Can water flush out an allergic reaction

Allergic reactions can be a nuisance, causing a range of uncomfortable symptoms from sneezing and a runny nose to itchy eyes and skin rashes. While there is no instant cure for allergies, many people wonder if there are ways to alleviate symptoms at home. One common suggestion is to flush out the allergen with water. But can water really flush out an allergic reaction?
Can Water Flush Out an Allergic Reaction?
No, water cannot flush out an allergic reaction. While drinking plenty of fluids is generally good advice for overall health and can help with some symptoms of mild allergic reactions like dehydration from diarrhea or vomiting, it does not address the underlying immune response causing the allergy. An allergic reaction is triggered by the body's immune system reacting to a perceived threat (the allergen). This reaction involves the release of histamine and other chemicals, leading to symptoms like itching, swelling, hives, and in severe cases, anaphylaxis. Water simply cannot remove or neutralize these chemicals from the bloodstream or tissues.
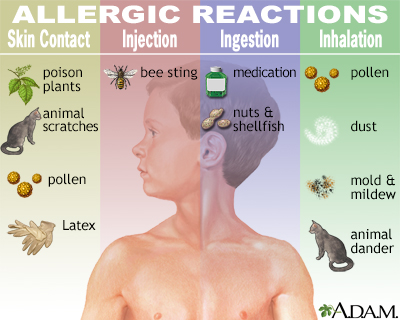
What causes an allergic reaction?
Allergic reactions are caused by the body's immune system overreacting to a normally harmless substance, known as an allergen. When exposed to an allergen (e.g., pollen, peanuts, pet dander), the immune system mistakenly identifies it as a threat. This triggers the release of histamine and other inflammatory mediators, leading to the characteristic symptoms of an allergic reaction. The severity of the reaction depends on factors like the amount of allergen exposure, the individual's sensitivity, and the specific allergen involved. Understanding the root cause is crucial for managing allergies effectively.
What are the symptoms of an allergic reaction?
Allergic reactions manifest in a wide range of symptoms, from mild to severe. Mild symptoms can include itching, sneezing, runny nose, mild rash, and watery eyes. More serious reactions may involve swelling of the face, lips, or tongue (angioedema), difficulty breathing (due to airway constriction), hives, and a drop in blood pressure (anaphylaxis). The severity and specific symptoms can vary depending on the allergen and the individual's sensitivity. Recognizing these symptoms is vital for prompt treatment.
What is the appropriate treatment for an allergic reaction?
Treatment for allergic reactions depends on the severity of the symptoms. Mild reactions often respond to over-the-counter antihistamines like diphenhydramine (Benadryl) or cetirizine (Zyrtec). For more severe reactions, immediate medical attention is crucial. Epinephrine (adrenaline) is the first-line treatment for anaphylaxis, a life-threatening allergic reaction. This medication is typically administered via an auto-injector (EpiPen). In addition to medication, other treatments may include oxygen therapy, intravenous fluids, and monitoring vital signs. Seeking professional medical advice is essential.
How can I prevent allergic reactions?
Preventing allergic reactions involves identifying and avoiding allergens. This may involve allergy testing to pinpoint specific triggers. Once allergens are identified, strategies such as avoiding exposure (e.g., staying indoors during high pollen counts), using allergen-blocking covers for mattresses and pillows, or carefully reading food labels can significantly reduce the risk of reactions. For some individuals, immunotherapy (allergy shots) may be an option to gradually desensitize the immune system to specific allergens. Proactive allergen avoidance is key to preventing reactions.
How to distinguish between a mild and severe allergic reaction?
