Can drinking milk make allergies worse

For many years, people with allergies have been advised to avoid milk and dairy products. This is because milk proteins can trigger an allergic reaction in some individuals. However, recent research suggests that drinking milk may not make allergies worse and may even help to reduce the risk of developing allergies in children.
Can Drinking Milk Worsen Allergies?
The relationship between milk consumption and allergies is complex and not fully understood. While milk itself isn't directly a known allergen for most people, it can exacerbate existing allergies or contribute to the development of others in some individuals. This is due to several factors, including the presence of specific proteins, individual sensitivities, and the interplay with other dietary components. It's crucial to understand that a direct causal link isn't always established, and reactions can vary widely depending on the individual.
Milk Proteins and Allergic Reactions
Cow's milk contains various proteins, primarily casein and whey, that are common allergens. These proteins can trigger an immune response in susceptible individuals, leading to symptoms ranging from mild digestive upset to severe anaphylaxis. The severity of the reaction depends on factors like the amount of milk consumed, the individual's sensitivity, and the presence of other allergens in the diet. Infants and young children are particularly vulnerable to milk allergies, although these often subside with age. Some individuals may experience cross-reactivity with other dairy products like cheese or yogurt.
Milk and Existing Allergies
Consuming milk can potentially worsen existing allergies, especially those involving respiratory symptoms. This is because milk can increase inflammation in the body, making individuals more sensitive to other allergens. For example, someone with seasonal allergies might find their symptoms are intensified after consuming dairy products. The mechanisms behind this exacerbation aren't entirely clear, but it is thought to involve the inflammatory effects of certain milk proteins and the body's overall immune response.
Milk and the Development of New Allergies
There's ongoing research into whether milk consumption plays a role in the development of new allergies in children. Some studies suggest a link between early milk introduction and increased risk of developing allergies, while others haven't found a strong correlation. The timing and method of introducing milk into an infant's diet might be crucial factors. It's important to note that these are observational studies, and more research is needed to establish a definitive causal relationship. Genetic predisposition also plays a significant role in allergy development.
Lactose Intolerance vs. Milk Allergy
It's crucial to differentiate between lactose intolerance and a milk allergy. Lactose intolerance is a digestive issue caused by the inability to digest lactose, the sugar in milk. It produces symptoms like bloating, gas, and diarrhea, but it's not a true allergic reaction involving the immune system. A milk allergy, on the other hand, is an immune response to milk proteins, potentially leading to much more severe symptoms, including skin rashes, respiratory difficulties, and even anaphylaxis.
Managing Milk and Allergies
If you suspect a link between milk consumption and your allergies or those of your child, it's essential to consult a doctor or allergist. They can perform allergy testing to determine any sensitivities and recommend appropriate management strategies. This might involve eliminating milk from the diet, substituting with dairy alternatives, or taking other measures to manage symptoms. Careful monitoring of symptoms and keeping a food diary can also help identify potential triggers and patterns.
| Symptom | Milk Allergy | Lactose Intolerance |
|---|---|---|
| Skin rash | Yes | No |
| Respiratory issues (wheezing, shortness of breath) | Yes | No |
| Digestive upset (bloating, gas, diarrhea) | Yes (often) | Yes |
| Anaphylaxis | Possible (severe cases) | No |
| Immune system response | Yes | No |
Can Drinking Milk Worsen Allergies?
The relationship between milk consumption and allergies is complex and not fully understood. While milk itself isn't directly a known allergen for most people, it can exacerbate existing allergies or contribute to the development of others in some individuals. This is due to several factors, including the presence of specific proteins, individual sensitivities, and the interplay with other dietary components. It's crucial to understand that a direct causal link isn't always established, and reactions can vary widely depending on the individual.
Milk Proteins and Allergic Reactions
Cow's milk contains various proteins, primarily casein and whey, that are common allergens. These proteins can trigger an immune response in susceptible individuals, leading to symptoms ranging from mild digestive upset to severe anaphylaxis. The severity of the reaction depends on factors like the amount of milk consumed, the individual's sensitivity, and the presence of other allergens in the diet. Infants and young children are particularly vulnerable to milk allergies, although these often subside with age. Some individuals may experience cross-reactivity with other dairy products like cheese or yogurt.
