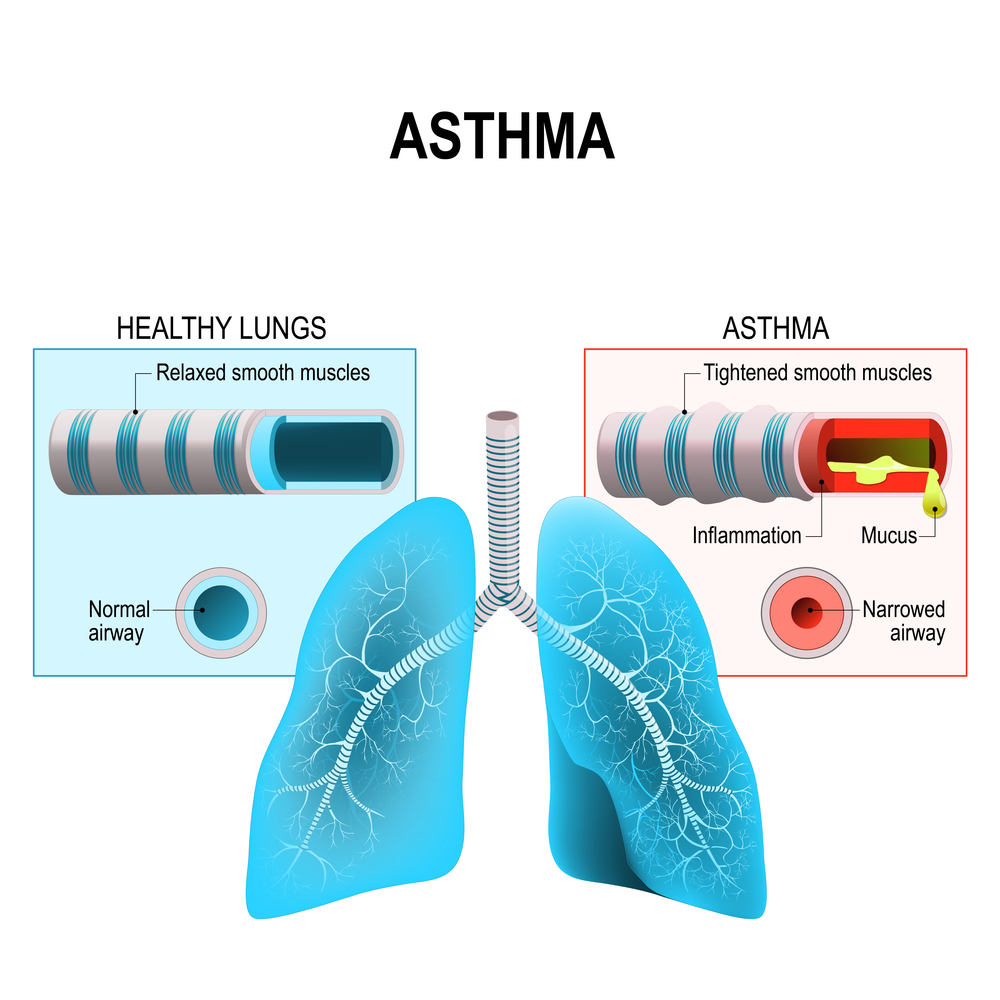
Many people with allergies also suffer from asthma. Allergies are a major trigger for asthma attacks. When allergens like pollen, dust mites, or pet dander are inhaled, they can trigger an inflammatory response in the airways. This inflammation leads to bronchoconstriction (narrowing of the airways), increased mucus production, and coughing, wheezing, and shortness of breath – the hallmarks of an asthma attack. Chronic inflammation from allergic asthma can, over time, lead to airway remodeling, making the airways permanently narrower and more susceptible to further attacks. This isn't necessarily "damage" in the sense of scarring, but it is a significant alteration in lung structure and function.
