Do allergies ever end

Allergies can be a disruptive force in our lives, causing discomfort and inconvenience with their itchy eyes, runny noses, and difficulty breathing. But do these allergies ever come to an end? Can we ever hope to live a life free from their grasp? This article will delve into the complexities of allergies, exploring whether they can truly disappear or if they are destined to stay with us forever.
Do Allergies Ever Really Go Away?
The simple answer is: it depends. While some allergies may lessen in severity or even disappear over time, others can persist throughout a person's life. There's no guaranteed cure for allergies, but understanding the different factors influencing their duration can provide valuable insight and management strategies. The journey with allergies is unique to each individual, with several contributing factors influencing their longevity and intensity.
What Causes Allergies to Develop?
Allergies develop when your immune system mistakenly identifies a harmless substance (allergen) as a threat. This leads to the production of immunoglobulin E (IgE) antibodies. Upon subsequent exposure to the allergen, these antibodies trigger a cascade of reactions, releasing histamine and other chemicals that cause allergy symptoms. The specific allergen causing the allergy, the individual's genetic predisposition, and environmental exposures are key factors determining the likelihood of an allergy developing and persisting.
Can Allergies Disappear in Childhood?
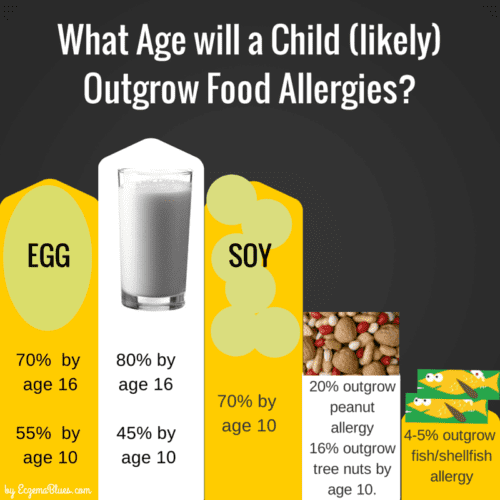
Some allergies, particularly those to milk, soy, wheat, and eggs, often improve or even resolve during childhood. This is because the immune system matures and becomes less reactive to these allergens. However, this isn't always the case, and some children may continue to experience allergies into adulthood. Early identification and appropriate management strategies are crucial. It's important to note that outgrowing one allergy doesn't guarantee immunity to developing others later in life.
Do Allergies Get Worse with Age?
While some allergies may improve with age, others, especially those related to seasonal allergens (pollen) or dust mites, can worsen. Changes in the immune system and environmental factors contribute to this. For example, increased exposure to various environmental triggers throughout one's life may lead to a higher risk of developing new allergies or seeing a worsening of existing ones. Maintaining a healthy lifestyle and adopting proactive allergy management strategies are essential as you age.
What Role Does Genetics Play?
Genetics play a significant role in the development and persistence of allergies. A family history of allergies increases the likelihood of developing allergies yourself. Genetic predisposition does not guarantee an allergy will develop, but it significantly increases the probability. Understanding your family history can help predict your allergy risk and allow for early intervention and preventative measures.
How Can I Manage My Allergies?
Effective allergy management involves various approaches, depending on the specific allergens and their severity. These strategies include allergy medication (antihistamines, decongestants, corticosteroids), immunotherapy (allergy shots), and lifestyle modifications (avoiding allergens, managing indoor environments). Regular consultation with an allergist is essential for personalized management and to monitor the progression or resolution of allergies.
| Allergy Type | Likelihood of Resolution | Management Strategies |
|---|---|---|
| Food Allergies (e.g., milk, eggs) | Often improves or resolves in childhood | Avoidance, early introduction of potential allergens (with doctor supervision) |
| Seasonal Allergies (e.g., pollen) | Less likely to resolve completely | Medication, immunotherapy, environmental control |
| Dust Mite Allergy | Relatively unlikely to resolve | Encasement of mattresses and pillows, regular cleaning, air purifiers |
| Pet Allergy | Rarely resolves | Avoidance, medication, frequent cleaning |
https://youtube.com/watch?v=allergies-asthma-cause-earth-day-lbb-orig.cnn
Do Allergies Ever Really Go Away?
The simple answer is: it depends. While some allergies may lessen in severity or even disappear over time, others can persist throughout a person's life. There's no guaranteed cure for allergies, but understanding the different factors influencing their duration can provide valuable insight and management strategies. The journey with allergies is unique to each individual, with several contributing factors influencing their longevity and intensity.
