Can you build immunity against allergies

When faced with an unwelcome guest, the immune system springs into action, ready to defend the body from invaders. However, in the case of allergies, the immune system misidentifies harmless substances as threats, launching an unnecessary and often uncomfortable response. Can we train the immune system to recognize these substances as harmless, building immunity against allergies?
Can You Train Your Immune System to Ignore Allergens?
The short answer is: no, you cannot build true immunity against allergies in the same way you do against infections. While some people may experience a lessening of allergy symptoms over time, this isn't due to the immune system becoming "immune" to the allergen. Instead, it's usually a result of other factors, like changes in exposure, aging, or the development of tolerance mechanisms. Your immune system doesn't learn to ignore the allergen completely; it simply learns to react less severely or in a different way. Think of it more like managing the reaction rather than eliminating the sensitivity. The allergic response is a complex process involving many different cells and chemical mediators, making it difficult to completely switch off.
What is an Allergic Reaction?
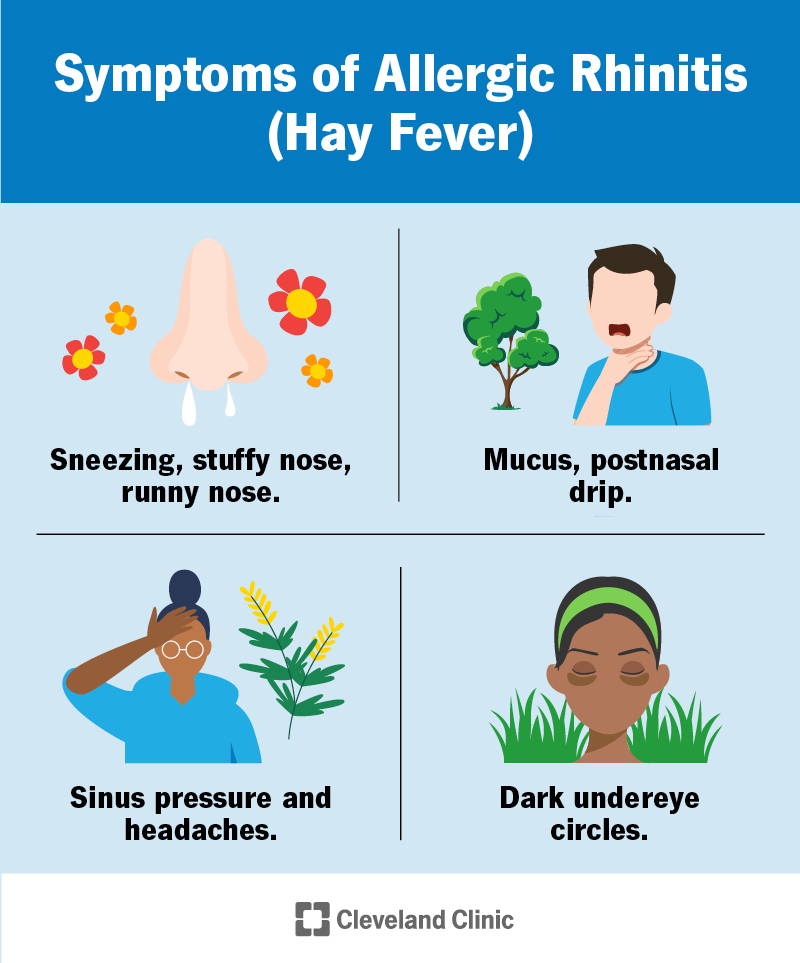
An allergic reaction occurs when your immune system mistakenly identifies a harmless substance (allergen), like pollen, pet dander, or peanuts, as a threat. This triggers a cascade of events, including the release of histamine and other inflammatory chemicals. These chemicals cause the characteristic symptoms of allergies, such as sneezing, itching, rash, and swelling. The immune system's initial response is to produce IgE antibodies specifically targeting the allergen. Upon subsequent exposure, these IgE antibodies bind to mast cells, triggering the release of inflammatory mediators.
Can Allergy Symptoms Decrease Over Time?
Yes, it's possible for allergy symptoms to lessen over time. This can be due to various factors: aging (the immune system can naturally become less reactive with age), changes in exposure (reduced contact with the allergen), or the development of a type of immune tolerance where the body learns to control the excessive immune response to the allergen, not eliminate it completely. However, these changes don't represent true immunity.