Differentiating between mild and severe allergic reactions is critical for appropriate treatment. Mild reactions typically involve localized symptoms like sneezing, itching, or a mild rash. These symptoms are usually manageable with over-the-counter medications. Severe allergic reactions (anaphylaxis) are characterized by widespread symptoms such as difficulty breathing, swelling of the face and throat, dizziness, and a rapid drop in blood pressure. Anaphylaxis is a life-threatening emergency requiring immediate medical attention. Recognizing the distinction is vital for ensuring timely and appropriate treatment.
| Symptom | Mild Allergic Reaction | Severe Allergic Reaction (Anaphylaxis) |
|---|---|---|
| Skin | Itching, hives, rash | Widespread hives, swelling (angioedema), severe itching |
| Respiratory | Runny nose, sneezing, mild coughing | Wheezing, shortness of breath, difficulty breathing |
| Gastrointestinal | Mild nausea, stomach cramps | Severe nausea, vomiting, diarrhea |
| Cardiovascular | None | Rapid heart rate, drop in blood pressure, dizziness, fainting |
Can Water Flush Out an Allergic Reaction?
No, water cannot flush out an allergic reaction. While drinking plenty of fluids is generally good advice for overall health and can help with some symptoms of mild allergic reactions like dehydration from diarrhea or vomiting, it does not address the underlying immune response causing the allergy. An allergic reaction is triggered by the body's immune system reacting to a perceived threat (the allergen). This reaction involves the release of histamine and other chemicals, leading to symptoms like itching, swelling, hives, and in severe cases, anaphylaxis. Water simply cannot remove or neutralize these chemicals from the bloodstream or tissues.
What causes an allergic reaction?
Allergic reactions are caused by the body's immune system overreacting to a normally harmless substance, known as an allergen. When exposed to an allergen (e.g., pollen, peanuts, pet dander), the immune system mistakenly identifies it as a threat. This triggers the release of histamine and other inflammatory mediators, leading to the characteristic symptoms of an allergic reaction. The severity of the reaction depends on factors like the amount of allergen exposure, the individual's sensitivity, and the specific allergen involved. Understanding the root cause is crucial for managing allergies effectively.
What are the symptoms of an allergic reaction?
Allergic reactions manifest in a wide range of symptoms, from mild to severe. Mild symptoms can include itching, sneezing, runny nose, mild rash, and watery eyes. More serious reactions may involve swelling of the face, lips, or tongue (angioedema), difficulty breathing (due to airway constriction), hives, and a drop in blood pressure (anaphylaxis). The severity and specific symptoms can vary depending on the allergen and the individual's sensitivity. Recognizing these symptoms is vital for prompt treatment.
What is the appropriate treatment for an allergic reaction?
Treatment for allergic reactions depends on the severity of the symptoms. Mild reactions often respond to over-the-counter antihistamines like diphenhydramine (Benadryl) or cetirizine (Zyrtec). For more severe reactions, immediate medical attention is crucial. Epinephrine (adrenaline) is the first-line treatment for anaphylaxis, a life-threatening allergic reaction. This medication is typically administered via an auto-injector (EpiPen). In addition to medication, other treatments may include oxygen therapy, intravenous fluids, and monitoring vital signs. Seeking professional medical advice is essential.
How can I prevent allergic reactions?
Preventing allergic reactions involves identifying and avoiding allergens. This may involve allergy testing to pinpoint specific triggers. Once allergens are identified, strategies such as avoiding exposure (e.g., staying indoors during high pollen counts), using allergen-blocking covers for mattresses and pillows, or carefully reading food labels can significantly reduce the risk of reactions. For some individuals, immunotherapy (allergy shots) may be an option to gradually desensitize the immune system to specific allergens. Proactive allergen avoidance is key to preventing reactions.
How to distinguish between a mild and severe allergic reaction?