What Causes Allergies to Develop?
Allergies develop when your immune system mistakenly identifies a harmless substance (allergen) as a threat. This leads to the production of immunoglobulin E (IgE) antibodies. Upon subsequent exposure to the allergen, these antibodies trigger a cascade of reactions, releasing histamine and other chemicals that cause allergy symptoms. The specific allergen causing the allergy, the individual's genetic predisposition, and environmental exposures are key factors determining the likelihood of an allergy developing and persisting.
Can Allergies Disappear in Childhood?
Some allergies, particularly those to milk, soy, wheat, and eggs, often improve or even resolve during childhood. This is because the immune system matures and becomes less reactive to these allergens. However, this isn't always the case, and some children may continue to experience allergies into adulthood. Early identification and appropriate management strategies are crucial. It's important to note that outgrowing one allergy doesn't guarantee immunity to developing others later in life.
Do Allergies Get Worse with Age?
While some allergies may improve with age, others, especially those related to seasonal allergens (pollen) or dust mites, can worsen. Changes in the immune system and environmental factors contribute to this. For example, increased exposure to various environmental triggers throughout one's life may lead to a higher risk of developing new allergies or seeing a worsening of existing ones. Maintaining a healthy lifestyle and adopting proactive allergy management strategies are essential as you age.
What Role Does Genetics Play?
Genetics play a significant role in the development and persistence of allergies. A family history of allergies increases the likelihood of developing allergies yourself. Genetic predisposition does not guarantee an allergy will develop, but it significantly increases the probability. Understanding your family history can help predict your allergy risk and allow for early intervention and preventative measures.
How Can I Manage My Allergies?
Effective allergy management involves various approaches, depending on the specific allergens and their severity. These strategies include allergy medication (antihistamines, decongestants, corticosteroids), immunotherapy (allergy shots), and lifestyle modifications (avoiding allergens, managing indoor environments). Regular consultation with an allergist is essential for personalized management and to monitor the progression or resolution of allergies.
| Allergy Type | Likelihood of Resolution | Management Strategies |
|---|---|---|
| Food Allergies (e.g., milk, eggs) | Often improves or resolves in childhood | Avoidance, early introduction of potential allergens (with doctor supervision) |
| Seasonal Allergies (e.g., pollen) | Less likely to resolve completely | Medication, immunotherapy, environmental control |
| Dust Mite Allergy | Relatively unlikely to resolve | Encasement of mattresses and pillows, regular cleaning, air purifiers |
| Pet Allergy | Rarely resolves | Avoidance, medication, frequent cleaning |
Will my allergies ever go away?
:max_bytes(150000):strip_icc()/VWH_Illustration_Preventing-and-Treating-Seasonal-Allergies_Danie-Drankwalter_Final-884166d09ac94425ad7e7a3b68a14249.jpg)
Will My Allergies Ever Go Away?
Whether your allergies will ever go away is a complex question with no single answer. It depends on several factors, including the type of allergy, your age, and the severity of your symptoms. Some allergies, particularly those developed in childhood, may lessen or even disappear over time. This is more common with allergies to things like milk, eggs, soy, or wheat. However, other allergies, such as those to pollen, pet dander, or dust mites, are more likely to persist throughout your life. The severity of your symptoms can also fluctuate; you might experience more intense reactions during certain seasons or periods of high exposure. In some cases, allergy symptoms might spontaneously decrease, but this isn't predictable, and there's no guarantee.
Types of Allergies and Their Likelihood of Resolution
The type of allergen plays a significant role in determining the long-term prognosis of your allergies. Food allergies, especially those that appear early in childhood, sometimes resolve themselves as the immune system matures. On the other hand, respiratory allergies (pollen, dust mites, pet dander) tend to be more persistent. Environmental allergies are often lifelong, requiring ongoing management strategies. It's important to note that even if a food allergy resolves, a person might still develop an allergy to a different food later in life.
- Food Allergies: Often improve or disappear by adulthood, particularly milk, egg, soy, and wheat allergies.
- Respiratory Allergies: Usually lifelong, requiring ongoing management with medication or immunotherapy.
- Environmental Allergies: Typically persistent, necessitating avoidance and/or treatment strategies.
Age and Allergy Development
The age at which you developed your allergies can influence their longevity. Allergies appearing in early childhood sometimes improve or disappear with age. This is because the immune system is still developing and maturing during childhood. Allergies developed in adulthood are less likely to spontaneously resolve. While some improvement is possible, complete resolution is less common.