Immunotherapy: A Treatment, Not a Cure
Allergy immunotherapy, also known as desensitization, is a medical treatment that aims to modify the immune response to specific allergens. It involves gradually exposing the patient to increasing doses of the allergen over time, with the goal of reducing the severity of allergic reactions. While it can be effective in managing allergies, it doesn't eradicate the allergy; it helps to modify the immune response making the body less sensitive to future exposure. It is a long-term treatment that requires a commitment from the patient and is supervised by a medical professional. It is not a cure.
The Role of Genetics and Environment
Both genetics and environmental factors play a significant role in the development of allergies. Genetic predisposition can make some individuals more susceptible to developing allergies. Environmental exposures, particularly during early childhood, also influence the development of allergic sensitivities. This complexity underscores the challenges in achieving true immunity to allergens, as multiple interconnected factors contribute to the allergic response.
Lifestyle Changes and Allergy Management
While you can't develop true immunity, you can significantly manage your allergy symptoms through lifestyle changes. This includes avoiding allergens whenever possible (allergen avoidance), using medications to control symptoms (antihistamines, corticosteroids), and practicing good hygiene (frequent handwashing). These strategies don't build immunity but greatly reduce the impact of allergies on your life.
| Factor | Influence on Allergy Development/Management |
|---|---|
| Genetics | Predisposition to developing allergies |
| Environmental Exposure | Triggers allergic responses, influences severity |
| Age | Can lead to changes in symptom severity over time |
| Immunotherapy | Modifies the immune response, doesn't cure the allergy |
| Allergen Avoidance | Reduces exposure, minimizes symptoms |
| Medication | Controls symptoms, doesn't eliminate the allergy |
Can You Train Your Immune System to Ignore Allergens?
The short answer is: no, you cannot build true immunity against allergies in the same way you do against infections. While some people may experience a lessening of allergy symptoms over time, this isn't due to the immune system becoming "immune" to the allergen. Instead, it's usually a result of other factors, like changes in exposure, aging, or the development of tolerance mechanisms. Your immune system doesn't learn to ignore the allergen completely; it simply learns to react less severely or in a different way. Think of it more like managing the reaction rather than eliminating the sensitivity. The allergic response is a complex process involving many different cells and chemical mediators, making it difficult to completely switch off.
What is an Allergic Reaction?
An allergic reaction occurs when your immune system mistakenly identifies a harmless substance (allergen), like pollen, pet dander, or peanuts, as a threat. This triggers a cascade of events, including the release of histamine and other inflammatory chemicals. These chemicals cause the characteristic symptoms of allergies, such as sneezing, itching, rash, and swelling. The immune system's initial response is to produce IgE antibodies specifically targeting the allergen. Upon subsequent exposure, these IgE antibodies bind to mast cells, triggering the release of inflammatory mediators.
Can Allergy Symptoms Decrease Over Time?
Yes, it's possible for allergy symptoms to lessen over time. This can be due to various factors: aging (the immune system can naturally become less reactive with age), changes in exposure (reduced contact with the allergen), or the development of a type of immune tolerance where the body learns to control the excessive immune response to the allergen, not eliminate it completely. However, these changes don't represent true immunity.
Immunotherapy: A Treatment, Not a Cure
Allergy immunotherapy, also known as desensitization, is a medical treatment that aims to modify the immune response to specific allergens. It involves gradually exposing the patient to increasing doses of the allergen over time, with the goal of reducing the severity of allergic reactions. While it can be effective in managing allergies, it doesn't eradicate the allergy; it helps to modify the immune response making the body less sensitive to future exposure. It is a long-term treatment that requires a commitment from the patient and is supervised by a medical professional. It is not a cure.
The Role of Genetics and Environment
Both genetics and environmental factors play a significant role in the development of allergies. Genetic predisposition can make some individuals more susceptible to developing allergies. Environmental exposures, particularly during early childhood, also influence the development of allergic sensitivities. This complexity underscores the challenges in achieving true immunity to allergens, as multiple interconnected factors contribute to the allergic response.