Differentiating between mild and severe allergic reactions is critical for appropriate treatment. Mild reactions typically involve localized symptoms like sneezing, itching, or a mild rash. These symptoms are usually manageable with over-the-counter medications. Severe allergic reactions (anaphylaxis) are characterized by widespread symptoms such as difficulty breathing, swelling of the face and throat, dizziness, and a rapid drop in blood pressure. Anaphylaxis is a life-threatening emergency requiring immediate medical attention. Recognizing the distinction is vital for ensuring timely and appropriate treatment.
| Symptom | Mild Allergic Reaction | Severe Allergic Reaction (Anaphylaxis) |
|---|---|---|
| Skin | Itching, hives, rash | Widespread hives, swelling (angioedema), severe itching |
| Respiratory | Runny nose, sneezing, mild coughing | Wheezing, shortness of breath, difficulty breathing |
| Gastrointestinal | Mild nausea, stomach cramps | Severe nausea, vomiting, diarrhea |
| Cardiovascular | None | Rapid heart rate, drop in blood pressure, dizziness, fainting |
Does drinking water help an allergic reaction?

Drinking water itself doesn't directly treat an allergic reaction. Allergic reactions are caused by the body's immune system overreacting to a harmless substance (allergen). This overreaction leads to the release of histamine and other chemicals, causing symptoms like itching, swelling, rash, and difficulty breathing. While water is crucial for overall health and hydration, it doesn't neutralize histamines or stop the immune response that's causing the allergic reaction. Adequate hydration is important for overall well-being, and this includes during an allergic reaction, but it's not a treatment for the reaction itself. You need to address the underlying cause and symptoms of the allergic reaction with appropriate medical intervention, which may include antihistamines or epinephrine depending on the severity.
How Hydration Affects Allergic Reactions
Maintaining proper hydration is essential for overall bodily function, and this is especially important during an allergic reaction. Dehydration can worsen symptoms and impact the body's ability to cope with the stress of the reaction. While water doesn't cure the allergy, sufficient hydration can aid in the body’s natural processes of eliminating allergens and mitigating some symptoms. However, it is crucial to remember that this is a supporting role, not a primary treatment.
- Supports the circulatory system, allowing for better distribution of medications if administered.
- Helps maintain normal blood pressure, which can be crucial in severe reactions.
- Aids in the removal of waste products through urine, which may assist in removing some of the byproducts of the allergic response.
Water vs. Oral Medication for Allergic Reactions
Water is absolutely NOT a substitute for proper medical treatment of an allergic reaction. Antihistamines, for example, directly counteract the effects of histamine, the chemical responsible for many allergy symptoms. Epinephrine, used in severe reactions (anaphylaxis), is a life-saving medication. While water is essential for overall health, it cannot address the underlying immunological processes causing the allergy.
- Oral antihistamines block histamine receptors, reducing symptoms like itching and swelling.
- Epinephrine (adrenaline) is a crucial treatment for anaphylaxis, a severe and potentially life-threatening allergic reaction.
- Other medications may be required depending on the specifics of the allergic reaction and its severity.
The Role of Hydration in General Well-being
Good hydration is fundamental for overall health and contributes to optimal bodily function. When your body is adequately hydrated, it can perform its functions more effectively, including its immune response. This general wellness may indirectly influence how your body responds to an allergic reaction. However, this is not a direct treatment of the allergy itself.
- Helps maintain optimal blood volume and pressure.
- Supports kidney function, which helps eliminate waste products.
- Plays a role in nutrient absorption and transportation.
Misconceptions about Water and Allergic Reactions
It's important to dispel any misconceptions that water alone can cure or significantly improve an allergic reaction. This is a dangerous belief, as relying solely on water could delay or prevent necessary medical intervention, potentially leading to severe complications. Water is a vital part of overall health, but it's not a treatment for allergic reactions.
- Drinking water will not stop an allergic reaction.
- Water does not neutralize histamines.
- Delaying proper medical treatment due to a belief in the effectiveness of water alone is dangerous.
Seeking Medical Attention for Allergic Reactions
Always seek appropriate medical attention for allergic reactions, especially if they are severe or worsening. Mild allergic reactions might be managed with over-the-counter antihistamines, but severe reactions (anaphylaxis) require immediate emergency medical care. Do not attempt to treat severe allergic reactions with water alone.
- Call emergency services immediately if you experience symptoms like difficulty breathing, swelling of the throat or face, or dizziness.
