Does allergies mean weak immune system
Allergies are a common problem, affecting millions of people around the world. They can cause a variety of symptoms, from sneezing and runny nose to more severe reactions such as asthma and anaphylaxis. Many people believe that allergies are a sign of a weak immune system, but is this really the case?
Do Allergies Indicate a Weak Immune System?
The relationship between allergies and a weak immune system is complex and not straightforward. While it might seem counterintuitive that a system designed to protect you would cause such reactions, the reality is more nuanced. Allergies aren't a sign of a weak immune system, but rather a case of an overactive one. A healthy immune system identifies and neutralizes threats like bacteria and viruses. However, in individuals with allergies, the immune system mistakenly identifies harmless substances, called allergens (like pollen, pet dander, or certain foods), as dangerous invaders.
What is an Allergic Reaction?
An allergic reaction occurs when the immune system's B cells produce a type of antibody called immunoglobulin E (IgE) in response to an allergen. These IgE antibodies attach to mast cells and basophils, which are cells found in your tissues and blood. Upon subsequent exposure to the same allergen, the IgE antibodies trigger the release of histamine and other inflammatory chemicals from these cells. This release leads to the characteristic symptoms of an allergic reaction, such as sneezing, itching, rash, and in severe cases, anaphylaxis.
The Role of Immune System Cells in Allergies
Several immune cells play a role in allergic reactions. Mast cells and basophils are key players, releasing histamine and other inflammatory mediators. T helper cells, specifically the Th2 subtype, are also crucial in driving the allergic response by producing cytokines that promote IgE production. While the immune system is actively responding, it's doing so in a way that's overly aggressive and inappropriate to the threat.
The Difference Between an Allergic Response and an Immune Deficiency
It's important to distinguish between an allergic response and an immune deficiency. Immune deficiencies result from a weakened or compromised immune system, leaving individuals vulnerable to infections. Allergies, on the other hand, involve an overly reactive immune system that responds excessively to harmless substances. They are not indicative of a weakened ability to fight off actual pathogens.
Can Allergies Co-exist with other Immune Issues?
Yes, it's possible to have allergies and other immune issues concurrently. For example, some individuals may experience allergies alongside autoimmune diseases, where the immune system attacks the body's own tissues. This doesn't mean the allergies are causing the autoimmune disease, or vice-versa, but it highlights the complexity of the immune system and the potential for multiple dysregulations to occur simultaneously. Careful diagnosis is needed to determine the specific condition(s).
Genetic Predisposition and Environmental Factors
The development of allergies is often influenced by a combination of genetic predisposition and environmental factors. A family history of allergies increases the likelihood of developing them, but environmental exposures, such as exposure to pollutants or certain foods during early childhood, can also play a significant role. This interaction between genes and environment underscores the intricate nature of the immune system's response to allergens.
| Feature | Allergic Response | Immune Deficiency |
|---|---|---|
| Immune System State | Overactive | Weakened |
| Target | Harmless substances (allergens) | Pathogens (bacteria, viruses, etc.) |
| Symptoms | Sneezing, itching, rash, anaphylaxis | Increased susceptibility to infections |
| Treatment | Allergy medication, immunotherapy | Immunotherapy, antibiotics (for infections) |
Do Allergies Indicate a Weak Immune System?
The relationship between allergies and a weak immune system is complex and not straightforward. While it might seem counterintuitive that a system designed to protect you would cause such reactions, the reality is more nuanced. Allergies aren't a sign of a weak immune system, but rather a case of an overactive one. A healthy immune system identifies and neutralizes threats like bacteria and viruses. However, in individuals with allergies, the immune system mistakenly identifies harmless substances, called allergens (like pollen, pet dander, or certain foods), as dangerous invaders.
What is an Allergic Reaction?
An allergic reaction occurs when the immune system's B cells produce a type of antibody called immunoglobulin E (IgE) in response to an allergen. These IgE antibodies attach to mast cells and basophils, which are cells found in your tissues and blood. Upon subsequent exposure to the same allergen, the IgE antibodies trigger the release of histamine and other inflammatory chemicals from these cells. This release leads to the characteristic symptoms of an allergic reaction, such as sneezing, itching, rash, and in severe cases, anaphylaxis.
