Can allergies scar lungs

Can allergies scar lungs? This is a question that many people with allergies may wonder about. Allergies are a common problem, affecting millions of people worldwide. While most allergies are not serious, some can be more severe and even life-threatening. In some cases, allergies can even lead to scarring of the lungs.
Can Allergies Scar Your Lungs?
Allergies, while often inconvenient and uncomfortable, generally don't directly cause scarring in the lungs. However, severe and prolonged allergic reactions, as well as the underlying conditions sometimes associated with allergies, can have indirect effects that might lead to lung damage over time. It's crucial to understand that this is not a common outcome of typical allergic reactions like hay fever or mild food allergies. The link between allergies and lung scarring is complex and often involves other factors.
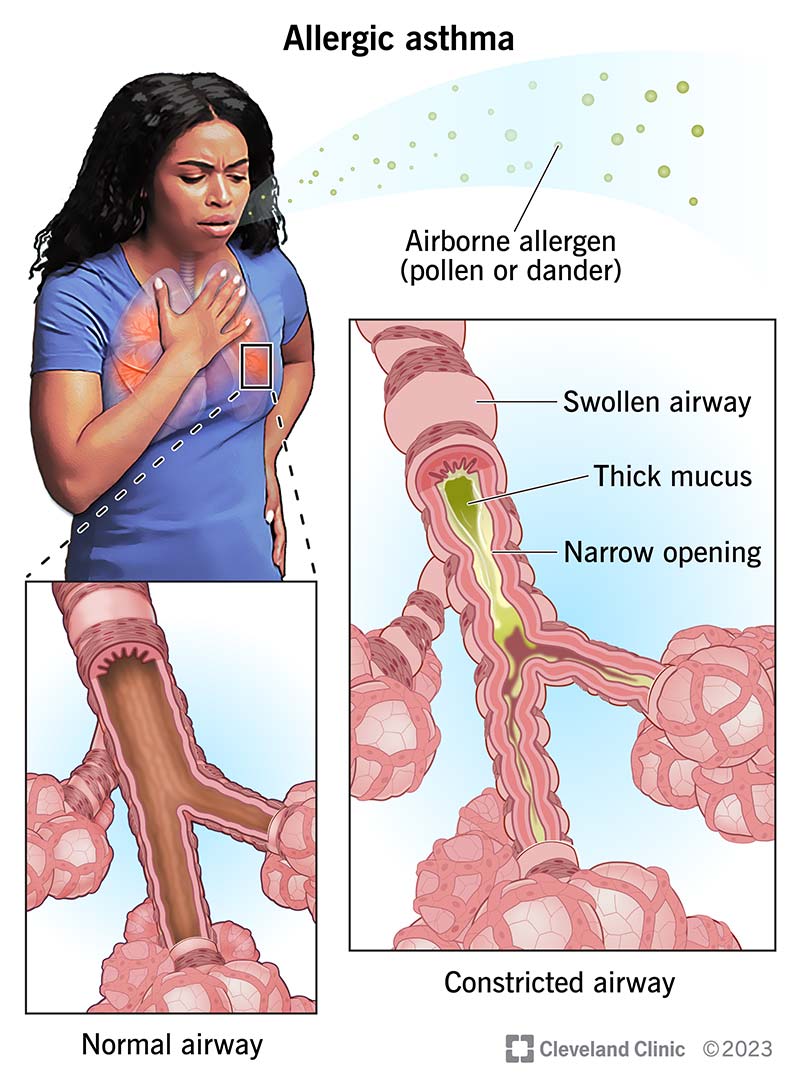
Allergic Asthma and Lung Damage
Allergic asthma is a common condition where an allergic reaction triggers inflammation and constriction of the airways. While asthma itself doesn't directly cause scarring (fibrosis), severe, uncontrolled asthma can lead to airway remodeling. This involves changes in the structure of the airways, including thickening of the walls and increased mucus production. Over many years, this remodeling can potentially contribute to irreversible lung damage, though it's not technically scarring in the same way a cut scars. The key here is the long-term, poorly managed inflammation.