Milk and Existing Allergies
Consuming milk can potentially worsen existing allergies, especially those involving respiratory symptoms. This is because milk can increase inflammation in the body, making individuals more sensitive to other allergens. For example, someone with seasonal allergies might find their symptoms are intensified after consuming dairy products. The mechanisms behind this exacerbation aren't entirely clear, but it is thought to involve the inflammatory effects of certain milk proteins and the body's overall immune response.
Milk and the Development of New Allergies
There's ongoing research into whether milk consumption plays a role in the development of new allergies in children. Some studies suggest a link between early milk introduction and increased risk of developing allergies, while others haven't found a strong correlation. The timing and method of introducing milk into an infant's diet might be crucial factors. It's important to note that these are observational studies, and more research is needed to establish a definitive causal relationship. Genetic predisposition also plays a significant role in allergy development.
Lactose Intolerance vs. Milk Allergy
It's crucial to differentiate between lactose intolerance and a milk allergy. Lactose intolerance is a digestive issue caused by the inability to digest lactose, the sugar in milk. It produces symptoms like bloating, gas, and diarrhea, but it's not a true allergic reaction involving the immune system. A milk allergy, on the other hand, is an immune response to milk proteins, potentially leading to much more severe symptoms, including skin rashes, respiratory difficulties, and even anaphylaxis.
Managing Milk and Allergies
If you suspect a link between milk consumption and your allergies or those of your child, it's essential to consult a doctor or allergist. They can perform allergy testing to determine any sensitivities and recommend appropriate management strategies. This might involve eliminating milk from the diet, substituting with dairy alternatives, or taking other measures to manage symptoms. Careful monitoring of symptoms and keeping a food diary can also help identify potential triggers and patterns.
| Symptom | Milk Allergy | Lactose Intolerance |
|---|---|---|
| Skin rash | Yes | No |
| Respiratory issues (wheezing, shortness of breath) | Yes | No |
| Digestive upset (bloating, gas, diarrhea) | Yes (often) | Yes |
| Anaphylaxis | Possible (severe cases) | No |
| Immune system response | Yes | No |
Does milk cause a histamine reaction?

Whether milk causes a histamine reaction is complex and not definitively yes or no. Milk itself doesn't contain significant amounts of histamine, unlike some fermented foods. However, milk can trigger histamine release in susceptible individuals through several mechanisms. This means that while milk isn't inherently high in histamine, it can indirectly lead to a histamine reaction in certain people. This reaction can manifest in a variety of ways depending on the individual's sensitivity and the specific components of the milk.
Histamine in Milk vs. Histamine Release
While cow's milk doesn't contain high levels of preformed histamine, it can trigger the body's mast cells to release their own store of histamine. This can happen in individuals with sensitivities to milk proteins or other components. The reaction isn't directly caused by the histamine inthe milk, but rather the body's response tothe milk. This distinction is crucial.
- Milk proteins: Certain proteins in milk, such as casein, can trigger an immune response in some people, leading to histamine release. This is more common in individuals with milk allergies or intolerances.
- Lactose intolerance: Although not directly a histamine reaction, lactose intolerance can cause gut inflammation, which can, in turn, indirectly increase histamine release.
- Other components: Certain additives or contaminants in milk could potentially influence histamine production in the body.
Milk and Mast Cell Activation
Mast cells are immune cells that release histamine and other inflammatory mediators. Certain components in milk can activate mast cells, leading to the release of histamine. This mast cell activation doesn't require a full-blown allergic reaction; it can happen even in individuals who are not clinically diagnosed with a milk allergy. The exact mechanisms behind this mast cell activation are still being studied but are likely related to specific milk proteins or other components interacting with mast cell receptors.
- Cross-reactivity: Some individuals allergic to other foods may experience cross-reactivity with milk proteins, leading to histamine release.
- Individual variations: The response to milk varies greatly depending on genetics, gut microbiome composition, and pre-existing conditions.
- Dosage effect: The amount of milk consumed can influence the severity of any histamine-related symptoms. Consuming large quantities of milk might be more likely to trigger a reaction.