The Role of Immune System Cells in Allergies
Several immune cells play a role in allergic reactions. Mast cells and basophils are key players, releasing histamine and other inflammatory mediators. T helper cells, specifically the Th2 subtype, are also crucial in driving the allergic response by producing cytokines that promote IgE production. While the immune system is actively responding, it's doing so in a way that's overly aggressive and inappropriate to the threat.
The Difference Between an Allergic Response and an Immune Deficiency
It's important to distinguish between an allergic response and an immune deficiency. Immune deficiencies result from a weakened or compromised immune system, leaving individuals vulnerable to infections. Allergies, on the other hand, involve an overly reactive immune system that responds excessively to harmless substances. They are not indicative of a weakened ability to fight off actual pathogens.
Can Allergies Co-exist with other Immune Issues?
Yes, it's possible to have allergies and other immune issues concurrently. For example, some individuals may experience allergies alongside autoimmune diseases, where the immune system attacks the body's own tissues. This doesn't mean the allergies are causing the autoimmune disease, or vice-versa, but it highlights the complexity of the immune system and the potential for multiple dysregulations to occur simultaneously. Careful diagnosis is needed to determine the specific condition(s).
Genetic Predisposition and Environmental Factors
The development of allergies is often influenced by a combination of genetic predisposition and environmental factors. A family history of allergies increases the likelihood of developing them, but environmental exposures, such as exposure to pollutants or certain foods during early childhood, can also play a significant role. This interaction between genes and environment underscores the intricate nature of the immune system's response to allergens.
| Feature | Allergic Response | Immune Deficiency |
|---|---|---|
| Immune System State | Overactive | Weakened |
| Target | Harmless substances (allergens) | Pathogens (bacteria, viruses, etc.) |
| Symptoms | Sneezing, itching, rash, anaphylaxis | Increased susceptibility to infections |
| Treatment | Allergy medication, immunotherapy | Immunotherapy, antibiotics (for infections) |
Is your immune system weak if you have allergies?

No, having allergies doesn't necessarily mean you have a weak immune system. In fact, it's quite the opposite. Allergies are a sign of an overactive, not a weak, immune system. Your immune system is designed to protect you from harmful substances like bacteria and viruses. In people with allergies, the immune system mistakenly identifies harmless substances, such as pollen, pet dander, or certain foods, as dangerous invaders. This triggers an immune response that's excessive and inappropriate, leading to allergy symptoms like sneezing, itching, and rashes. A truly weak immune system would be less likely to mount such a robust (though misguided) response.
The Role of IgE Antibodies in Allergies
Allergies are largely mediated by a type of antibody called IgE. When a person with an allergy is exposed to an allergen, their immune system produces IgE antibodies that bind to mast cells and basophils. Upon subsequent exposure to the allergen, these antibodies trigger the release of histamine and other inflammatory mediators, causing allergic symptoms. This strong, specific immune response, although inappropriately targeted, highlights the immune system's activity, not weakness.
- IgE antibodies are key players in allergic reactions.
- Mast cells and basophils release histamine and other inflammatory mediators.
- This process showcases an active, albeit misguided immune response.
The Difference Between a Weak Immune System and Allergies
A weak immune system is characterized by an inability to effectively fight off infections. People with weakened immune systems are more susceptible to frequent and severe infections. Allergies, on the other hand, are characterized by an overreaction to harmless substances, not an inability to fight off infections. The immune system is functioning, but it’s targeting the wrong things.
- Weakened immune systems struggle to fight infections.
- Allergies involve an overreaction to harmless substances.
- These conditions stem from distinct mechanisms within the immune system.
The Genetics of Allergies
A predisposition to allergies often has a genetic component, meaning it can run in families. This doesn't necessarily imply a generally weaker immune system. Instead, it suggests a genetic tendency towards an overactive immune response to certain types of allergens. Specific genes can influence the production of IgE antibodies and the sensitivity of mast cells, leading to a higher likelihood of developing allergies.
- Genetic factors play a role in allergy susceptibility.
- Genes may influence IgE production and mast cell activity.
- This doesn't signify an overall weaker immune response, but rather a different pattern of immune response.