- Use an epinephrine auto-injector (EpiPen) if prescribed and trained to do so.
- Follow the advice of medical professionals regarding treatment and management of your allergies.
How do you flush out an allergic reaction?
There's no single method to "flush out" an allergic reaction, as the body's response varies depending on the allergen and the severity of the reaction. Treatment focuses on managing symptoms and preventing escalation. The goal is to counteract the effects of the allergen and alleviate the patient's discomfort. This usually involves a combination of approaches, ranging from home remedies for mild reactions to emergency medical intervention for severe ones.
Identifying and Removing the Allergen
The first step in managing an allergic reaction is to identify and remove the source of the allergen. This might involve removing a bee sting, washing off a plant irritant, or discarding contaminated food. Prompt removal can significantly reduce the severity and duration of the reaction. If you're unsure about the source, seeking medical attention is crucial.
- Carefully examine the area for any visible allergens.
- Remove clothing that may have come into contact with the allergen.
- Wash the affected area thoroughly with soap and water.
Administering Antihistamines
Oral antihistamines, such as diphenhydramine (Benadryl) or cetirizine (Zyrtec), can help relieve many symptoms of allergic reactions, including itching, hives, and swelling. They work by blocking the action of histamine, a chemical released by the body during an allergic response. Always follow the dosage instructions on the product label. For severe reactions, an injectable antihistamine might be necessary, administered by a healthcare professional.
- Take the recommended dosage of oral antihistamine immediately.
- Monitor your symptoms carefully after taking the medication.
- Avoid driving or operating machinery if drowsiness occurs.
Using Epinephrine (for Severe Reactions)
For severe allergic reactions (anaphylaxis), which can be life-threatening, epinephrine (adrenaline) is essential. Epinephrine is a potent medication that reverses the effects of anaphylaxis by constricting blood vessels, relaxing airways, and increasing heart rate. It should be administered immediately via an auto-injector (EpiPen, Auvi-Q) and followed by immediate medical attention.
- Administer epinephrine according to the instructions on the auto-injector.
- Call emergency medical services immediately.
- Remain with the person until help arrives, monitoring their breathing and circulation.
Seeking Medical Attention
Prompt medical attention is crucial for moderate to severe allergic reactions. Healthcare professionals can assess the severity of the reaction, provide appropriate treatment, and monitor for complications. Don't hesitate to seek medical assistance, especially if symptoms are worsening or if you experience difficulty breathing, swelling of the throat or tongue, dizziness, or loss of consciousness. Early intervention is key to preventing life-threatening complications.
- Call emergency services (911 in the US) or your local emergency number.
- Describe your symptoms accurately to the dispatcher.
- Follow the instructions of emergency medical personnel.
Supporting Measures for Mild Reactions
For mild allergic reactions, such as mild itching or a rash, supporting measures can provide relief. These might include applying cool compresses to reduce swelling and itching, taking a lukewarm bath with oatmeal or baking soda, or applying a topical hydrocortisone cream (for rashes). These measures are not substitutes for medical attention if the reaction worsens.
- Apply cool compresses to the affected area.
- Take a lukewarm bath with added oatmeal or baking soda.
- Apply a topical hydrocortisone cream, if appropriate.
Can water flush out histamines?
No, water alone cannot directly flush out histamines. Histamines are released by immune cells (mast cells and basophils) in response to an allergen or injury. These cells are located within tissues throughout the body, not just in the bloodstream. While drinking plenty of fluids, including water, is generally good for overall health and can help to maintain hydration which supports various bodily functions, it doesn't specifically target or remove histamines from the sites where they are already released and causing symptoms. The body's own metabolic processes are responsible for breaking down and eliminating histamines.
How Histamines Are Produced and Released
Histamines are involved in the body's inflammatory response. When the body encounters an allergen or experiences an injury, certain immune cells, specifically mast cells and basophils, release pre-formed histamines. This release leads to the characteristic symptoms of an allergic reaction like sneezing, itching, inflammation and swelling. The location of these immune cells is key: they are within the body's tissues. Simply drinking water won't reach and remove histamines from these locations.