Diagnosing Milk-Induced Histamine Reactions
Diagnosing milk-induced histamine reactions can be challenging because the symptoms can mimic other conditions. Elimination diets and allergy testing are often used to determine if milk is a trigger. It's important to note that a negative allergy test doesn't completely rule out a histamine reaction from milk, as the mechanisms involved are not always captured by standard allergy tests. A detailed medical history and careful consideration of symptoms are crucial.
- Elimination diet: Removing milk from the diet and observing for symptom improvement.
- Skin prick test: A test to check for allergic reactions to milk proteins.
- Blood tests: Can detect antibodies to milk proteins, but may not be conclusive for histamine reactions.
Symptoms of Milk-Induced Histamine Reactions
Symptoms of a milk-induced histamine reaction can vary widely. They may be mild or severe, depending on individual sensitivity and the amount of milk consumed. Symptoms often overlap with those of other conditions, making diagnosis challenging. It's crucial to consult a doctor if you suspect a milk-induced reaction.
- Gastrointestinal issues: Diarrhea, bloating, abdominal cramps.
- Skin reactions: Hives, itching, rash.
- Respiratory symptoms: Runny nose, congestion.
Managing Milk-Induced Histamine Reactions
If you suspect a milk-induced histamine reaction, managing symptoms involves identifying triggers and avoiding them. In some cases, medication may be necessary to manage symptoms. Consult a doctor or allergist to develop a personalized management plan. This might include dietary changes, medication, and strategies for reducing mast cell activation. Always seek professional medical advice before making significant dietary changes.
- Dietary modifications: Eliminating or reducing milk consumption.
- Antihistamines: Medication to counter the effects of histamine.
- Lifestyle changes: Managing stress and other factors that can influence histamine release.
What foods make allergies worse?

What Foods Make Allergies Worse?
Certain foods can exacerbate allergic reactions or increase the likelihood of experiencing symptoms. This isn't because they causethe allergy directly (the allergen is usually a protein), but because they can trigger a heightened immune response or interact with the allergic reaction in ways that worsen symptoms. The specific foods that worsen allergies vary widely depending on the individual's specific allergies and sensitivities. However, some common culprits include foods high in histamine, foods that trigger cross-reactivity, and foods that irritate the digestive system, leading to inflammation.
Histamine-Rich Foods
Histamine is a compound involved in the body's immune response. High histamine foods can worsen allergic reactions because they increase the amount of histamine already present in the body. Consuming these foods when experiencing an allergic reaction or having a predisposition to allergies can amplify symptoms. This is particularly relevant to those with histamine intolerance, but can also affect individuals with other allergies.
- Fermented foods: Sauerkraut, kimchi, yogurt, kefir.
- Aged cheeses: Cheddar, parmesan, brie.
- Smoked or cured meats: Salami, bacon, ham.
Foods with Cross-Reactivity
Cross-reactivity occurs when the immune system reacts to proteins in different foods that share similar structures. For example, someone allergic to birch pollen might experience symptoms when eating apples or hazelnuts because of similar proteins. This means the allergy isn't directly caused by the apple itself but rather the immune system misidentifying the apple protein as the birch pollen protein.
- Fruits: Apples, peaches, kiwi, melons (for pollen allergies).
- Nuts and seeds: Peanuts, tree nuts, sesame seeds (various cross-reactivities).
- Vegetables: Celery, tomatoes, potatoes (various cross-reactivities).
Highly Processed Foods
Processed foods often contain additives and preservatives that can trigger inflammatory responses in the body, exacerbating allergic reactions. These additives might not be allergens themselves but can contribute to overall inflammation, making someone more susceptible to allergy symptoms or worsening existing ones. Reducing the intake of highly processed foods can be beneficial for many allergy sufferers.
- Foods with artificial colors and flavors.
- Foods with high levels of sulfites (preservatives).
- Foods with high fructose corn syrup.
Foods That Irritate the Digestive System
Foods that cause digestive upset or inflammation can indirectly worsen allergies. This is because the gut plays a crucial role in immune function. Inflammation in the gut can make the body more prone to allergic reactions. Reducing intestinal irritation can help to minimize this effect.