Co-occurrence of Allergies and Other Immune Conditions
It's true that some individuals may experience both allergies and other immune-related conditions like asthma or eczema. This co-occurrence doesn't automatically imply a weak immune system. Instead, it suggests a complex interplay of immune responses, where an overactive response in one area (allergies) may interact with or influence other aspects of the immune system.
- Allergies can co-occur with other conditions like asthma or eczema.
- This reflects complex immune system interactions, not necessarily a generalized immune deficiency.
- The immune response is dysregulated rather than weakened.
Are you weak if you have allergies?
No, having allergies does not inherently make you weak. While allergies can cause a variety of symptoms that may lead to feeling unwell, allergies themselves are not a marker of overall physical weakness or frailty. The severity of allergic reactions varies greatly from person to person, and the impact on daily life also depends on individual factors and the type of allergy.
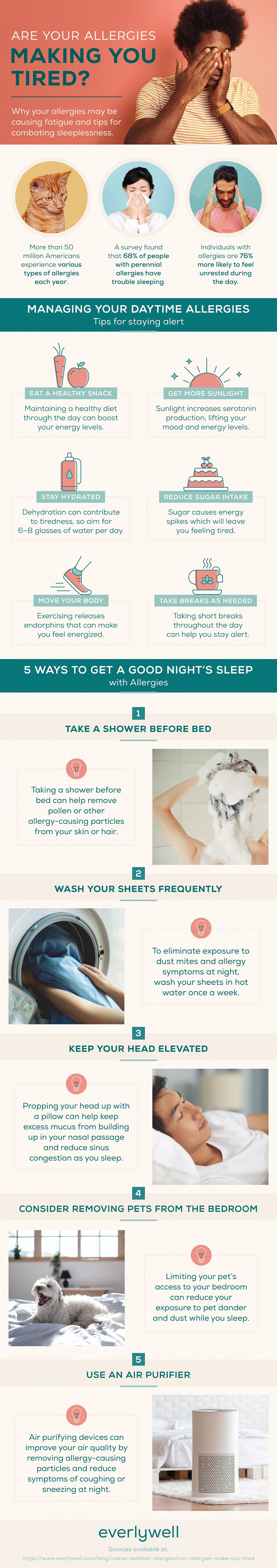
Allergies and Energy Levels
Many people with allergies experience fatigue as a symptom. This can stem from various factors: poor sleep due to nighttime allergies, inflammation throughout the body, or the need to constantly manage allergy symptoms. However, fatigue is a symptom, not a measure of underlying strength or weakness. It's important to differentiate between feeling tired due to allergies versus a broader health concern.
- Poor sleep: Nasal congestion, coughing, and sneezing can disrupt sleep patterns, leading to daytime fatigue.
- Inflammation: Allergic reactions trigger inflammation, which can drain energy.
- Medication side effects: Some allergy medications can cause drowsiness.
Allergies and Immune System Function
It's a common misconception that having allergies means a weak immune system. Allergies are actually a sign of an overactiveimmune system. The immune system is mistakenly identifying harmless substances (allergens) as threats, triggering an inappropriate response. This overreaction can lead to symptoms, but it doesn't signify a weaker immune system overall. A truly weak immune system would struggle to fight off infections, while allergies involve a specific type of immune response.
- Misdirected response: The immune system overreacts to harmless substances.
- Not a sign of general weakness: Allergies are a specific immune dysfunction, not a sign of overall immune deficiency.
- Other functions unaffected: A person with allergies can still fight off infections effectively.
The Impact of Severe Allergic Reactions
While most allergy symptoms are manageable, severe allergic reactions, like anaphylaxis, are a serious concern. Anaphylaxis is a life-threatening emergency that requires immediate medical attention. During an anaphylactic reaction, a person might experience a significant drop in blood pressure and difficulty breathing, making them feel very unwell. However, even after recovering from anaphylaxis, this doesn't equate to underlying weakness; rather, it highlights the need for careful allergy management.
- Anaphylaxis: A severe and potentially life-threatening allergic reaction.
- Medical emergency: Requires immediate treatment to prevent death.
- Recovery: Recovery from anaphylaxis doesn't imply general physical weakness.
Managing Allergies and Maintaining Strength
Proper allergy management can significantly improve quality of life. This includes strategies like allergen avoidance, medication, and immunotherapy. Active management is key to maintaining overall health and strength. By addressing allergy symptoms effectively, individuals can minimize their impact on daily life and energy levels.