Lifestyle Changes and Allergy Management
While you can't develop true immunity, you can significantly manage your allergy symptoms through lifestyle changes. This includes avoiding allergens whenever possible (allergen avoidance), using medications to control symptoms (antihistamines, corticosteroids), and practicing good hygiene (frequent handwashing). These strategies don't build immunity but greatly reduce the impact of allergies on your life.
| Factor | Influence on Allergy Development/Management |
|---|---|
| Genetics | Predisposition to developing allergies |
| Environmental Exposure | Triggers allergic responses, influences severity |
| Age | Can lead to changes in symptom severity over time |
| Immunotherapy | Modifies the immune response, doesn't cure the allergy |
| Allergen Avoidance | Reduces exposure, minimizes symptoms |
| Medication | Controls symptoms, doesn't eliminate the allergy |
Can you gain immunity to allergies?

No, you generally cannot gain immunity to allergies in the same way you can gain immunity to infectious diseases through vaccination or prior infection. Allergies are a result of your immune system overreacting to a harmless substance, called an allergen. This overreaction is mediated by IgE antibodies, which trigger the release of histamine and other inflammatory chemicals, leading to allergic symptoms. While some individuals may experience a decrease in the severity of their allergic reactions over time, this is not true immunity. Rather, it's often due to factors like changes in exposure, age-related immune system modifications, or the development of tolerance, a different process than true immunity.
What is Allergic Tolerance?
Allergic tolerance is a state where the immune system learns to ignore an allergen, reducing or eliminating allergic reactions. This is distinct from immunity, which implies complete protection. Tolerance can develop naturally over time or through specific therapies like immunotherapy (allergy shots). However, tolerance is not guaranteed, and it's allergen-specific – tolerance to one allergen doesn't mean tolerance to others.
- Development is gradual and not always successful: Tolerance doesn't happen overnight. It requires repeated, controlled exposure.
- Individual variation is significant: Some people develop tolerance easily, while others don't.
- Loss of tolerance is possible: Factors like high-level exposure or changes in the immune system can lead to a relapse of allergic symptoms even after developing tolerance.
The Role of the Immune System in Allergies
The immune system's response to allergens is complex, involving various cells and molecules. In allergic individuals, the initial exposure to an allergen sensitizes the immune system, leading to the production of IgE antibodies. Subsequent exposures trigger a rapid release of histamine and other inflammatory mediators from mast cells and basophils, leading to the characteristic symptoms of an allergic reaction. This hypersensitivity reaction is the hallmark of allergies, not a protective immune response like that seen in immunity to infections.
- IgE antibodies are key players: These antibodies bind to allergens and trigger mast cell degranulation.
- Histamine release causes symptoms: This inflammatory molecule contributes to symptoms like sneezing, itching, and swelling.
- Genetic predisposition plays a role: Some individuals are genetically more prone to developing allergies.
Immunotherapy (Allergy Shots)
Immunotherapy involves gradually increasing exposure to an allergen over time, aiming to induce tolerance. This method works by shifting the immune response from an IgE-mediated reaction to a more tolerant IgG-mediated response. While immunotherapy can be effective in reducing allergy symptoms, it is not a cure and does not confer true immunity. It requires ongoing treatment and may not be suitable for everyone.
- Gradual desensitization is key: The allergen dose is slowly increased to avoid triggering severe reactions.
- IgG antibody production is a goal: This helps to neutralize the allergen and prevent IgE-mediated reactions.
- Requires commitment and monitoring: Regular injections are needed, and patients must be monitored for potential side effects.
Age and Allergy Severity
Some people experience a reduction in allergy symptoms as they get older. This isn't due to acquired immunity but rather potentially to changes in their immune systems, lifestyle factors, or reduced exposure to allergens. For example, children often outgrow milk allergies, but this isn't because they develop immunity, but rather a shift in their immune response. It's crucial to remember that this isn't always the case, and allergy symptoms can persist or even worsen throughout life.
- Immune system maturation: The immune system undergoes significant changes with age, which might influence allergic responses.
- Lifestyle changes: Dietary modifications or changes in environment can affect allergy severity.
- Exposure levels: Reduced exposure to certain allergens might contribute to lessened symptoms.
Environmental Factors and Allergy Development
Environmental factors play a significant role in the development and severity of allergies. Exposure to certain pollutants, allergens, and infections during childhood can influence the risk of developing allergies. Hygiene hypothesis suggests that reduced exposure to microbes in early life might increase the risk of allergies. However, it’s important to note that environmental factors don't create immunity to allergies but can influence their development and course.
- Hygiene hypothesis: Lack of early exposure to microbes may increase allergy risk.
- Air pollution: Exposure to pollutants can worsen allergy symptoms.
- Pet exposure: Early exposure to pets can either increase or decrease allergy risk, depending on various factors.