- Spicy foods
- Fried foods
- Dairy products (in some individuals)
Alcohol
Alcohol, particularly certain types, can contain histamine or other compounds that exacerbate allergic reactions. Furthermore, alcohol can irritate the digestive system, potentially worsening inflammation and making allergy symptoms worse. The effect varies from person to person and the type of alcoholic beverage.
- Red wine
- Beer
- Certain spirits (depending on additives)
Is milk bad for skin allergies?
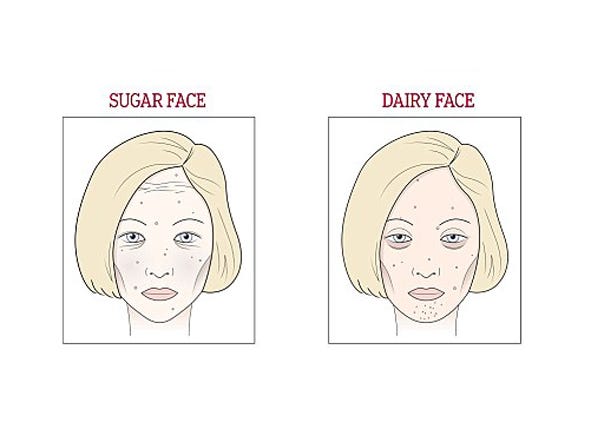
Whether milk is bad for skin allergies is complex and depends on several factors. While milk itself doesn't directly cause skin allergies, it contains proteins that can trigger allergic reactions in susceptible individuals. These proteins, primarily casein and whey, are found in various dairy products including milk, cheese, yogurt, and ice cream. The reaction isn't a direct toxicity but rather an immune system response. When someone with a milk allergy consumes dairy, their immune system mistakenly identifies these proteins as harmful invaders. This leads to the release of antibodies (IgE), initiating an allergic reaction which can manifest in various ways, including skin issues.
Milk Allergy Symptoms on the Skin
Skin manifestations of milk allergies are common and can vary in severity. They range from mild to severe, and a diagnosis should always involve a healthcare professional. Common skin reactions include eczema, hives (urticaria), and atopic dermatitis. It's important to note that the severity and type of reaction can differ significantly between individuals. Some people experience only mild itching and redness, while others can suffer severe inflammation and widespread rashes.
- Eczema: Characterized by dry, itchy, inflamed skin with potential cracking and weeping.
- Hives: Raised, itchy welts that appear suddenly and can disappear just as quickly.
- Atopic Dermatitis: A chronic inflammatory skin condition associated with dry skin, intense itching, and recurring rashes.
The Role of Casein and Whey
Casein and whey are the two major milk proteins most frequently implicated in allergic reactions. Casein is a slow-digesting protein, while whey is faster-digesting. These proteins are not easily broken down into smaller peptides by the digestive system in people with milk allergies. This means larger, intact proteins can enter the bloodstream, triggering an immune response. The sensitivity to either casein or whey can vary between individuals; some might be more sensitive to one than the other. It is important for individuals with milk allergies to carefully avoid products containing both proteins.
- Casein: Found predominantly in cheese and yogurt.
- Whey: Often found in whey protein supplements and some dairy products.
- Hidden sources of dairy: Be aware of hidden dairy sources in processed foods and medications.
Diagnosis and Treatment of Milk Allergy Related Skin Issues
A proper diagnosis is crucial for managing milk allergy-related skin problems. This typically involves a combination of medical history, physical examination, and allergy testing. Allergy testing, such as skin prick tests or blood tests, can help identify specific milk proteins causing the reaction. Treatment options focus on avoiding milk and dairy products, managing symptoms with antihistamines or topical corticosteroids, and potentially undergoing immunotherapy in some cases. The severity of the allergic reaction greatly impacts treatment decisions, ranging from simple avoidance to emergency medical intervention.
- Skin prick tests: A quick and relatively painless method of identifying allergens.
- Blood tests: Measure the levels of specific IgE antibodies against milk proteins.
- Elimination diet: Removing milk and dairy from the diet to observe any improvement in symptoms.