- Allergen avoidance: Reducing exposure to triggers.
- Medication: Using appropriate medications to manage symptoms.
- Immunotherapy: Desensitization treatments to build tolerance.
Allergies and Physical Activity
Allergies may temporarily impact your ability to exercise due to symptoms like shortness of breath or fatigue. However, regular physical activity is actually beneficial for overall health, even with allergies. Listen to your body, adjust exercise intensity as needed during allergy flares, and ensure you are managing your allergies effectively. Exercise can improve energy levels and overall wellbeing despite allergies.
- Exercise benefits: Improves mood, boosts energy, strengthens the body.
- Adjusting intensity: Reduce intensity during allergy flares.
- Allergy management: Effective allergy management makes exercise easier.
Can you build immunity against allergies?

No, you cannot build immunity against allergies in the same way you build immunity against infectious diseases like measles or chickenpox. While the immune system's response to allergens is complex and involves various factors, it's fundamentally different from the response to pathogens. In infectious disease, the goal of the immune system is to eliminate the pathogen. With allergies, the immune system mistakenly identifies a harmless substance (allergen) as a threat and overreacts, triggering an inflammatory response. This response doesn't lead to eradication of the allergen but rather to the symptoms we associate with allergic reactions.
What is an Allergy?
An allergy is an immune system response to a typically harmless substance (allergen) such as pollen, pet dander, or certain foods. The body identifies these allergens as dangerous, triggering an immune response. This response involves the production of IgE antibodies, which bind to mast cells and basophils. When exposed to the allergen again, these cells release histamine and other inflammatory mediators, causing symptoms like sneezing, itching, rash, or difficulty breathing.
- IgE antibodies are key players in allergic reactions.
- Histamine release leads to the characteristic allergy symptoms.
- Allergens are usually harmless substances that trigger an inappropriate immune response.
Immune Tolerance and Allergies
The concept of immune tolerance involves the ability of the immune system to differentiate between self and non-self, and to not react against harmless substances. In allergies, this tolerance mechanism fails. The immune system mistakenly classifies harmless substances as threats, leading to an exaggerated immune response. While some research explores ways to induce immune tolerance, it's not a simple matter of “building immunity.” Instead, the focus is on modifying the immune response to reduce the allergic reaction.
- Immune tolerance is the failure of the immune system to recognize harmless substances as such.
- Research focuses on modifying the immune response rather than building immunity.
- There is no "building immunity" in the sense of acquiring immunity to an allergen.
Allergy Treatments and Desensitization
Current allergy treatments aim to manage symptoms or reduce the severity of allergic reactions. This often involves medications like antihistamines or corticosteroids. Immunotherapy, also known as allergy shots, is a form of desensitization where gradually increasing doses of the allergen are administered to modify the immune response over time. This doesn't necessarily create true immunity, but rather aims to reduce the severity of the reaction.
- Medications manage symptoms, but don't eliminate the allergy.
- Immunotherapy (allergy shots) aim to reduce the severity of allergic reactions.
- Desensitization is a process aimed at reducing the strength of allergic reactions.
Genetic Predisposition to Allergies
A significant factor in developing allergies is genetics. Individuals with a family history of allergies are at increased risk of developing allergies themselves. This highlights the complexity of the immune system's response and the influence of genetic factors on the development of allergic diseases. While you can't change your genes, understanding family history can help identify risk factors and guide preventative measures.
- Family history is a strong predictor of allergy development.
- Genetic factors play a crucial role in allergic responses.
- Understanding genetics can help in risk assessment and prevention.
Environmental Factors and Allergies
Environmental factors also play a role in the development and severity of allergies. Exposure to certain pollutants, allergens, or even changes in the microbiome can influence the immune system's response. While you cannot directly "build immunity," managing environmental exposures can help minimize the chance of developing an allergic reaction or lessen the severity of symptoms.
- Environmental exposure is a significant factor in allergy development.
- Pollutants and allergens can trigger or worsen allergic reactions.
- Environmental management can help in reducing allergy symptoms.
What deficiency causes allergies?

What Deficiency Causes Allergies?