Hypersensitivity Pneumonitis and Lung Scarring
Hypersensitivity pneumonitis (HP) is a rare but serious lung disease caused by an allergic reaction to inhaled substances like mold spores, bird droppings, or certain dusts. Unlike typical allergies, HP involves a more intense immune response that directly damages the lung tissue. This damage can lead to interstitial lung disease, a group of conditions that cause scarring and inflammation in the spaces between the air sacs in the lungs. HP is a severe condition that requires prompt diagnosis and treatment to prevent permanent lung damage.
Eosinophilic Granulomatosis with Polyangiitis (EGPA)
EGPA is a rare condition that affects the blood vessels and can also involve the lungs. It's considered a type of vasculitis, which is inflammation of the blood vessels. Although linked to allergies in some cases, EGPA's main issue is the inflammation in blood vessels, which can lead to the formation of granulomas (clusters of immune cells) and damage to lung tissue. This damage can result in scarring and other significant lung problems. It is important to emphasize that EGPA's relationship to allergies is often complex and not fully understood.
Chronic Obstructive Pulmonary Disease (COPD) and Allergies
While not directly caused by allergies, some studies suggest a possible link between allergies and an increased risk of developing COPD. COPD is a progressive lung disease that primarily affects the airways and air sacs in the lungs, leading to breathing difficulties. While allergies don't cause COPD directly, the chronic inflammation associated with allergies might contribute to a more severe progression of the disease if someone already has a predisposition. More research is needed to establish a definitive link.
The Role of Infections in Allergic Individuals
Individuals with allergies might be more susceptible to respiratory infections, such as bronchitis or pneumonia. These infections can cause inflammation in the lungs, and repeated or severe infections can, over time, contribute to lung damage and potential scarring. It's important to note that the scarring is a result of the infection, not the allergy itself, but the allergy could have increased the susceptibility to the infection.
| Condition | Mechanism of Lung Damage | Scarring Likelihood |
|---|---|---|
| Allergic Asthma | Airway remodeling, chronic inflammation | Low; more likely airway changes than true scarring |
| Hypersensitivity Pneumonitis | Direct lung tissue damage, interstitial lung disease | High |
| EGPA | Vasculitis, granuloma formation, blood vessel damage | High |
| COPD (with allergy association) | Chronic inflammation, airway obstruction | Possible, but mainly due to COPD itself |
| Respiratory Infections (in allergic individuals) | Inflammation from infection | Possible, dependent on severity and frequency of infections |
Can Allergies Scar Your Lungs?
Allergies, while often inconvenient and uncomfortable, generally don't directly cause scarring in the lungs. However, severe and prolonged allergic reactions, as well as the underlying conditions sometimes associated with allergies, can have indirect effects that might lead to lung damage over time. It's crucial to understand that this is not a common outcome of typical allergic reactions like hay fever or mild food allergies. The link between allergies and lung scarring is complex and often involves other factors.
Allergic Asthma and Lung Damage
Allergic asthma is a common condition where an allergic reaction triggers inflammation and constriction of the airways. While asthma itself doesn't directly cause scarring (fibrosis), severe, uncontrolled asthma can lead to airway remodeling. This involves changes in the structure of the airways, including thickening of the walls and increased mucus production. Over many years, this remodeling can potentially contribute to irreversible lung damage, though it's not technically scarring in the same way a cut scars. The key here is the long-term, poorly managed inflammation.
Hypersensitivity Pneumonitis and Lung Scarring
Hypersensitivity pneumonitis (HP) is a rare but serious lung disease caused by an allergic reaction to inhaled substances like mold spores, bird droppings, or certain dusts. Unlike typical allergies, HP involves a more intense immune response that directly damages the lung tissue. This damage can lead to interstitial lung disease, a group of conditions that cause scarring and inflammation in the spaces between the air sacs in the lungs. HP is a severe condition that requires prompt diagnosis and treatment to prevent permanent lung damage.