- Childhood Allergies: Higher chance of resolution as the immune system develops.
- Adult-Onset Allergies: Lower chance of spontaneous resolution, often requiring long-term management.
- Immune System Maturity: Plays a crucial role in the potential resolution of allergies.
Severity of Allergic Reactions
The intensity of your allergic reactions does not necessarily predict whether the allergy will disappear. Even mild allergies can persist throughout life, whereas severe allergies might not always resolve. However, the severity of symptoms can fluctuate, sometimes lessening over time. While a severe reaction requires immediate attention, the long-term outlook regarding allergy resolution doesn't directly correlate with the severity of the reaction.
- Mild Allergies: Can still be lifelong, even if symptoms are manageable.
- Severe Allergies: Require immediate medical attention, but the likelihood of resolution remains unpredictable.
- Fluctuation in Severity: Symptom intensity can change over time, regardless of the allergy's overall persistence.
Treatment Options and Their Impact
Allergy treatments like immunotherapy can sometimes help reduce allergy symptoms over time, and in rare cases, might lead to the complete resolution of an allergy. However, immunotherapy is not a guaranteed cure. Medication such as antihistamines, decongestants, and nasal corticosteroids can effectively manage symptoms, but they don't typically eliminate the allergy itself. These treatments provide relief, improving the quality of life, rather than a potential cure for your allergy.
- Immunotherapy: Can reduce symptom severity and, in some cases, lead to long-term remission.
- Medication: Manages symptoms effectively but usually does not cure the allergy.
- Avoidance Strategies: Helpful in reducing exposure and alleviating symptoms but doesn’t resolve the underlying allergy.
Will allergies ever be cured?

Whether allergies will ever be completely cured is a complex question with no definitive answer. Current medical understanding suggests a complete cure is unlikely in the foreseeable future, but significant advancements are being made in managing and potentially mitigating allergic reactions. The development of a universal cure would require a deep understanding and manipulation of the intricate immune system responses that trigger allergic reactions, a feat that remains exceptionally challenging. Research is focusing on several promising avenues, including immunotherapy, genetic engineering, and the development of novel drugs targeting specific pathways in the allergic response. While a complete eradication of allergies might be a distant goal, substantial improvements in managing and preventing allergic symptoms are achievable and constantly being refined.
Current Treatments and Their Limitations
Current allergy treatments primarily focus on managing symptoms and preventing allergic reactions rather than providing a cure. These treatments include antihistamines, decongestants, corticosteroids, and immunotherapy. While effective in reducing symptoms for many, they have limitations. Antihistamines and decongestants only address the symptoms and don't target the root cause of the allergy. Immunotherapy, also known as allergy shots, can desensitize individuals to specific allergens, but it's a lengthy process, not effective for all allergens, and can have side effects. Furthermore, these treatments often manage symptoms, rather than offering a lasting resolution to the underlying allergic response.
- Antihistamines: Block the effects of histamine, a chemical released during an allergic reaction.
- Decongestants: Reduce nasal congestion by constricting blood vessels in the nasal passages.
- Corticosteroids: Reduce inflammation and suppress the immune system.
The Role of the Immune System in Allergies
Allergies are fundamentally driven by a malfunctioning immune system. When exposed to an allergen (like pollen, pet dander, or peanuts), the immune system mistakenly identifies it as a threat. This triggers an inappropriate immune response, leading to the release of inflammatory chemicals like histamine, causing symptoms such as sneezing, itching, and swelling. Understanding the precise mechanisms of this immune system malfunction is crucial for developing effective cures. Research focuses on identifying the specific immune cells and signaling pathways involved to design targeted therapies. The complexity of the immune system and the variability of allergic responses make it challenging to find a universal solution.
- Inappropriate IgE antibody production: The immune system produces excessive amounts of IgE antibodies that bind to allergens.
- Mast cell degranulation: Mast cells release histamine and other inflammatory mediators.
- Inflammation: Leads to the characteristic symptoms of allergic reactions.
Immunotherapy and its Potential for Long-Term Management
Immunotherapy, while not a cure, represents a significant advancement in allergy management. It aims to re-educate the immune system to tolerate allergens. This is typically done through gradually increasing exposure to the allergen, either through injections (allergy shots) or sublingual tablets (under the tongue). The goal is to shift the immune response from an IgE-mediated reaction to a more tolerant, IgG-mediated response. While effective for many, immunotherapy is not a quick fix and requires a significant time commitment. Furthermore, it's not effective for all allergens or all individuals. Research continues to improve immunotherapy protocols and expand its applicability.