There isn't one single deficiency that directly causesallergies. Allergies are a complex interplay of genetic predisposition and environmental factors. However, several deficiencies can exacerbate allergic reactions or increase susceptibility to developing them. It's more accurate to say that certain deficiencies weaken the body's ability to regulate immune responses, making it more likely to overreact to harmless substances (allergens).
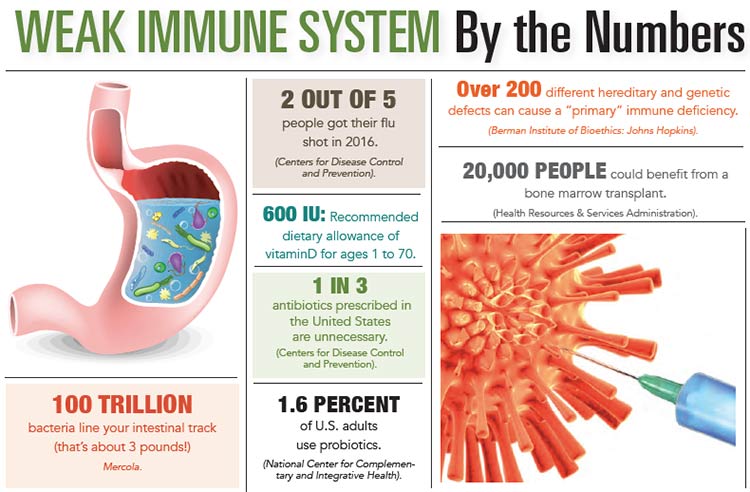
Vitamin D Deficiency and Allergies
Vitamin D plays a crucial role in immune regulation. A deficiency can lead to an imbalance in immune cells, potentially increasing the risk of allergic diseases like asthma and eczema. Sufficient vitamin D helps maintain a healthy balance of T helper cells (Th1 and Th2), preventing an overactive Th2 response—the type associated with allergies.
- Reduced immune regulation: Vitamin D deficiency disrupts the balance of immune cells, leading to exaggerated immune responses.
- Increased Th2 cell activity: A deficiency can contribute to an overproduction of Th2 cells, which are key players in allergic reactions.
- Weakened epithelial barrier: Vitamin D plays a role in maintaining the integrity of the skin and mucous membranes, which are the first lines of defense against allergens. A deficiency can weaken this barrier.
Omega-3 Fatty Acid Deficiency and Allergies
Omega-3 fatty acids, particularly EPA and DHA, possess anti-inflammatory properties. A deficiency can lead to a heightened inflammatory response, making individuals more susceptible to allergic reactions. These fatty acids help to regulate immune cell function and reduce the production of inflammatory mediators involved in allergy development.
- Increased inflammation: Omega-3 deficiency promotes inflammation, worsening allergic symptoms.
- Impaired immune cell function: Lack of omega-3s can negatively impact the function of immune cells involved in regulating allergic responses.
- Elevated levels of inflammatory markers: Deficiency can result in higher levels of inflammatory molecules, contributing to allergy severity.
Gut Microbiome Imbalance and Allergies
The gut microbiome plays a vital role in immune development and function. An imbalance in gut bacteria (dysbiosis) has been linked to an increased risk of allergies. A healthy gut microbiome helps train the immune system to distinguish between harmless and harmful substances. A disrupted microbiome can impair this process, leading to an increased likelihood of allergic responses.
- Altered immune development: A dysbiotic gut can negatively affect the maturation of the immune system, increasing allergy susceptibility.
- Increased intestinal permeability: Gut dysbiosis can lead to "leaky gut," allowing allergens to enter the bloodstream and trigger immune responses.
- Reduced production of anti-inflammatory compounds: Beneficial gut bacteria produce compounds that suppress inflammation; their absence can exacerbate allergies.
Magnesium Deficiency and Allergies
Magnesium is involved in numerous cellular processes, including immune regulation. A deficiency may weaken immune responses, potentially contributing to allergies. Magnesium helps to modulate inflammation and support the balance of immune cells, impacting the body’s reaction to allergens.
- Impaired immune cell function: Magnesium is essential for the proper function of immune cells, and deficiency can impair their ability to control allergic responses.
- Increased inflammation: A lack of magnesium can contribute to heightened inflammatory processes, exacerbating allergy symptoms.
- Reduced histamine regulation: Magnesium plays a role in managing histamine release, a key mediator in allergic reactions. Deficiency can lead to excessive histamine release.