Eosinophilic Granulomatosis with Polyangiitis (EGPA)
EGPA is a rare condition that affects the blood vessels and can also involve the lungs. It's considered a type of vasculitis, which is inflammation of the blood vessels. Although linked to allergies in some cases, EGPA's main issue is the inflammation in blood vessels, which can lead to the formation of granulomas (clusters of immune cells) and damage to lung tissue. This damage can result in scarring and other significant lung problems. It is important to emphasize that EGPA's relationship to allergies is often complex and not fully understood.
Chronic Obstructive Pulmonary Disease (COPD) and Allergies
While not directly caused by allergies, some studies suggest a possible link between allergies and an increased risk of developing COPD. COPD is a progressive lung disease that primarily affects the airways and air sacs in the lungs, leading to breathing difficulties. While allergies don't cause COPD directly, the chronic inflammation associated with allergies might contribute to a more severe progression of the disease if someone already has a predisposition. More research is needed to establish a definitive link.
The Role of Infections in Allergic Individuals
Individuals with allergies might be more susceptible to respiratory infections, such as bronchitis or pneumonia. These infections can cause inflammation in the lungs, and repeated or severe infections can, over time, contribute to lung damage and potential scarring. It's important to note that the scarring is a result of the infection, not the allergy itself, but the allergy could have increased the susceptibility to the infection.
| Condition | Mechanism of Lung Damage | Scarring Likelihood |
|---|---|---|
| Allergic Asthma | Airway remodeling, chronic inflammation | Low; more likely airway changes than true scarring |
| Hypersensitivity Pneumonitis | Direct lung tissue damage, interstitial lung disease | High |
| EGPA | Vasculitis, granuloma formation, blood vessel damage | High |
| COPD (with allergy association) | Chronic inflammation, airway obstruction | Possible, but mainly due to COPD itself |
| Respiratory Infections (in allergic individuals) | Inflammation from infection | Possible, dependent on severity and frequency of infections |
What are the symptoms of allergies in the lungs?
Allergic reactions in the lungs, often stemming from inhaling allergens like pollen, dust mites, pet dander, or mold spores, manifest in a variety of ways. These symptoms range from mild to severe and can significantly impact respiratory function and overall well-being. The severity depends on the individual's sensitivity, the amount of allergen exposure, and the specific allergen involved. Some symptoms are relatively common, while others might indicate a more serious allergic reaction requiring immediate medical attention.
Wheezing and Cough
Wheezing is a high-pitched whistling sound that occurs during breathing, particularly exhalation. It's caused by the narrowing of the airways due to inflammation and constriction of the smooth muscles surrounding the bronchioles. A persistent cough, often dry and hacking, is another common symptom. The cough can be triggered by the irritation of the airways. Both wheezing and coughing are hallmark signs of allergic asthma, a condition where lung inflammation is triggered by an allergic reaction.
- Wheezing: A high-pitched whistling sound during breathing.
- Cough: Often dry, hacking, and persistent.
- Shortness of Breath: Difficulty breathing, particularly during exertion.
Shortness of Breath and Chest Tightness
Shortness of breath (dyspnea) is a feeling of breathlessness or difficulty breathing. It occurs when the airways are narrowed, restricting the flow of air into and out of the lungs. This can be accompanied by a sensation of tightness or pressure in the chest, making it feel difficult to expand the lungs fully. The severity of shortness of breath can vary from mild discomfort to a life-threatening inability to breathe.
- Difficulty inhaling or exhaling air.
- Feeling of chest constriction or tightness.
- Increased respiratory rate (breathing faster than normal).
Increased Mucus Production
Allergies in the lungs often lead to an increase in mucus production. The body tries to expel the irritants causing the allergic reaction by producing more mucus, which can be thicker and stickier than usual. This excess mucus can clog the airways, further hindering airflow and contributing to coughing and wheezing. Excessive mucus production can also lead to a productive cough, where phlegm is expelled.
- Increased amount of mucus produced.
- Thick, sticky mucus.
- Productive cough (coughing up phlegm).