Cross-Reactivity with Other Dairy Products
Individuals with milk allergies may also experience reactions to other dairy products due to the presence of similar proteins. Cross-reactivity can occur with products like cheese, yogurt, butter, and even seemingly unrelated items that contain milk derivatives. These can include baked goods, processed meats, and even some medications. Carefully reading food labels and being aware of hidden sources of dairy are essential for managing milk allergies. Even small amounts can trigger a reaction.
- Cheese: Contains high levels of casein.
- Yogurt: Contains both casein and whey.
- Hidden dairy: Look out for words like "whey," "casein," "milk solids," "lactose" on food labels.
Managing Milk Allergy and Skin Conditions
Managing milk allergies and associated skin problems often requires a multi-pronged approach. Careful avoidance of dairy products is paramount, involving reading food labels diligently and asking about ingredients when eating out. Working closely with a healthcare professional, including an allergist or dermatologist, is crucial for developing an effective management plan. This might involve medication to manage symptoms, recommendations for skincare routines, and strategies for managing flare-ups. It's also vital to understand that individual reactions can differ greatly, and personalized management is essential.
- Read food labels carefully: Check for hidden dairy sources.
- Maintain a food diary: Track symptoms and identify trigger foods.
- Work with an allergist or dermatologist: Develop a personalized management plan.
How does milk help with allergies?

Milk itself does not directly treat or cure allergies. The relationship between milk and allergies is complex and often involves misconceptions. While milk is a common allergen, certain components within milk, or the way it's processed, might influence allergic responses in indirect ways. It's crucial to understand that milk should never be used as a treatment for allergies without consulting a doctor. Incorrect self-medication can be extremely dangerous.
Milk's Role in Infant Allergy Development
The timing and method of introducing milk into an infant's diet plays a significant role in allergy development. Early introduction of cow's milk proteins, particularly in infants with a family history of allergies, may increase the risk of developing milk allergies. Conversely, some studies suggest that introducing milk gradually and as part of a diverse diet could help to prevent future allergies. However, this is a complex issue with ongoing research, and a doctor's advice is vital.
- Early introduction may increase risk of milk allergy.
- Gradual introduction may potentially reduce risk (requires further research).
- Always consult a pediatrician for guidance on infant feeding.
Milk as a Source of Nutrients for Allergy Management
Milk can be a good source of certain nutrients that support overall health and might indirectly aid in managing allergy symptoms. For example, vitamin D plays a role in immune function, and calcium is crucial for bone health. A healthy immune system can better manage allergic reactions. However, this is not a direct treatment for allergies; it supports general well-being. If someone has a milk allergy, they should obtain these nutrients from other sources.
- Milk provides essential nutrients like vitamin D and calcium.
- These nutrients support immune function and overall health.
- Alternatives are needed for individuals with milk allergies.
Milk and Oral Tolerance
The concept of oral tolerance involves introducing small amounts of an allergen to gradually desensitize the immune system. Some research suggests that controlled exposure to milk proteins under medical supervision might help some children with mild milk allergies to tolerate milk better over time. However, this should only be attempted under the strict guidance of an allergist or immunologist. Improper implementation could lead to severe allergic reactions.
- Oral tolerance involves controlled exposure to allergens.
- It might improve tolerance in some individuals with mild allergies.
- Must be done under strict medical supervision to avoid dangerous reactions.
Milk and Other Food Allergies
Milk allergies sometimes co-occur with other food allergies, particularly those to soy, eggs, and peanuts. Managing these multiple allergies can be challenging, requiring careful dietary planning and attention to cross-contamination. Milk itself doesn't directly influence other food allergies, but the management strategies for one might overlap with another. It's crucial to work with a doctor or registered dietitian to create a safe and nutritious diet plan.
- Milk allergies often coincide with other food allergies.
- Careful diet planning is essential to manage multiple allergies.
- A healthcare professional should help develop a safe diet plan.
Misconceptions about Milk and Allergy Treatment
It's critical to dispel common misconceptions. Drinking milk to treat or prevent allergies is not only ineffective but can be dangerous. Milk is not a cure for allergies and can trigger severe reactions in individuals with milk allergies. Furthermore, assuming milk helps all allergies is incorrect; its impact varies greatly depending on the type of allergy.