Allergic Rhinitis and its Lung Implications
Allergic rhinitis (hay fever) primarily affects the nose, causing symptoms like sneezing, runny nose, and congestion. However, it can also impact the lungs. The inflammation associated with allergic rhinitis can extend to the lower airways, contributing to cough, wheezing, and shortness of breath. While not directly causing lung damage, the chronic inflammation can increase susceptibility to respiratory infections and worsen existing lung conditions like asthma.
Sinusitis and its Connection to Lung Health
Allergic sinusitis, an inflammation of the sinuses caused by an allergic reaction, can also have ramifications for lung health. The inflammation and infection can sometimes spread to the lower respiratory tract, leading to bronchitis or pneumonia. Chronic sinusitis can contribute to persistent cough and shortness of breath, affecting lung function and potentially increasing the risk of more severe respiratory illnesses.
Lung Infections and Allergic Responses
People with allergies may be more prone to lung infections. The inflammation caused by allergies can weaken the immune system's ability to fight off bacteria and viruses. This increased susceptibility means that individuals with allergies might experience more frequent or severe respiratory infections, such as bronchitis and pneumonia. These infections, in turn, can further irritate and inflame the lungs.
The Role of Allergic Pneumonitis
In rare cases, allergies can lead to a more serious condition called allergic pneumonitis (hypersensitivity pneumonitis). This occurs when the immune system overreacts to inhaled allergens, causing inflammation and damage to the alveoli (the tiny air sacs in the lungs). Allergic pneumonitis can cause a range of symptoms, from mild cough and shortness of breath to severe respiratory distress and even permanent lung damage. This condition is less common than other allergy-related lung issues but highlights the potential for significant impact in severe cases.
| Allergic Condition | Impact on Lungs | Potential Long-Term Effects |
|---|---|---|
| Asthma | Airway inflammation and bronchoconstriction | Airway remodeling, increased susceptibility to attacks |
| Allergic Rhinitis | Inflammation extending to lower airways | Increased susceptibility to respiratory infections |
| Allergic Sinusitis | Potential spread of infection to lungs | Chronic cough and shortness of breath |
| Allergic Pneumonitis | Inflammation and damage to alveoli | Severe respiratory distress, potential permanent lung damage |
Can Allergies Damage Your Lungs?
Allergies, while often inconvenient and uncomfortable, don't typically cause permanent lung damage in the way a chronic lung disease like COPD or cystic fibrosis might. However, they can significantly impact lung health and function, leading to various issues that, if left unmanaged, could have long-term consequences. The severity of the impact depends largely on the type of allergy, the individual's sensitivity, and the frequency and intensity of exposure to allergens. Untreated allergies can exacerbate underlying lung conditions and even increase the risk of developing respiratory problems.
Asthma and Allergies: A Close Relationship
Many people with allergies also suffer from asthma. Allergies are a major trigger for asthma attacks. When allergens like pollen, dust mites, or pet dander are inhaled, they can trigger an inflammatory response in the airways. This inflammation leads to bronchoconstriction (narrowing of the airways), increased mucus production, and coughing, wheezing, and shortness of breath – the hallmarks of an asthma attack. Chronic inflammation from allergic asthma can, over time, lead to airway remodeling, making the airways permanently narrower and more susceptible to further attacks. This isn't necessarily "damage" in the sense of scarring, but it is a significant alteration in lung structure and function.
Allergic Rhinitis and its Lung Implications
Allergic rhinitis (hay fever) primarily affects the nose, causing symptoms like sneezing, runny nose, and congestion. However, it can also impact the lungs. The inflammation associated with allergic rhinitis can extend to the lower airways, contributing to cough, wheezing, and shortness of breath. While not directly causing lung damage, the chronic inflammation can increase susceptibility to respiratory infections and worsen existing lung conditions like asthma.
Sinusitis and its Connection to Lung Health
Allergic sinusitis, an inflammation of the sinuses caused by an allergic reaction, can also have ramifications for lung health. The inflammation and infection can sometimes spread to the lower respiratory tract, leading to bronchitis or pneumonia. Chronic sinusitis can contribute to persistent cough and shortness of breath, affecting lung function and potentially increasing the risk of more severe respiratory illnesses.