- Mast cells reside in connective tissues throughout the body.
- Basophils circulate in the bloodstream.
- Histamine release is triggered by specific interactions between allergens and immune cells.
The Body's Mechanisms for Histamine Breakdown
The body has its own sophisticated mechanisms to regulate and eliminate histamine. Histamine is primarily metabolized by an enzyme called histamine-N-methyltransferase (HNMT) and also by diamine oxidase (DAO). These enzymes break down histamine into inactive metabolites, which are then excreted in the urine. The speed and efficiency of this process varies between individuals and depends on factors such as genetics and overall health.
- HNMT is found predominantly in the liver and kidneys.
- DAO is located in the intestinal lining and other tissues.
- Genetic variations in HNMT can influence the efficiency of histamine metabolism.
Hydration and its Indirect Effects on Allergic Symptoms
While water won't directly remove histamines, maintaining adequate hydration is crucial for overall well-being and can indirectly influence the body's response to allergic reactions. Good hydration supports healthy bodily functions that contribute to effective immune responses. Dehydration, on the other hand, may worsen some symptoms due to decreased efficiency in bodily processes.
- Proper hydration supports the immune system.
- Hydration aids in the removal of metabolic waste products, though not specifically histamines.
- Dehydration can exacerbate some allergy symptoms.
Medications for Histamine Control
Antihistamines are medications that directly counteract the effects of histamine. They work by blocking histamine receptors, preventing histamine from binding and causing symptoms. There are various types of antihistamines available, and your doctor can help determine the best option for your specific needs. They can provide relief for symptoms while the body's natural processes manage the elimination of the released histamines.
- Antihistamines are a common treatment for allergic reactions.
- They block the effects of histamine, not directly remove it.
- Different types of antihistamines have varying effects and durations.
How do you detox from an allergic reaction?

There is no such thing as "detoxing" from an allergic reaction in the sense of removing toxins. Allergic reactions are caused by the immune system overreacting to a harmless substance (allergen). The body doesn't need to be "detoxified"; it needs the allergic reaction to be stopped and its effects managed. Treatment focuses on managing symptoms and preventing future reactions. This involves removing the allergen and administering appropriate medical interventions.
Here's the information formatted as requested:
1. Identifying and Removing the Allergen
The first and most crucial step in managing an allergic reaction is to identify and remove the source of the allergen. This could involve anything from removing a bee sting, washing off a plant irritant, or getting rid of food that caused the reaction. This immediate action is critical to halting further exposure and preventing worsening symptoms.
- Carefully examine the environment to pinpoint potential allergens.
- Remove any clothing or items that may have come into contact with the allergen.
- Wash the affected area thoroughly with soap and water.
2. Administering Medication
Depending on the severity of the allergic reaction, medication will be necessary. For mild reactions, antihistamines like diphenhydramine (Benadryl) can be effective. For more severe reactions, such as anaphylaxis (a life-threatening condition), immediate medical attention is crucial, often involving an injection of epinephrine (adrenaline) with a EpiPen or similar auto-injector. Always follow the instructions provided by your doctor or pharmacist.
- Take antihistamines as directed to reduce symptoms like itching and swelling.
- If symptoms worsen or you experience difficulty breathing, seek immediate medical care.
- Carry an EpiPen or other prescribed medication if you have a history of severe allergic reactions.
3. Seeking Medical Attention
If the allergic reaction is severe or involves symptoms like difficulty breathing, swelling of the face or throat, dizziness, or loss of consciousness, immediate medical attention is absolutely necessary. This is a life-threatening emergency requiring immediate treatment. Don't hesitate to call emergency services or go to the nearest hospital.
- Call emergency services immediately (911 in the US).
- Describe the symptoms clearly to the dispatcher.
- Follow any instructions given by the emergency responders.