- Milk does not cure or prevent allergies.
- Consuming milk can trigger severe reactions in those with milk allergies.
- Milk's relationship with allergy depends on the specific allergen.
Can drinking milk make my existing allergies worse?
It's a common concern, and the answer is a nuanced "possibly". While milk itself doesn't directly cause new allergies, it can exacerbate existing ones, particularly those related to dairy proteins. For individuals with lactose intolerance, consuming milk can lead to gastrointestinal distress like bloating, gas, and diarrhea. This isn't technically a worsening of an allergy, but it's an adverse reaction stemming from the inability to digest lactose, a sugar found in milk. However, for individuals with a dairy allergy (a true immunological reaction to milk proteins like casein or whey), consuming milk can trigger a range of symptoms, from mild skin rashes and itching to more serious reactions such as anaphylaxis. The severity of the reaction depends on the individual's sensitivity and the amount of milk consumed. Therefore, if you have a known allergy or intolerance, it's crucial to avoid milk and consult with an allergist or doctor to determine the best course of action. They can help you identify the specific allergens you react to and develop a management plan to minimize your risk of adverse reactions. Additionally, cross-contamination should be considered. Milk proteins can be found in many unexpected processed foods, so careful label reading is crucial for people with dairy allergies.
Does drinking milk increase the risk of developing new allergies?
The relationship between milk consumption and the development of new allergies is a complex area of research with inconclusive results. Some studies suggest that introducing cow's milk too early in infancy might be linked to a slightly higher risk of developing certain allergies later in life. This is particularly true for children with a family history of allergies or atopic eczema. However, other studies have found no such correlation. Many factors contribute to the development of allergies, including genetics, environmental exposures, and gut microbiome composition. Therefore, it's difficult to isolate the effect of milk consumption alone. The hygiene hypothesis, which suggests that increased exposure to certain microbes in early childhood might protect against allergies, also plays a role. Introducing milk too early might interfere with this beneficial microbial colonization. It is important to note that this isn't necessarily a cause-and-effect relationship; correlation doesn't equal causation. Ultimately, the current scientific understanding doesn't definitively confirm that drinking milk increases the risk of developing new allergies. Breastfeeding, however, is generally recommended for the first six months of life, as it is believed to provide protective benefits for infants and could even contribute to a reduced allergy risk.
Can milk worsen allergies other than dairy allergies?
While milk itself doesn't directly trigger allergies to other substances, there are some indirect ways it might worsen unrelated allergies. For instance, if someone has a food allergy and experiences gastrointestinal distress after consuming milk (due to lactose intolerance), this can compromise their gut barrier function. A compromised gut can increase the likelihood of allergens passing through the gut lining and triggering an allergic reaction. This is especially relevant to individuals with leaky gut syndrome. Additionally, certain additives or contaminants present in some milk products, though not milk itself, might interact with other allergies. For example, if a person has a sulfite allergy, they should be aware that some milk products might contain sulfites as preservatives. Therefore, while milk itself may not directly worsen allergies other than dairy allergies, related factors can indirectly affect the severity of other allergic reactions. Always carefully check food labels and consider the overall health of your gut when managing multiple allergies.
Should I avoid milk if I have allergies?
The answer to this question depends entirely on the specific allergy you have and its severity. If you have a confirmed dairy allergy, avoiding milk is strongly recommended to prevent potentially severe allergic reactions, ranging from mild skin rashes to life-threatening anaphylaxis. Even small amounts of milk can trigger reactions in some individuals. If you have another type of allergy, and your reaction to milk is only indirect (e.g., worsening of symptoms due to gastrointestinal distress from lactose intolerance), limiting or avoiding milk might be beneficial. This is especially true if you experience symptoms like bloating or diarrhea that compromise your immune system and might increase susceptibility to allergic reactions to other substances. It's essential to consult with your allergist or doctor. They can help determine the extent of your milk sensitivity and advise on the best approach for managing your allergies and overall health. They can also guide you towards alternative sources of calcium and other nutrients found in milk that are safe for you.
Deja una respuesta