Lung Infections and Allergic Responses
People with allergies may be more prone to lung infections. The inflammation caused by allergies can weaken the immune system's ability to fight off bacteria and viruses. This increased susceptibility means that individuals with allergies might experience more frequent or severe respiratory infections, such as bronchitis and pneumonia. These infections, in turn, can further irritate and inflame the lungs.
The Role of Allergic Pneumonitis
In rare cases, allergies can lead to a more serious condition called allergic pneumonitis (hypersensitivity pneumonitis). This occurs when the immune system overreacts to inhaled allergens, causing inflammation and damage to the alveoli (the tiny air sacs in the lungs). Allergic pneumonitis can cause a range of symptoms, from mild cough and shortness of breath to severe respiratory distress and even permanent lung damage. This condition is less common than other allergy-related lung issues but highlights the potential for significant impact in severe cases.
| Allergic Condition | Impact on Lungs | Potential Long-Term Effects |
|---|---|---|
| Asthma | Airway inflammation and bronchoconstriction | Airway remodeling, increased susceptibility to attacks |
| Allergic Rhinitis | Inflammation extending to lower airways | Increased susceptibility to respiratory infections |
| Allergic Sinusitis | Potential spread of infection to lungs | Chronic cough and shortness of breath |
| Allergic Pneumonitis | Inflammation and damage to alveoli | Severe respiratory distress, potential permanent lung damage |
What are the symptoms of pulmonary allergies?
:max_bytes(150000):strip_icc()/respiratory-allergies-symptoms-causes-and-treatment-5206183-5205177-final-7af9eb5916eb4a8dacf8b9bd516cad85.jpg)
Pulmonary allergies, also known as allergic lung diseases, encompass a range of conditions where the lungs react adversely to inhaled allergens. Symptoms vary depending on the specific allergy and its severity, but generally involve the airways and lungs' inflammatory response. Common symptoms can manifest in the respiratory system, but also impact other parts of the body due to the interconnectedness of the immune system.
Cough
A cough is a very common symptom of pulmonary allergies. It can range from a mild, occasional cough to a persistent, severe cough that disrupts sleep and daily activities. The cough is often dry, meaning it doesn't produce much phlegm, but it can become productive (producing phlegm) in more severe cases. The cough is triggered by the body's attempt to clear the airways of irritants. The severity and type of cough can vary greatly depending on the allergen and individual response.
- Dry, hacking cough: Characterized by a repetitive, often irritating cough without mucus production.
- Productive cough: Produces phlegm, which may be clear, white, yellow, or even green depending on the stage of the inflammation.
- Wheezing cough: Associated with airway narrowing, producing a whistling sound during exhalation.
Wheezing
Wheezing is a high-pitched whistling sound during breathing, typically heard on exhalation. It's caused by the narrowing of the airways in the lungs due to inflammation and bronchospasm. Wheezing is a hallmark sign of asthma, a common pulmonary allergy. It indicates that the air passages are constricted, making it difficult to breathe. The intensity of wheezing can vary depending on the severity of the allergic reaction.
- Severity: Wheezing can range from a mild, intermittent sound to a severe, constant sound that significantly impacts breathing.
- Timing: It might occur only during an allergic reaction or be present constantly.
- Associated Symptoms: Wheezing often accompanies other symptoms, such as coughing, shortness of breath, and chest tightness.
Shortness of Breath (Dyspnea)
Shortness of breath, or dyspnea, is a feeling of not getting enough air. This is a crucial symptom indicating that the lungs are not functioning efficiently. In pulmonary allergies, shortness of breath can result from airway inflammation and narrowing, reducing the amount of air that can enter and leave the lungs. The intensity of shortness of breath can range from mild difficulty catching one's breath to severe breathlessness, even at rest. It can be triggered by exertion or exposure to allergens.
- Exercise-induced dyspnea: Shortness of breath that occurs only during physical activity.