Zinc Deficiency and Allergies
Zinc is vital for immune cell function and wound healing. Deficiency can impair immune response, making individuals more vulnerable to infections and possibly contributing to increased allergic reactions. Zinc helps regulate immune cell activity and production of inflammatory cytokines, potentially influencing the severity of allergic symptoms.
- Weakened immune function: Zinc deficiency compromises the immune system's ability to respond effectively to allergens.
- Impaired T-cell function: T-cells are crucial for immune regulation, and zinc deficiency impairs their activity.
- Increased susceptibility to infections: A weaker immune system due to zinc deficiency may also worsen allergic symptoms as the body is busy combating infections.
Does having allergies mean I have a weak immune system?
This is a common misconception. While it might seem counterintuitive that a system designed to protect you would cause such reactions, allergies aren't actually a sign of a weak immune system. Instead, allergies are a result of an overactive immune system. Your immune system is designed to identify and neutralize threats like bacteria and viruses. However, in individuals with allergies, the immune system mistakenly identifies otherwise harmless substances, like pollen, pet dander, or certain foods, as dangerous invaders. This triggers an immune response that's disproportionate to the actual threat. This response involves the release of histamine and other chemicals, leading to the symptoms we associate with allergies, such as sneezing, itching, rash, or difficulty breathing. A truly weak immune system would be more susceptible to infections and illnesses, not necessarily prone to allergic reactions. In fact, some research suggests that individuals with allergies may even have a more robust immune response to some pathogens compared to those without allergies. Therefore, having allergies doesn't inherently indicate a compromised immune system; rather, it signifies a specific type of immune dysfunction where the response is misdirected and excessive.
If allergies are an overactive immune system, why are some people more prone to them than others?
The reasons behind individual susceptibility to allergies are complex and not fully understood, but several factors play significant roles. Genetics are a major contributor. A family history of allergies, asthma, or eczema significantly increases an individual's risk. This suggests a genetic predisposition towards an overactive immune response to certain allergens. Environmental factors also play a crucial part. Exposure to certain pollutants, irritants, and potential allergens during early childhood development can influence the development of allergies. The "hygiene hypothesis" proposes that a lack of early childhood exposure to infections and diverse microbes can lead to an underdeveloped and potentially overreactive immune system. Lifestyle factors, such as diet and stress levels, may also have an impact, though the exact mechanisms are still being investigated. Ultimately, the development of allergies is likely a result of a complex interaction between genetic predisposition and environmental triggers, making some individuals much more vulnerable than others.
Can a weak immune system make me more susceptible to developing allergies?
While allergies themselves don't directly indicate a weak immune system, a compromised immune system due to other factors could theoretically influence the development or severity of allergic reactions. A weakened immune system, perhaps due to illness, malnutrition, or certain medications, might be less capable of efficiently regulating the immune response. This could potentially lead to a more exaggerated allergic reaction. However, it's important to note that this is not a direct causal relationship. Having a weak immune system increases susceptibility to infections, but it doesn't automatically translate to a higher likelihood of developing allergies. The underlying mechanisms driving allergic reactions remain distinct from those responsible for overall immune deficiency. In essence, a weak immune system is a separate issue from the overactive immune response characteristic of allergies. Therefore, while a compromised immune system might exacerbate allergic symptoms, it's not a primary cause of allergies.
Should I be concerned if I have both allergies and frequent infections?
Experiencing both allergies and frequent infections warrants a visit to your doctor. While allergies and a weakened immune system are not directly linked, the simultaneous presence of both suggests a need for thorough assessment. Frequent infections indicate a potential issue with your immune system's ability to fight off pathogens effectively. It's important to determine the underlying cause of the frequent infections, as this could be a separate issue entirely unrelated to your allergies. Your doctor can conduct tests to rule out any underlying conditions, such as immune deficiencies or other health problems. Treatment might involve addressing both the allergies and the weakened immune system. For allergies, this could include allergy shots or medications. Strengthening your immune system might involve lifestyle changes, dietary improvements, or management of any underlying health conditions. Never self-diagnose or self-treat; consulting a healthcare professional is crucial for accurate diagnosis and appropriate management of both allergies and frequent infections.
Deja una respuesta