Frequent Respiratory Infections
Individuals with lung allergies are more susceptible to respiratory infections such as bronchitis and pneumonia. The inflammation and irritation in the airways caused by allergies weaken the lungs' defense mechanisms against viruses and bacteria, making them more vulnerable to infection. Frequent respiratory infections can further compromise lung function and lead to worsening symptoms. This is because the already inflamed airways are more susceptible to further infection.
- Increased frequency of colds and flu.
- Development of bronchitis or pneumonia.
- Persistent cough and respiratory symptoms.
Postnasal Drip
Although primarily affecting the nose and sinuses, postnasal drip—the excessive drainage of mucus from the back of the nose into the throat—can significantly affect the lungs. The excess mucus irritates the airways, triggering coughing and potentially leading to wheezing and shortness of breath. This irritation contributes to the overall inflammatory response in the respiratory system. This constant dripping of mucus irritates the sensitive lining of the lungs, exacerbating symptoms.
- Excess mucus dripping down the back of the throat.
- Throat clearing and coughing.
- Irritation and inflammation of the airways.
How to cure lung allergies?
:max_bytes(150000):strip_icc()/respiratory-allergies-symptoms-causes-and-treatment-5206183-5205177-final-7af9eb5916eb4a8dacf8b9bd516cad85.jpg)
How to Cure Lung Allergies?
There is no known cure for lung allergies (allergic asthma or allergic bronchopulmonary aspergillosis), but they can be effectively managed to significantly reduce symptoms and improve quality of life. Treatment focuses on controlling the underlying inflammation and preventing allergic reactions. This usually involves a combination of approaches tailored to the individual's specific triggers and severity of symptoms.
Identifying and Avoiding Allergens
The cornerstone of allergy management is identifying and avoiding your specific allergens. This requires careful attention to your environment and potential triggers. Common lung allergy triggers include pollen, dust mites, pet dander, mold, and certain foods. Accurate identification often involves allergy testing performed by an allergist or immunologist. Once identified, avoidance strategies become crucial.
- Keep your home clean: Regularly dust, vacuum, and wash bedding in hot water.
- Use air purifiers: These can filter out airborne allergens in your home.
- Control humidity: Low humidity helps minimize mold growth.
Medication for Symptom Relief and Prevention
Several medications are available to treat lung allergy symptoms and prevent future reactions. These medications work through different mechanisms, often used in combination for optimal results. Choosing the right medication and dosage requires consultation with a healthcare professional.
- Inhalers (corticosteroids, bronchodilators): These deliver medication directly to the lungs, reducing inflammation and opening airways.
- Oral medications (antihistamines, leukotriene modifiers): These address broader allergy symptoms such as itching, sneezing, and inflammation.
- Biologics (e.g., monoclonal antibodies): Newer treatments targeting specific immune pathways for severe cases.
Immunotherapy (Allergy Shots)
For some individuals with persistent lung allergies, immunotherapy (also known as allergy shots or sublingual immunotherapy) might be considered. This involves gradually introducing increasing doses of the allergen to desensitize the immune system over time, reducing the allergic reaction. Immunotherapy is a long-term treatment and requires regular visits to an allergist.
- Allergy shots are administered by a healthcare professional.
- Sublingual immunotherapy involves placing drops under the tongue.
- Effectiveness varies depending on the allergen and the individual.
Lifestyle Changes and Environmental Controls
Along with medical treatments, lifestyle modifications and environmental controls play a vital role in lung allergy management. These strategies aim to minimize exposure to triggers and improve overall respiratory health.
- Regular exercise can improve lung function and overall fitness.
- Quit smoking and avoid secondhand smoke.
- Manage stress levels as stress can exacerbate allergy symptoms.
Monitoring and Regular Check-ups
Regular monitoring of lung function and allergy symptoms is crucial for effective management. This typically involves regular visits to a doctor or allergist for assessments, peak flow measurements, and adjustments to treatment plans as needed. Early detection and proactive management are key to preventing serious complications.
- Keep a symptom diary to track triggers and responses.
- Use a peak flow meter to monitor lung function.
- Attend regular check-ups with your doctor or allergist.