- Resting dyspnea: Shortness of breath that occurs even when resting.
- Paroxysmal nocturnal dyspnea: Sudden shortness of breath at night that awakens the individual.
Chest Tightness
A feeling of tightness or pressure in the chest is a common symptom associated with pulmonary allergies, especially asthma. This sensation is caused by the constriction of the airways and inflammation of the lung tissues. Chest tightness often accompanies shortness of breath and wheezing, and it can vary in severity from a mild discomfort to a feeling of intense pressure and suffocation. It can be triggered by exposure to allergens, respiratory infections or physical activity.
- Intensity: Can range from a mild feeling of pressure to a severe, constricting feeling.
- Location: Usually felt in the center of the chest, but can sometimes radiate to other areas.
- Associated symptoms: Often accompanied by wheezing, coughing, and shortness of breath.
Sneezing and Runny Nose
While primarily associated with upper respiratory allergies like hay fever, sneezing and a runny nose can also be present in pulmonary allergies, especially if the allergens are also affecting the upper airways. This is because the inflammatory response isn't always limited to the lower respiratory tract (lungs). These symptoms indicate an immune response to inhaled allergens and may precede or accompany other pulmonary allergy symptoms. The severity can vary widely.
- Frequency: Sneezing can range from occasional sneezes to frequent bouts.
- Mucus Production: Runny nose produces clear, watery mucus, sometimes turning thicker and more colored in later stages of inflammation.
- Itchiness: The nose and throat may also feel itchy.
What are the symptoms of long term allergies?
What are the symptoms of long-term allergies?
Long-term allergies, also known as chronic allergies, can manifest in a wide variety of symptoms, depending on the allergen and the individual's sensitivity. Symptoms can range from mild to severe and may impact multiple body systems. Unlike acute allergic reactions which are immediate, chronic allergies often present with persistent or recurring symptoms that can significantly affect quality of life. The persistence of these symptoms often leads to complications if left unmanaged. It's crucial to consult an allergist for proper diagnosis and management of chronic allergies.
Persistent Respiratory Symptoms
Chronic allergies frequently trigger persistent respiratory issues. These are often characterized by ongoing inflammation in the airways, leading to a range of uncomfortable and potentially debilitating symptoms. The severity and specific symptoms can vary greatly depending on the individual and the specific allergen.
- Persistent coughing: A dry, hacking cough that may be worse at night or early morning.
- Wheezing: A whistling sound during breathing, indicating airway narrowing.
- Shortness of breath: Difficulty breathing, even during rest or mild exertion.
- Chest tightness: A feeling of constriction or pressure in the chest.
- Sinusitis: Inflammation of the sinuses leading to facial pain, pressure, and congestion.
Chronic Skin Manifestations
Long-term allergic reactions can significantly impact the skin. The resulting skin conditions can be itchy, unsightly, and sometimes painful. These conditions can be persistent and challenging to manage, requiring ongoing treatment and careful attention to triggers.
- Eczema (Atopic Dermatitis): Characterized by itchy, inflamed, and often cracked skin.
- Hives (Urticaria): Raised, itchy welts that can appear anywhere on the body.
- Contact Dermatitis: Inflammation of the skin caused by direct contact with an allergen.
- Persistent Itching: General itching that is not easily relieved.
- Dry, Scaly Skin: Chronic dryness and scaling, especially in affected areas.
Eye Irritation and Discomfort
Allergic conjunctivitis, a common manifestation of long-term allergies, affects the eyes. The eyes become irritated and inflamed, often accompanied by other uncomfortable symptoms. These symptoms can impact daily activities and significantly reduce quality of life if left untreated.
- Itchy, watery eyes: Persistent itching and excessive tearing.
- Red, swollen eyelids: Inflammation and swelling of the eyelids.
- Eyelid crusting: Build-up of secretions on the eyelids, especially upon waking.
- Blurred vision: Temporary blurring due to eye irritation and swelling.
- Light sensitivity (Photophobia): Increased sensitivity to light.