4. Managing Symptoms
Once the allergen is removed and medical intervention is provided, focus on managing remaining symptoms. This may involve taking over-the-counter pain relievers for headaches or muscle aches, using cool compresses for swelling, or applying topical creams for itching. Rest and hydration are also vital.
- Use cool compresses or ice packs to reduce swelling.
- Take over-the-counter pain relievers as needed.
- Drink plenty of fluids to stay hydrated.
5. Preventing Future Reactions
Once you've experienced an allergic reaction, it's crucial to work with your doctor or an allergist to determine the allergen and implement strategies to prevent future occurrences. This might include allergy testing, avoidance strategies, or immunotherapy (allergy shots). Prevention is key to managing allergies long-term.
- Undergo allergy testing to identify specific allergens.
- Work with your doctor to create an allergy management plan.
- Consider immunotherapy if appropriate.
Can drinking water help with an allergic reaction?
While drinking plenty of water is generally good for your health and can help with overall hydration, it won't directly flush out an allergic reaction. Allergic reactions are caused by your body's immune system overreacting to a specific allergen. This overreaction involves the release of histamine and other chemicals into your bloodstream, causing symptoms like hives, itching, swelling, and difficulty breathing. Drinking water won't remove these chemicals from your system. In fact, focusing solely on hydration might delay seeking appropriate medical attention, which is crucial in managing an allergic reaction, especially a severe one. Water is important for general well-being, but it's not a treatment or cure for allergic reactions. Think of it this way: if you have a cut, you wouldn't rely solely on drinking water to heal it; you'd clean and treat the wound. Similarly, an allergic reaction needs specific treatment tailored to its severity. The best approach is to identify the allergen, manage symptoms with appropriate medication (like antihistamines), and, if necessary, seek immediate medical help. For mild reactions, hydration supports overall health but doesn't actively combat the allergy itself.
Does water help with the symptoms of an allergic reaction?
Water itself doesn't directly alleviate the symptoms of an allergic reaction. While maintaining proper hydration is beneficial for overall health and well-being, it won't reduce swelling, itching, or difficulty breathing caused by an allergic response. These symptoms are caused by the release of inflammatory chemicals in your body. Although adequate fluid intake is a component of overall health management, it's not a treatment for the underlying immunological process of an allergic reaction. Antihistamines, epinephrine (in severe cases), and other medical interventions are much more effective in addressing the symptoms. Water can help support your body's functions, but it doesn't target the root cause of the allergic reaction or significantly diminish symptoms. It's important to address the allergy itself with appropriate medical care and medication.
Can water help to dilute allergens in the body?
The idea that water can dilute allergens in the body and thereby reduce the severity of an allergic reaction is a misconception. Allergic reactions aren't primarily caused by a high concentration of allergens; instead, they result from the body's immune system overreacting to even trace amounts of allergens. The immune system doesn't work on a simple dilution principle. Once an allergen triggers an allergic response, the body's reaction is already initiated through a complex chain of events involving histamine and other chemical mediators. Drinking water increases the overall fluid volume in your body, but it won't significantly change the concentration of these chemicals, nor will it remove the allergens from your system. The focus should be on managing the immune response, not on trying to dilute the allergen through increased water intake. This means using appropriate medications and seeking medical attention when necessary.
Should I only drink water during an allergic reaction?
No, relying solely on water during an allergic reaction is not recommended. While staying hydrated is crucial for overall health, water alone won't treat the underlying allergic response. Depending on the severity of the reaction, you might need specific medical interventions like antihistamines for mild reactions or epinephrine (adrenaline) for anaphylaxis. If the allergic reaction is severe or involves symptoms like difficulty breathing, swelling of the throat, or dizziness, you should immediately seek emergency medical help. Drinking water should be part of your overall health management, but it's not a substitute for appropriate medical care during an allergic reaction. It's essential to prioritize treatment of the allergic reaction itself, which often involves medication tailored to the specific symptoms. Focusing solely on water intake could delay critical interventions and exacerbate the situation.

Deja una respuesta