What causes scarring around the lungs?

Scarring around the lungs, medically known as pulmonary fibrosis, is a complex condition resulting from the lungs' attempt to repair damaged tissue. This repair process, however, can lead to the formation of excessive scar tissue, which stiffens the lungs and hinders their ability to function properly. The underlying causes are varied and can be broadly categorized as idiopathic (unknown cause), or linked to specific diseases, environmental exposures, or medical treatments. The scarring process involves the abnormal accumulation of extracellular matrix proteins, primarily collagen, leading to the characteristic thickening and hardening of lung tissue. The severity of scarring and its impact on lung function depend on the extent of the damage and the body's response to it. Ultimately, the precise mechanisms triggering the excessive scar tissue formation in many cases remain poorly understood, making diagnosis and treatment challenging.
Idiopathic Pulmonary Fibrosis (IPF)
Idiopathic pulmonary fibrosis (IPF) is the most common form of pulmonary fibrosis, where the cause remains unknown. It typically affects older adults and progresses slowly over time. While the exact trigger remains elusive, several factors are suspected to play a role, including genetic predisposition and environmental exposures. Research suggests that genetic abnormalities may affect the body's ability to repair lung injuries effectively, leading to excessive scarring.
- Genetic predisposition: Certain genetic variations increase the risk of developing IPF.
- Environmental triggers: Exposure to certain dusts, fumes, or gases could contribute to the development of IPF.
- Immune system dysfunction: Abnormal immune responses may play a role in the development and progression of IPF.
Occupational and Environmental Exposures
Exposure to various environmental and occupational hazards can significantly increase the risk of developing pulmonary fibrosis. Inhaled particles such as asbestos, silica, coal dust, and certain types of metal dust can cause significant lung damage, leading to scarring. Harmful gases, including chlorine and nitrogen dioxide, can also induce lung injury and fibrosis. The severity of lung damage depends on the duration and intensity of exposure. Early detection and avoidance of these harmful substances are crucial in preventing pulmonary fibrosis.
- Asbestosis: Inhalation of asbestos fibers leads to significant lung scarring.
- Silicosis: Inhalation of silica dust results in the formation of scar tissue in the lungs.
- Coal worker's pneumoconiosis: Prolonged exposure to coal dust causes lung scarring and black lung disease.
Autoimmune Diseases
Certain autoimmune diseases, where the immune system mistakenly attacks the body's own tissues, can cause lung inflammation and subsequent scarring. Conditions such as rheumatoid arthritis, lupus, and scleroderma are known to increase the risk of pulmonary fibrosis. The immune system's aberrant activity leads to the release of inflammatory molecules that damage lung tissue and promote the formation of scar tissue. Treating the underlying autoimmune condition is essential in managing the associated pulmonary fibrosis.
- Rheumatoid arthritis: Inflammation associated with this disease can damage lung tissue.
- Systemic lupus erythematosus (SLE): Autoantibodies can attack lung tissue, leading to fibrosis.
- Scleroderma: The excessive production of collagen can cause significant lung scarring.
Medications and Radiation Therapy
Some medications and radiation therapy can cause lung damage as a side effect, leading to pulmonary fibrosis. Certain chemotherapy drugs used in cancer treatment are known to have pulmonary toxicity, resulting in lung scarring. Radiation therapy aimed at chest tumors can also damage lung tissue, inducing fibrosis. Careful monitoring and risk assessment are necessary when administering these treatments to minimize the risk of developing pulmonary fibrosis.
- Chemotherapy drugs: Some anticancer drugs can cause lung damage as a side effect.
- Radiation therapy to the chest: High doses of radiation can damage lung tissue, leading to fibrosis.
- Amiodarone: This medication used to treat irregular heartbeats can, in some cases, cause lung damage.
Genetic Factors
Genetic mutations can play a role in the development of pulmonary fibrosis. Several genes have been identified that are associated with an increased risk of developing IPF and other forms of pulmonary fibrosis. These mutations often affect the proteins involved in maintaining the structure and function of the lungs, increasing susceptibility to damage and abnormal scar formation. Further research is ongoing to fully understand the complex interplay between genetic factors and environmental influences in the pathogenesis of pulmonary fibrosis.