Digestive Issues
While less commonly associated with allergies than respiratory or skin symptoms, digestive problems can also be a hallmark of long-term allergic reactions. These can range from mild discomfort to severe gastrointestinal distress and can be difficult to diagnose and manage.
- Abdominal pain: Persistent or recurring abdominal pain.
- Diarrhea: Loose or watery stools.
- Nausea and vomiting: Feelings of sickness and the urge to vomit.
- Bloating and gas: Abdominal distension and gas.
- Food allergies: Persistent digestive issues triggered by specific foods.
Fatigue and General Malaise
Chronic allergies often result in persistent fatigue and a general feeling of unwellness. This fatigue is not simply tiredness; it's often profound and debilitating, interfering with daily activities and impacting quality of life. The underlying inflammation and immune system response associated with long-term allergies contribute to this overall feeling of being unwell.
- Persistent fatigue: Extreme tiredness and lack of energy.
- Difficulty concentrating: Impaired focus and cognitive function.
- Headaches: Frequent or persistent headaches.
- Muscle aches and pains: Generalized muscle aches and discomfort.
- Reduced overall well-being: A persistent feeling of illness and discomfort.
How to clear allergies from lungs?
:max_bytes(150000):strip_icc()/respiratory-allergies-symptoms-causes-and-treatment-5206183-5205177-final-7af9eb5916eb4a8dacf8b9bd516cad85.jpg)
There's no way to completely "clear" allergies from your lungs. Allergies are an immune system response, and you can't simply eliminate that response. However, you can significantly reduce allergy symptoms and inflammation in your lungs. This involves managing your exposure to allergens and using treatments to control the symptoms. It's crucial to remember that if you suspect a serious lung issue related to allergies, like asthma, you should seek immediate medical attention. Self-treating can be dangerous.
Identify and Avoid Allergens
The first step to managing lung allergy symptoms is identifying your specific triggers. Common airborne allergens include pollen, dust mites, pet dander, and mold spores. Food allergies can also trigger respiratory symptoms. Once you know your triggers, actively avoid them. This involves things like:
- Regularly cleaning your home to reduce dust mites and other allergens. This includes vacuuming, dusting, and washing bedding in hot water.
- Using air purifiers with HEPA filters in your home, especially in bedrooms.
- Keeping pets out of bedrooms or regularly grooming them to minimize dander.
Medication for Allergy Relief
Various medications can help control allergy symptoms affecting your lungs. These often involve managing inflammation and reducing the immune response. Your doctor can help determine the best course of action based on your specific needs and medical history. Commonly prescribed medications include:
- Antihistamines to alleviate sneezing, itching, and runny nose.
- Decongestants to reduce nasal congestion.
- Corticosteroids (inhaled or oral) to reduce inflammation in the airways, particularly crucial for asthma sufferers.
- Leukotriene modifiers which block the effects of leukotrienes, inflammatory substances contributing to allergy symptoms.
Lifestyle Changes for Lung Health
Certain lifestyle adjustments can complement medical treatments and improve lung health. Maintaining a healthy lifestyle contributes to a stronger immune system, making you better equipped to handle allergy triggers. These changes include:
- Regular exercise to improve lung capacity and overall health.
- Quitting smoking, as smoking significantly worsens respiratory conditions and can interact negatively with allergy medication.
- Managing stress levels, as stress can exacerbate allergy symptoms.
- Eating a balanced diet rich in fruits and vegetables, supporting a healthy immune system.
Seek Professional Medical Advice
It's crucial to consult an allergist or doctor if you experience persistent or severe allergy symptoms affecting your lungs. They can conduct allergy testing to identify your specific triggers, assess your respiratory health, and recommend the most appropriate treatment plan. Don't hesitate to seek professional help, especially if you suspect you have asthma or other underlying respiratory conditions.
- Allergy testing can identify specific allergens causing your symptoms.
- Spirometry measures lung function to assess the severity of any lung impairment.