Can you build tolerance for allergies?

No, you cannot truly "build a tolerance" to allergies in the same way you might build a tolerance to certain medications. Allergies are a result of your immune system mistakenly identifying a harmless substance (allergen) as a threat. This triggers a reaction, often involving the release of histamine and other chemicals, leading to symptoms like sneezing, itching, rash, or even life-threatening anaphylaxis. Your immune system doesn't "learn" to ignore the allergen; it continues to react in the same way upon repeated exposure. While some people may experience seemingly less severe reactions over time with repeated exposure, this is not true tolerance but rather a result of other factors.
Oral Immunotherapy (OIT)
Oral immunotherapy (OIT) is a treatment approach that aims to gradually desensitize individuals to specific allergens. It involves progressively increasing doses of the allergen over time, under strict medical supervision. The goal isn't to eliminate the allergy completely, but rather to increase the threshold at which a reaction occurs, allowing individuals to tolerate higher levels of the allergen. However, it's crucial to note that OIT carries risks, including allergic reactions during treatment, and requires a commitment to ongoing medical monitoring.
- Requires strict medical supervision: OIT must be administered by trained allergists in a controlled environment.
- Gradual dose increase: The amount of allergen administered is increased slowly over time to minimize the risk of serious reactions.
- Ongoing monitoring: Patients need regular check-ups and allergy testing throughout the treatment and afterward.
Natural Tolerance Development
In some cases, people might experience a decrease in the severity of their allergic symptoms over time without any specific intervention. This isn't true tolerance but rather a complex process that may involve changes in the immune system, exposure to diverse environmental factors, or simply a change in the amount of allergen exposure. It's not a predictable or reliable phenomenon and shouldn't be relied upon as a treatment for allergies. Many factors may play a role, including the type of allergen, age, and overall health.
- Not a reliable treatment strategy: It's not possible to predict or control this natural process.
- Multiple contributing factors: The exact reasons why this occurs are not fully understood.
- Unpredictable outcomes: Symptoms may vary significantly even with prolonged exposure.
Sublingual Immunotherapy (SLIT)
Similar to OIT, sublingual immunotherapy (SLIT) involves introducing small amounts of allergen, but it's administered under the tongue rather than orally. This method is generally considered safer than OIT, but it's also less effective at inducing tolerance in some cases. SLIT aims to reduce allergy symptoms, not necessarily eliminate the allergy. The process requires consistent administration for long periods and may not work for everyone.
- Less effective than OIT: It may not induce the same level of tolerance as oral immunotherapy.
- Self-administration: Once a maintenance dose is reached, SLIT can be self-administered at home.
- Longer treatment duration: SLIT usually requires treatment for several years to achieve optimal effects.
Allergen Avoidance
The most effective way to manage allergies is to avoid the allergen that triggers your symptoms. This can be challenging, as allergens are often present in multiple places and situations. However, by meticulously avoiding the allergen, you can prevent triggering an immune response and mitigate the severity of your allergy. This isn't building tolerance, but managing the condition. It's crucial to carefully identify allergens through allergy testing.
- Accurate allergen identification: Allergy testing helps pinpoint the specific allergen or allergens to avoid.
- Environmental controls: Removing allergens from your home and work environment is important.
- Dietary changes: Eliminating allergenic foods from your diet is necessary if you have a food allergy.
Medication Management
Antihistamines, decongestants, and other medications can help manage allergy symptoms. These medications don't change your immune response or create tolerance; instead, they alleviate the effects of the allergic reaction. They are a critical component of allergy management, but they don't address the underlying cause of the allergy.
- Symptom relief: Medications reduce the severity of symptoms, such as sneezing, itching, and inflammation.
- Prescription and over-the-counter options: Various medications are available to treat different types of allergies.
- Emergency medications: For severe allergic reactions (anaphylaxis), epinephrine is a life-saving medication.
Why are my allergies so bad all of a sudden?
The sudden worsening of your allergies could be due to a variety of factors. It's not uncommon for allergies to fluctuate in severity, even in individuals who have experienced them for a long time. Several elements might be contributing to this recent intensification. These include changes in your environment, exposure to new allergens, hormonal shifts, or even underlying medical conditions. Determining the precise cause necessitates careful consideration of these potential contributors and possibly a consultation with an allergist or doctor.