- Allergy shots: Gradual increases in allergen exposure through injections.
- Sublingual immunotherapy (SLIT): Allergen exposure through tablets placed under the tongue.
- Personalized immunotherapy: Tailoring treatment to individual patients' allergies and immune responses.
Genetic Factors and Their Influence on Allergies
Genetic predisposition plays a significant role in the development of allergies. Certain genes are linked to an increased risk of developing allergies. Research is actively exploring these genetic factors to identify potential targets for therapeutic interventions. Understanding the genetic basis of allergies could pave the way for gene therapies or other approaches that modify the genetic predisposition to allergies. However, the complex interplay between genes and environmental factors makes the development of such therapies challenging.
- Identification of susceptibility genes: Pinpointing genes linked to increased allergy risk.
- Gene therapy: Exploring possibilities of correcting faulty genes contributing to allergies.
- Pharmacogenomics: Tailoring treatments based on an individual's genetic profile.
Emerging Technologies and Future Directions
Several promising avenues are being explored in allergy research. These include the development of novel drugs that target specific pathways in the allergic response, such as inhibitors of certain inflammatory molecules or molecules involved in immune cell activation. Additionally, advancements in nanotechnology and biotechnology are opening up new possibilities for targeted drug delivery and immune system modulation. The development of more precise and personalized therapies is a key goal, aiming to reduce side effects and improve treatment effectiveness. The ongoing research into the microbiome’s role in the immune system also offers potential for therapeutic development.
- Targeted drug therapies: Developing drugs that specifically target key molecules in the allergic response.
- Nanotechnology-based drug delivery: Improving drug targeting and reducing side effects.
- Biotechnology and microbiome research: Exploring new therapeutic approaches.
Is it possible to outgrow allergies?
Whether it's possible to outgrow allergies is complex and depends on several factors. While some allergies, particularly those related to food, can be outgrown, others, like allergies to pollen or animal dander, are more persistent. The age of onset, the type of allergen, and individual immune system responses all play a significant role. There's no guarantee that someone will outgrow an allergy, but it is certainly possible, particularly during childhood. The likelihood of outgrowing an allergy diminishes with age, making it less common for adults to spontaneously lose an allergy.
What Allergies Are Most Likely to Be Outgrown?
Food allergies are the most common type of allergies that children may outgrow. Milk, egg, soy, and wheat allergies are often resolved by adolescence or early adulthood. However, peanut and tree nut allergies are less likely to be outgrown. The timing of when a child develops an allergy can influence whether it will be outgrown. Early onset allergies, often appearing within the first year of life, are frequently outgrown, unlike later onset allergies.
- Milk allergy: Often disappears by school age.
- Egg allergy: Many children outgrow this by the age of 10.
- Soy and Wheat allergies: These have a relatively high outgrowing rate, though some individuals may carry them into adulthood.
What Allergies Are Less Likely to Be Outgrown?
Allergies to environmental triggers such as pollen, dust mites, pet dander, and insect stings are generally considered to be lifelong. While the severity of symptoms might fluctuate, the underlying allergic sensitivity typically persists. These allergies frequently involve immunoglobulin E (IgE) antibodies which tend to be long-lasting. Even with successful immunotherapy, the allergy is not entirely eradicated. It’s vital to maintain allergy management strategies to mitigate symptoms.
- Pollen allergies: Highly unlikely to be outgrown.
- Dust mite allergies: Usually persistent throughout life.
- Pet dander allergies: Rarely disappear completely.
Factors Affecting the Likelihood of Outgrowing Allergies
Several factors contribute to whether an allergy will be outgrown. Age of onset is crucial; allergies that develop earlier in life have a greater potential to be outgrown. The specific allergen plays a major role; some allergens are more likely to induce tolerance over time than others. Finally, individual immune system variations determine how the body reacts to allergens. Some individuals naturally develop tolerance, while others remain sensitive throughout their lives.
- Early onset allergies: Higher likelihood of resolution.
- Genetic predisposition: Family history of allergies can influence the likelihood of outgrowing them.
- Immune system maturity: The immune system's development and adaptation affect allergy progression.
The Role of the Immune System in Outgrowing Allergies
The immune system's response to allergens is central to the possibility of outgrowing an allergy. The process of outgrowing an allergy often involves a shift in the immune response. The body may develop tolerance, meaning the immune system becomes less reactive to the allergen, resulting in a decrease or disappearance of symptoms. This is not necessarily a complete elimination of sensitivity, but a change in reaction threshold. Other factors, like gut microbiome diversity may also play a role in allergy development and resolution, but more research is needed in this area.