- Mutations in the surfactant protein genes: These genes are involved in maintaining lung function.
- Mutations in telomerase genes: Telomeres protect the ends of chromosomes; mutations can lead to cell damage.
- Mutations in other genes involved in lung repair and fibrosis: Ongoing research is identifying more genes associated with the disease.
What are the symptoms of long term allergies?
What are the symptoms of long-term allergies?
Long-term allergies, also known as chronic allergies, can manifest in a variety of ways, and the symptoms can vary greatly depending on the allergen and the individual's sensitivity. Symptoms can range from mild to severe and may impact multiple systems in the body. Unlike acute allergic reactions, which are typically immediate and intense, chronic allergies present with persistent and recurring symptoms over extended periods, often for weeks, months, or even years. The severity and frequency of symptoms can fluctuate depending on exposure levels to the allergen.
Persistent Respiratory Symptoms
One of the most common manifestations of long-term allergies is persistent respiratory irritation. This can significantly impact quality of life, leading to chronic coughing, wheezing, and shortness of breath. These symptoms are often accompanied by a persistent feeling of tightness or pressure in the chest, making everyday activities difficult. The constant inflammation in the airways can also lead to recurrent infections.
- Chronic Cough: A persistent cough that is not related to illness.
- Wheezing: A whistling sound during breathing.
- Shortness of breath: Difficulty breathing or feeling breathless.
Persistent Skin Issues
Chronic allergies frequently affect the skin, resulting in a variety of long-term dermatological problems. Eczema, a chronic inflammatory skin condition, is a common manifestation, characterized by itchy, red, and inflamed skin. Furthermore, long-term allergic reactions can exacerbate existing skin conditions or trigger new ones. This can lead to a cycle of inflammation and irritation, making it difficult to manage symptoms. Treatment often involves topical corticosteroids and avoiding triggers.
- Eczema/Atopic Dermatitis: Itchy, inflamed, and often cracked skin.
- Hives: Raised, itchy welts on the skin.
- Chronic Itching: Persistent itching even without visible skin lesions.
Chronic Sinus Problems
The sinuses are highly susceptible to allergic reactions, and long-term allergies often lead to persistent sinus issues. This can manifest as chronic sinusitis, marked by nasal congestion, postnasal drip, and facial pressure. These symptoms can interfere with sleep, concentration, and overall well-being. In severe cases, chronic sinus infections can develop, requiring medical intervention.
- Nasal Congestion: A stuffy nose.
- Postnasal Drip: Mucus dripping down the back of the throat.
- Facial Pain/Pressure: Pain or pressure in the sinuses.
Eye Irritation and Conjunctivitis
The eyes are another common site of allergic reactions, and long-term allergies can lead to chronic eye irritation. Allergic conjunctivitis, characterized by itchy, watery, and red eyes, is a frequent symptom. This can be accompanied by swelling of the eyelids and increased sensitivity to light. In severe cases, corneal damage may occur. Consistent management is needed to alleviate the symptoms.
- Itchy, Watery Eyes: Persistent itching and excessive tearing.
- Red Eyes: Bloodshot or inflamed eyes.
- Swollen Eyelids: Puffiness and inflammation around the eyes.
Gastrointestinal Problems
While less common than respiratory or skin symptoms, long-term allergies can also affect the digestive system. Food allergies are a significant factor, leading to symptoms such as bloating, abdominal pain, diarrhea, and nausea. These gastrointestinal problems can be chronic and significantly affect nutrient absorption and overall health. Careful dietary management and identification of food triggers are crucial for managing these symptoms.
- Abdominal Pain: Persistent or recurring stomach pain.
- Bloating: Feeling of fullness and distention in the abdomen.
- Diarrhea: Loose, watery stools.
Can allergies cause scarring in my lungs?