Increased Pollen Count
Higher pollen counts are a common culprit behind a sudden increase in allergy symptoms. Different plants release pollen at various times of the year, and fluctuations in weather patterns – such as unusually warm temperatures or extended periods of rain followed by sunshine – can lead to a dramatic spike in pollen levels. This sudden surge can overwhelm your immune system, leading to more severe symptoms than you're used to experiencing.
- Increased wind: Windy conditions spread pollen further and more efficiently.
- High temperatures: Warm weather accelerates pollen production.
- Unusually wet weather: A rainy period followed by sunshine can result in a massive pollen release.
New Allergens in Your Environment
You may have recently been exposed to a new allergen that your body hasn't encountered before. This could be due to a recent move, renovations to your home, or even changes in your workplace or daily routine. Your immune system will react strongly to this novel allergen, leading to a significant worsening of allergy symptoms. It's important to consider any environmental changes that may have occurred recently.
- Moving to a new area with different plant life.
- Introducing new pets or plants into your home.
- Undergoing home renovations, potentially exposing you to new mold or dust.
Changes in Your Immune System
Underlying health conditions or even stress can influence your immune system's response to allergens. For example, a weakened immune system due to illness or medication can make you more susceptible to allergic reactions. Similarly, increased stress levels can exacerbate allergy symptoms. Hormonal changes, particularly in women, also influence the immune system and can cause allergy fluctuations.
- Recent illness or infection weakening your immune response.
- Increased stress levels contributing to heightened sensitivity.
- Hormonal changes related to pregnancy, menstruation, or menopause.
Changes in Medication or Lifestyle
Changes to your medication or lifestyle can unexpectedly affect your allergies. Stopping or altering allergy medication can lead to a rapid return of symptoms and potentially more severe reactions. Similarly, dietary changes, a lack of sleep, or increased alcohol consumption can also trigger allergy flare-ups. Careful consideration of recent adjustments in any of these areas is necessary.
- Discontinuing or altering your allergy medication.
- Changes in diet that may be increasing your exposure to certain allergens.
- Lifestyle factors like poor sleep, increased stress, or higher alcohol consumption.
Hidden Allergens
You may be unaware of a new allergen source. Hidden allergens can be surprisingly difficult to pinpoint. These might include hidden mold growth within your home, a new cleaning product, or even changes in the types of fabrics you're frequently exposed to. Carefully investigating your environment and lifestyle for any potential new sources of allergens is an important step in managing these more intense symptoms.
- Mold growth in damp areas of your home.
- New cleaning products containing strong fragrances or chemicals.
- Exposure to new fabrics or materials in clothing or furnishings.
What is the best natural thing for allergies?

There's no single "best" natural remedy for allergies, as effectiveness varies greatly depending on the individual, the allergen, and the severity of the allergy. What works wonders for one person might not have any effect on another. Allergic reactions are complex, involving the immune system's response to perceived threats. While natural remedies can offer some relief for mild symptoms, they shouldn't replace medical advice or prescribed treatments for severe allergies. Always consult with a doctor or allergist before starting any new treatment, especially if you have a history of severe allergic reactions.
1. Identifying and Avoiding Allergens
The most effective "natural" approach to allergies is proactive avoidance of known allergens. This involves careful identification of what triggers your symptoms and minimizing or eliminating exposure. This is far more effective than any other method.
- Keep a detailed allergy diary to track your symptoms and potential triggers.
- Regularly clean your home, particularly bedding, carpets, and upholstery, to reduce dust mite exposure.
- Use air purifiers with HEPA filters to remove airborne allergens like pollen and pet dander.
2. Local Honey
Some people find relief from seasonal allergies by consuming local, raw honey. The theory is that it contains small amounts of local pollen, potentially helping to desensitize the immune system. However, scientific evidence supporting this is limited and results vary widely. It's important to note that honey can contain other allergens, and it's not suitable for infants.
- Choose raw, unfiltered honey from local beekeepers.
- Start with a small amount to check for any adverse reactions.
- Consult with a doctor or allergist before using honey as an allergy treatment.
3. Butterbur
Butterbur (Petasites hybridus) is a plant that has been traditionally used for allergy relief, containing compounds that may help reduce inflammation. However, it's crucial to use only purified butterbur extracts that are free from pyrrolizidine alkaloids (PAs), which are toxic liver compounds. Unpurified butterbur is dangerous and can cause serious liver damage.
- Only use purified butterbur extracts that are clearly labeled as PA-free.