- Chest X-rays or other imaging tests might be necessary to rule out other lung problems.
Home Remedies and Natural Approaches
While home remedies and natural approaches may provide some relief for mild allergy symptoms, they shouldn't replace medical treatment, especially if your symptoms are severe or persistent. Some people find relief with techniques like:
- Nasal irrigation (using a neti pot) to rinse out allergens and irritants from the nasal passages.
- Steam inhalation to soothe irritated airways (but be cautious to avoid burns).
- Certain herbal remedies, although their effectiveness varies and they should be discussed with your doctor before use.
Can allergies affect my lungs?
Yes, allergies can significantly affect your lungs. Allergic reactions occur when your immune system mistakenly identifies a harmless substance (allergen) as a threat. This triggers the release of histamine and other chemicals that cause inflammation throughout the body, including in the lungs. The effects can range from mild irritation to severe, life-threatening conditions.
Allergic Asthma
Allergic asthma is a common lung condition triggered by allergens. When allergens like pollen, dust mites, or pet dander are inhaled, they inflame the airways, leading to symptoms like wheezing, coughing, shortness of breath, and chest tightness. The inflammation narrows the airways, making it difficult to breathe. This is a chronic condition requiring ongoing management.
- Symptoms: Wheezing, coughing, shortness of breath, chest tightness.
- Triggers: Pollen, dust mites, pet dander, mold, cockroaches.
- Treatment: Inhalers (corticosteroids, bronchodilators), allergy shots, avoidance of triggers.
Allergic Bronchitis
Allergic bronchitis is inflammation of the bronchi (large airways in the lungs) caused by an allergic reaction. Unlike asthma, it may not always involve airway narrowing, but it can still lead to a persistent cough, especially at night. This cough is often accompanied by mucus production. The inflammation is a key characteristic, and it can be triggered by various airborne allergens.
- Symptoms: Persistent cough (often worse at night), mucus production.
- Triggers: Similar to asthma: pollen, dust mites, pet dander, mold.
- Treatment: Cough suppressants, anti-inflammatory medications, allergy management.
Hypersensitivity Pneumonitis
Hypersensitivity pneumonitis (HP) is a more serious condition resulting from an allergic reaction in the lungs. It's often caused by inhaling organic dusts like mold spores, bird droppings, or animal proteins. The body's immune response leads to inflammation and damage to the tiny air sacs (alveoli) in the lungs. Symptoms can vary, from mild cough to severe shortness of breath and even lung failure in severe cases.
- Symptoms: Cough, shortness of breath, fever, fatigue.
- Triggers: Inhaled organic dusts (mold, bird droppings, animal proteins).
- Treatment: Corticosteroids, avoiding exposure to triggers, oxygen therapy in severe cases.
Allergic Rhinitis and its Lung Effects
While primarily affecting the nose (causing runny nose, sneezing, itchy eyes), allergic rhinitis can also contribute to lung problems. Postnasal drip from allergic rhinitis can irritate the lungs and airways, triggering coughing and wheezing, especially in those predisposed to asthma or other lung conditions. This irritation is often indirect, stemming from the nasal inflammation.
- Symptoms: Runny nose, sneezing, itchy eyes, postnasal drip, coughing, wheezing.
- Triggers: Pollen, dust mites, pet dander, mold.
- Treatment: Nasal corticosteroids, antihistamines, saline nasal sprays.
Anaphylaxis and its Lung Impact
Anaphylaxis is a severe, life-threatening allergic reaction. It can affect multiple systems, including the lungs, causing bronchospasm (severe constriction of the airways) and potentially leading to respiratory failure. This is a medical emergency requiring immediate treatment with epinephrine.
- Symptoms: Difficulty breathing, wheezing, swelling of the throat and tongue, hives, dizziness, rapid pulse.
- Triggers: Wide variety of allergens (e.g., peanuts, bee stings, medications).
- Treatment: Immediate injection of epinephrine, oxygen therapy, airway management.
Can allergies cause permanent lung damage?