- Tolerance development: The immune system learns to ignore the allergen.
- Immune regulation: Shift in the balance of immune cells and mediators.
- Changes in antibody production: Reduction in IgE antibody levels.
Medical Interventions and Outgrowing Allergies
While spontaneous outgrowing is possible, medical interventions such as immunotherapy (allergy shots or sublingual immunotherapy) can help desensitize the body to specific allergens. Though these therapies don't guarantee an individual will completely outgrow their allergy, they can significantly reduce symptom severity and improve quality of life. These are not methods of "outgrowing" as such, but effective management strategies. Regular medical check-ups and monitoring are essential.
- Immunotherapy: Allergy shots or sublingual tablets can gradually reduce allergic reactions.
- Medication management: Antihistamines, corticosteroids, and other medications can control symptoms.
- Lifestyle adjustments: Avoiding allergens whenever possible is crucial for symptom control.
What's the longest allergies can last?
The duration of allergies can vary greatly depending on the allergen, the individual's sensitivity, and the type of allergic reaction. There's no single definitive answer to "how long allergies can last," as some might only last a few hours while others can persist for months or even, in some chronic cases, a lifetime. However, it's important to differentiate between the acute symptoms of an allergic reaction and the underlying allergic condition itself.
Seasonal Allergies: Duration and Symptoms
Seasonal allergies, also known as hay fever, are typically triggered by pollen from plants like trees, grasses, and weeds. These allergies usually last for the pollen season, which can span several months depending on the geographic location and specific allergens. Symptoms like sneezing, runny nose, itchy eyes, and congestion can come and go within a day, but the overall allergy season lasts longer. The duration depends heavily on the environmental factors such as weather and the specific pollen count for the region.
- Peak season: This period sees the highest pollen concentration and consequently, the most intense allergy symptoms. This can last several weeks.
- Gradual onset and offset: The onset and the decline in symptoms are usually gradual, meaning the severity of the allergy increases and decreases progressively, rather than abruptly.
- Regional variations: The length of the pollen season varies significantly across different regions and microclimates.
Chronic Allergies: Persistent Symptoms
Chronic allergies, such as those to dust mites, pet dander, or certain foods, can persist year-round. While the severity of symptoms might fluctuate, the underlying allergic condition remains. These allergies are considered long-lasting, sometimes persisting throughout a person's life if not managed effectively. The key is recognizing triggers and implementing avoidance strategies and/or medical interventions.
- Consistent exposure: Continuous exposure to the allergen is a key factor determining the duration of symptoms. Removing or reducing exposure can lessen severity.
- Symptom management: Treatment like medication, immunotherapy, or environmental control can help manage symptoms, but the allergy itself remains.
- Underlying condition: This type of allergy is not a temporary condition; it's a persistent immune response to a specific antigen.
Allergic Reactions: Acute vs. Prolonged
It's crucial to distinguish between an acute allergic reaction (like anaphylaxis) and the duration of an allergy itself. Anaphylaxis is a severe, life-threatening reaction that requires immediate medical attention, and its symptoms can last for varying periods of time depending on the severity and treatment received. This is different from the overall time frame of the allergic condition.
- Immediate reaction: Anaphylaxis can manifest within minutes of exposure to the allergen.
- Treatment duration: Treatment such as epinephrine and other interventions dictates the length of acute symptoms.
- Long-term effects: Even after acute symptoms subside, there might be lingering effects such as fatigue or organ damage in severe cases.
Contact Dermatitis: Duration and Treatment
Contact dermatitis is an allergic reaction to substances that come into contact with the skin. The duration depends heavily on the allergen and the extent of exposure. Symptoms can range from a few days to several weeks, depending on the severity of the reaction and the effectiveness of treatment. Avoiding contact with the triggering substance is crucial, and topical treatments such as corticosteroids often alleviate symptoms.
- Severity of reaction: Mild reactions may resolve quickly with simple treatment, while severe reactions might require more extensive care.
- Allergen avoidance: Removing the allergen is paramount for healing and preventing recurrence.
- Treatment response: The response to treatment significantly influences the length of time symptoms persist.
Medication and Allergy Duration
While medication doesn't cure allergies, it can significantly affect the duration and severity of symptoms. Antihistamines can provide immediate relief, but their effect is typically temporary, lasting only as long as the medication is active in the body. Other medications like corticosteroids or immunotherapy offer longer-term management options but don't inherently shorten the duration of the underlying allergic condition itself. The duration of the allergy is still determined by exposure and the nature of the allergy itself.