While allergies themselves don't directly cause scarring in the lungs (pulmonary fibrosis), they can contribute to conditions that do lead to scarring. Allergic asthma, for example, is a significant risk factor. In asthma, the airways become inflamed and narrowed in response to allergens. Chronic inflammation, a hallmark of poorly controlled asthma, can over time damage lung tissue. This damage isn't always scarring in the traditional sense, like a surgical scar, but rather a thickening and stiffening of the airways and lung tissue, reducing lung function. This is often seen as airway remodeling, characterized by changes in the structure of the airways. Additionally, some severe allergic reactions can trigger a condition called hypersensitivity pneumonitis, which is an inflammatory lung disease that can lead to lung scarring. This is less common than the effects of poorly managed asthma, however. It's crucial to effectively manage allergies and asthma to minimize the risk of long-term lung damage. Proper medication, allergen avoidance, and regular check-ups with a doctor are key to preventing the development of serious lung conditions. The severity and long-term impact depend heavily on the individual, the specific allergy, and the effectiveness of treatment.
What are the symptoms of lung scarring from allergies?
It's important to note that lung scarring related to allergies isn't a direct consequence of the allergy itself but rather a complication of conditions like poorly controlled asthma or hypersensitivity pneumonitis. Symptoms therefore vary depending on the underlying cause and the severity of the lung damage. Common symptoms related to allergic asthma that may indicate progression towards scarring include persistent coughing, wheezing, shortness of breath, especially during exertion, and chest tightness. These symptoms, if left untreated, can worsen over time. In cases of hypersensitivity pneumonitis, symptoms can be more severe and include a dry cough, shortness of breath, fatigue, fever, and weight loss. As the scarring progresses, symptoms often become more pronounced, and the individual may experience decreased exercise tolerance, a chronic cough that doesn't resolve, and increasing shortness of breath even at rest. It's crucial to seek medical attention if you experience any of these symptoms, particularly if they're persistent or worsening, as early diagnosis and treatment are vital in preventing further lung damage. A healthcare professional will be able to accurately diagnose the underlying cause and recommend appropriate treatment.
How is lung scarring from allergies diagnosed?
Diagnosing lung scarring related to allergies requires a comprehensive evaluation by a physician, typically a pulmonologist. The process often begins with a thorough medical history review, including a detailed account of allergic symptoms, asthma history, and exposure to potential allergens. A physical exam will assess breathing patterns, lung sounds, and overall health. Imaging tests such as chest X-rays and high-resolution CT scans are crucial in visualizing the lungs and detecting any scarring or abnormalities. Pulmonary function tests (PFTs) measure lung capacity and airflow, providing valuable information about the extent of lung damage. Bronchoscopy, a procedure involving inserting a thin, flexible tube into the airways, may be performed to obtain tissue samples for biopsy. These samples can be examined under a microscope to confirm the presence of scarring and inflammation. Blood tests may also be conducted to identify markers of inflammation and assess the overall health of the lungs. The specific diagnostic tests used will depend on the individual's symptoms, medical history, and the physician's assessment.
Can lung scarring from allergies be reversed or treated?
Unfortunately, lung scarring, whether caused by allergic conditions or other factors, is often not fully reversible. Once significant scarring has occurred, the damaged lung tissue cannot be repaired. However, treatment focuses on managing symptoms, slowing the progression of the disease, and improving lung function. For conditions like allergic asthma, effective management involves controlling inflammation with medication such as inhaled corticosteroids, bronchodilators, and in some cases, biologics. Allergen avoidance strategies are crucial to minimize exposure to triggers. In cases of hypersensitivity pneumonitis, removing the offending allergen is paramount. Treatment may also include corticosteroids, immunosuppressants, and oxygen therapy. Pulmonary rehabilitation, a comprehensive program of exercise, education, and support, can significantly improve quality of life by enhancing respiratory function and overall physical fitness. While complete reversal of scarring might not be achievable, effective treatment can significantly improve symptoms, slow disease progression, and enhance a patient's quality of life. Regular monitoring and adherence to the prescribed treatment plan are essential for managing the condition long-term.

Deja una respuesta