While allergies themselves don't directly cause permanent lung damage in most cases, the inflammation they trigger can have long-term consequences if left unmanaged. The most significant risk lies in the development of allergic asthma. Asthma, triggered by allergic reactions, causes the airways to narrow and swell, leading to wheezing, coughing, and shortness of breath. If asthma is poorly controlled over many years, it can lead to irreversible changes in lung structure, including airway remodeling, which involves the thickening of airway walls and increased mucus production. This remodeling can result in persistent airflow limitation and reduced lung function, even when symptoms are controlled. However, with proper diagnosis, medication management, and avoidance of allergy triggers, the chances of developing severe, irreversible lung damage are significantly reduced. It’s crucial to note that the severity of the potential damage depends on several factors, including the severity and frequency of allergic reactions, the individual's response to treatment, and the presence of other underlying respiratory conditions. Early diagnosis and consistent treatment are essential for preventing long-term lung complications related to allergies.
Can food allergies damage my lungs?
Food allergies can indirectly affect your lungs, primarily through the reaction they trigger in the body. While a food allergy itself doesn't directly damage lung tissue, the systemic allergic reaction it can induce may involve the respiratory system. A severe allergic reaction, known as anaphylaxis, can cause a life-threatening constriction of the airways, leading to difficulty breathing, wheezing, and potentially even respiratory arrest. Though anaphylaxis is a relatively rare occurrence, it demonstrates the potential for severe respiratory complications. Additionally, some individuals might experience eosinophilic esophagitis (EoE), a condition where eosinophils (a type of white blood cell) infiltrate the esophagus. While primarily affecting the esophagus, EoE has been linked to other allergic conditions including asthma, which can indeed lead to lung damage over time. Therefore, managing food allergies effectively is vital not only to prevent immediate reactions but also to reduce the long-term risk of respiratory complications associated with allergies. Regular check-ups with an allergist and careful adherence to dietary restrictions are essential in minimizing potential lung complications from food allergies.
How do seasonal allergies affect my lungs?
Seasonal allergies, or hay fever, primarily affect the upper respiratory tract, causing symptoms like runny nose, sneezing, and itchy eyes. However, they can also significantly impact lung function. The inflammation caused by allergens like pollen can trigger or exacerbate underlying respiratory conditions such as asthma. Seasonal allergy symptoms, especially when severe or prolonged, lead to ongoing airway inflammation, which can increase the frequency and severity of asthma attacks. This constant inflammation, even if not causing immediate damage, can contribute to the airway remodeling process, potentially leading to irreversible changes in the lungs over time. Furthermore, the constant coughing and mucus production associated with seasonal allergies can irritate the lungs and airways, possibly contributing to long-term respiratory issues. Therefore, effectively managing seasonal allergies through medication, immunotherapy, or avoidance strategies is crucial to minimize their impact on lung health. Proper management can reduce the frequency and severity of exacerbations of asthma and other respiratory conditions, thereby limiting the potential for long-term lung damage.
Can dust mite allergies damage lungs?
Dust mite allergies, like other allergies, don’t directly cause permanent lung damage, but their effects can be significant, particularly in individuals with asthma or other respiratory sensitivities. Dust mites are tiny creatures that live in bedding, carpets, and upholstery. Their droppings and body parts contain allergens that trigger an immune response, leading to inflammation in the airways. This inflammation can exacerbate existing asthma, causing increased frequency and severity of attacks. The constant exposure to dust mite allergens and the resulting airway irritation can contribute to the development of airway hyperresponsiveness, making the airways more sensitive to irritants and triggers, further increasing the risk of asthma attacks and other respiratory problems. Prolonged exposure and uncontrolled inflammation can, in severe cases, contribute to the progression of lung disease over time. However, with effective allergy management, including strategies like dust mite control in the home (encasement of mattresses and pillows, regular cleaning), medication, and avoidance techniques, the risk of serious long-term lung damage can be mitigated. The key is proactive management of the allergy to minimize ongoing inflammation.

Deja una respuesta