- Medication type: Different medications offer varying durations of relief; some provide short-term symptom control, others longer-term management.
- Dosage and frequency: The effectiveness of medication depends on proper dosage and adherence to the prescribed schedule.
- Individual response: The response to medication can vary considerably between individuals, affecting the perceived duration of allergy symptoms.
Do allergies ever completely disappear?
While it's not common for allergies to completely vanish, it's certainly possible, though the likelihood depends on several factors. Childhood allergies, especially those to milk, eggs, soy, wheat, or peanuts, often lessen in severity or even disappear entirely by adulthood. This is thought to be due to the body's immune system maturing and adapting. However, it's crucial to understand that this isn't a guaranteed outcome. Some individuals will experience these allergies throughout their lives, even if the severity fluctuates. Environmental allergies, such as pollen or pet dander, can also change over time. If your exposure to the allergen decreases significantly, your symptoms might lessen or disappear. For example, moving to a region with less pollen might dramatically improve your seasonal allergies. It’s also important to consider that while symptoms might decrease, the underlying allergy might not have disappeared completely. A seemingly resolved allergy could resurface if you're re-exposed to the allergen at a sufficient level, particularly in cases of severe allergies. Therefore, even if you experience long periods of remission, it’s best to remain cautious and avoid potential triggers. It's always advisable to consult an allergist to understand your specific situation and potential management strategies.
Can I outgrow my allergies?
The possibility of "outgrowing" allergies depends largely on the type of allergy. As mentioned before, some food allergies, particularly those that manifest in early childhood, are more likely to lessen or resolve themselves as a person ages. The immune system develops and matures, potentially developing a higher tolerance to the previously allergenic substance. However, this is not a universal experience. Some individuals retain their food allergies throughout their lives. For allergies to environmental triggers like pollen, dust mites, or pet dander, the chance of "outgrowing" them is less likely. While symptoms might lessen with reduced exposure or changes in environmental factors, the underlying allergy often remains. These allergies are typically less influenced by immune system maturation and more dependent on continued exposure. It's also worth noting that the term "outgrowing" can be misleading. It's more accurate to say that symptoms can lessen or disappear due to several factors. The allergy itself may persist, though possibly in a less severe form, potentially resurfacing with increased exposure. Consulting an allergist is always the best course of action to understand your specific situation and receive personalized advice.
What factors influence whether allergies will end?
Several factors influence whether allergies will diminish or disappear over time. The type of allergen plays a significant role. Food allergies are more likely to improve or resolve in childhood, whereas environmental allergies tend to persist. Genetics also plays a part. If you have a family history of persistent allergies, you're more likely to experience them throughout your life. Exposure level is another critical factor. Reduced or limited exposure to allergens can significantly alleviate symptoms and may even lead to a lessening of the allergic response over time. The age of onset is also relevant; allergies appearing later in life are less likely to resolve spontaneously compared to those developed in childhood. Lastly, the individual's immune system response plays a major role. The body's ability to adapt and tolerate allergens can differ considerably between individuals. Some people's immune systems might develop a tolerance over time, while others continue to show a strong reaction. Regular check-ups with an allergist, coupled with careful monitoring of symptoms, are important for managing allergies and understanding individual responses.
Are there treatments that can help allergies end?
While there's no guaranteed "cure" to make allergies completely disappear, various treatments can significantly reduce symptoms and, in some cases, lead to long-term improvement or even remission. Immunotherapy, also known as allergy shots or sublingual immunotherapy (SLIT), is a common treatment that aims to desensitize the immune system to specific allergens. Over time, this can lead to a reduced allergic response, often resulting in lessened symptoms or even a complete absence of symptoms for some individuals. However, it's a long-term commitment, requiring regular injections or drops over several years. Medication, such as antihistamines, decongestants, and nasal corticosteroids, effectively manage allergy symptoms, providing relief during allergy seasons or exposure to allergens. While they don't cure the allergy, they make it manageable. Lifestyle modifications are also crucial. Avoiding triggers as much as possible can drastically reduce symptom severity. This includes things like using air purifiers, maintaining a clean home, avoiding certain foods, and washing bedding regularly. While these treatments don't guarantee the complete elimination of allergies, they offer effective strategies to manage symptoms and potentially lead to long-term improvement or even remission in some cases. Consulting with an allergist is essential to determine the best treatment plan based on individual needs and allergy type.

Deja una respuesta