- Follow the recommended dosage instructions carefully.
- Consult your doctor before taking butterbur, especially if you have liver problems or are taking other medications.
4. Nettle
Nettle (Urtica dioica) is another herb with anti-inflammatory properties that some find helpful for allergies. It's thought to stabilize mast cells, which release histamine (a key player in allergic reactions). Like with other natural remedies, the evidence for its effectiveness is mixed and more research is needed.
- Nettle can be taken as a tea, tincture, or capsule.
- Start with a low dose and gradually increase as tolerated.
- Consult your doctor before using nettle, especially if you have any underlying health conditions.
5. Quercetin
Quercetin is a plant-based flavonoid with antioxidant and anti-inflammatory properties. It's found in many fruits, vegetables, and other plants. Some studies suggest it may help reduce allergy symptoms by stabilizing mast cells and inhibiting histamine release. However, more research is needed to confirm its effectiveness as an allergy treatment.
- Quercetin is available in supplement form.
- Follow the recommended dosage instructions on the supplement label.
- Consult your doctor before taking quercetin supplements, especially if you are taking other medications.
Can you actually build immunity against allergies?
The short answer is: no, you can't build immunity against allergies in the same way you can build immunity against infections. Allergic reactions are caused by your immune system mistakenly identifying a harmless substance (allergen) as a threat. This leads to an exaggerated immune response, producing IgE antibodies and releasing histamine and other inflammatory chemicals. Unlike infections where your body develops memory cells to fight off future encounters with the same pathogen, allergies don't work this way. Your immune system doesn't "learn" to tolerate the allergen; instead, it continues to react excessively each time it encounters the allergen. While some people might experience a decrease in the severity of their symptoms over time, this is generally due to factors like age, changes in exposure, or better allergen management, rather than a genuine development of immunity. In fact, new allergies can develop throughout life, demonstrating the absence of true acquired immunity. Tolerance induction, a process being researched, aims to re-educate the immune system to respond less aggressively, but it’s not yet a widespread or readily available cure.
Can immunotherapy help build immunity against allergies?
Immunotherapy, often called allergy shots or sublingual immunotherapy (SLIT), is a treatment that aims to desensitize, rather than build immunity, to allergens. It works by gradually exposing you to increasing doses of the allergen, prompting the immune system to adapt its response. The goal isn't to completely eliminate the allergic reaction, but to reduce its severity and frequency. The mechanism behind its effectiveness isn't fully understood, but it's thought to involve shifting the immune response away from the IgE-mediated pathway (the immediate, severe reaction) towards more tolerant IgG responses. While it doesn't create true immunity, it can significantly improve the management of allergic symptoms and, in some cases, lead to long-term relief even after treatment is stopped. However, it's important to remember that immunotherapy requires a commitment to a long-term treatment plan, often involving multiple injections or daily medication, and isn't suitable for everyone. It’s crucial to consult with an allergist to determine suitability and manage potential side effects.
Can avoiding allergens build immunity?
No, avoiding allergens doesn't build immunity. In fact, the opposite may be true. Constantly avoiding an allergen can lead to a phenomenon called the "allergic march," where a child's immune system may become sensitized to other allergens. For example, avoiding peanuts might increase the risk of developing other food allergies or eczema. While avoiding allergens is crucial for managing symptoms and preventing severe reactions, particularly in individuals with severe allergies, it isn't a strategy to build immunity or prevent future allergies. The idea that exposure can desensitize is a complex one, and carefully managed, controlled exposure as part of immunotherapy is different than complete avoidance. Avoiding allergens primarily helps in managing the severity and frequency of allergic reactions in individuals already sensitized, not in building any sort of protective immunity.
Are there any natural ways to build immunity against allergies?
There's a lot of misinformation about "natural" ways to build immunity against allergies. While some lifestyle changes can support overall health and potentially reduce the severity of allergic reactions, there's no scientific evidence to support the idea that natural remedies can build immunity against specific allergens. Practices like probiotics, vitamin supplements, or herbal remedies might offer some general health benefits and may help manage certain symptoms, but they don't address the underlying immune response that causes allergies. Some studies suggest a link between diet and allergy development, with some evidence indicating that a balanced diet might help reduce the risk of developing allergies or decrease symptom severity. However, this is a complex area of research with no clear-cut answers. Always consult with a healthcare professional before making significant dietary or lifestyle changes, particularly if you have allergies.
Deja una respuesta