Does drinking milk reduce allergies

Milk, a ubiquitous beverage consumed by billions worldwide, has long been praised for its nutritional value. Yet, its purported health benefits extend beyond its ability to strengthen bones and teeth. In recent years, research has explored a potential link between milk consumption and the reduction of allergies. This article delves into the scientific evidence to examine whether drinking milk can indeed alleviate the symptoms and prevalence of allergic reactions.
Does Drinking Milk Reduce Allergies? A Closer Look
The relationship between milk consumption and allergies is complex and not fully understood. While some studies suggest a potential link between early introduction of cow's milk and a reduced risk of certain allergies, other research offers conflicting results. It's crucial to understand that there's no definitive answer to whether drinking milk reduces allergies, and individual responses vary greatly.
The Hygiene Hypothesis and Milk Consumption
The hygiene hypothesis proposes that early exposure to various microbes strengthens the immune system, making it less prone to allergies. Some argue that milk, being a common food introduced early in life, could contribute to this effect by introducing a variety of proteins and potentially stimulating immune tolerance. However, this theory remains under investigation, and more research is needed to clarify the direct link between milk consumption and a strengthened immune response against allergens.
Milk Proteins and Allergen Exposure
Cow's milk contains various proteins, some of which are known allergens. Early introduction of cow's milk might induce oral tolerance, a process where the immune system learns to recognize and tolerate these proteins. This tolerance could potentially extend to other allergens, leading to a decreased risk of developing allergies. However, this is not guaranteed and the mechanism remains unclear. Early introduction could also trigger an allergic reaction in predisposed individuals, so caution is advised.
Studies Showing Mixed Results
Numerous studies have explored the association between milk consumption and allergy development. Some studies suggest a protective effect of early milk introduction against allergies like eczema and asthma. However, other studies have found no significant association or even a potential increased risk in certain populations. These inconsistencies highlight the complexity of this issue and the need for further, large-scale, well-designed studies to draw definitive conclusions. The existing data suggests no consistent, universally applicable conclusion can be made.
Genetic Predisposition and Individual Responses
An individual's genetic predisposition plays a significant role in determining their risk of developing allergies. Some individuals are genetically more likely to develop allergies, regardless of their milk consumption habits. Others may exhibit a protective response to early milk exposure, while others may develop milk allergies themselves. Therefore, any conclusions about the effect of milk on allergies must consider the significant role of individual genetic factors.
The Importance of Consultations with Healthcare Professionals
Given the conflicting evidence and the individual variations in response, it's crucial to consult with a healthcare professional or allergist before making any decisions about milk consumption, especially regarding infants and young children. They can assess individual risk factors, consider family history of allergies, and provide personalized advice based on the individual's health status. Self-treating allergies is never advised.
| Factor | Effect on Allergy Risk (Milk Consumption) | Notes |
|---|---|---|
| Hygiene Hypothesis | Potentially protective (uncertain) | More research needed to establish a clear link. |
| Oral Tolerance | Potentially protective (uncertain) | May induce tolerance to milk proteins, but not necessarily other allergens. |
| Genetic Predisposition | Significant influence, independent of milk consumption | Individual genetic factors heavily influence allergy development. |
| Study Results | Mixed and inconsistent | Some studies show a protective effect; others show no effect or even an increased risk. |
| Individual Response | Highly variable | Responses vary greatly depending on genetics and other factors. |
Does Drinking Milk Reduce Allergies? A Closer Look
The relationship between milk consumption and allergies is complex and not fully understood. While some studies suggest a potential link between early introduction of cow's milk and a reduced risk of certain allergies, other research offers conflicting results. It's crucial to understand that there's no definitive answer to whether drinking milk reduces allergies, and individual responses vary greatly.
The Hygiene Hypothesis and Milk Consumption
The hygiene hypothesis proposes that early exposure to various microbes strengthens the immune system, making it less prone to allergies. Some argue that milk, being a common food introduced early in life, could contribute to this effect by introducing a variety of proteins and potentially stimulating immune tolerance. However, this theory remains under investigation, and more research is needed to clarify the direct link between milk consumption and a strengthened immune response against allergens.
Milk Proteins and Allergen Exposure
Cow's milk contains various proteins, some of which are known allergens. Early introduction of cow's milk might induce oral tolerance, a process where the immune system learns to recognize and tolerate these proteins. This tolerance could potentially extend to other allergens, leading to a decreased risk of developing allergies. However, this is not guaranteed and the mechanism remains unclear. Early introduction could also trigger an allergic reaction in predisposed individuals, so caution is advised.
Studies Showing Mixed Results
Numerous studies have explored the association between milk consumption and allergy development. Some studies suggest a protective effect of early milk introduction against allergies like eczema and asthma. However, other studies have found no significant association or even a potential increased risk in certain populations. These inconsistencies highlight the complexity of this issue and the need for further, large-scale, well-designed studies to draw definitive conclusions. The existing data suggests no consistent, universally applicable conclusion can be made.
Genetic Predisposition and Individual Responses
An individual's genetic predisposition plays a significant role in determining their risk of developing allergies. Some individuals are genetically more likely to develop allergies, regardless of their milk consumption habits. Others may exhibit a protective response to early milk exposure, while others may develop milk allergies themselves. Therefore, any conclusions about the effect of milk on allergies must consider the significant role of individual genetic factors.
The Importance of Consultations with Healthcare Professionals
Given the conflicting evidence and the individual variations in response, it's crucial to consult with a healthcare professional or allergist before making any decisions about milk consumption, especially regarding infants and young children. They can assess individual risk factors, consider family history of allergies, and provide personalized advice based on the individual's health status. Self-treating allergies is never advised.
| Factor | Effect on Allergy Risk (Milk Consumption) | Notes |
|---|---|---|
| Hygiene Hypothesis | Potentially protective (uncertain) | More research needed to establish a clear link. |
| Oral Tolerance | Potentially protective (uncertain) | May induce tolerance to milk proteins, but not necessarily other allergens. |
| Genetic Predisposition | Significant influence, independent of milk consumption | Individual genetic factors heavily influence allergy development. |
| Study Results | Mixed and inconsistent | Some studies show a protective effect; others show no effect or even an increased risk. |
| Individual Response | Highly variable | Responses vary greatly depending on genetics and other factors. |
Does drinking milk help with allergies?

The relationship between milk consumption and allergies is complex and not fully understood. There's no definitive answer to whether drinking milk helps with allergies, as it can actually exacerbate allergies in some individuals while potentially offering some benefits in others, depending on the specific type of allergy and individual factors. Studies have yielded conflicting results, with some suggesting a potential protective effect against certain allergies, particularly in early childhood, while others indicate that milk consumption might increase the risk of developing allergies.
Milk Allergy vs. Lactose Intolerance
It's crucial to distinguish between a milk allergy and lactose intolerance. A milk allergy is a true immune response triggered by milk proteins (casein and whey), leading to potentially serious symptoms like hives, vomiting, and difficulty breathing. Lactose intolerance, on the other hand, is a digestive issue caused by the inability to break down lactose, the sugar in milk, resulting in symptoms like bloating and diarrhea. Drinking milk can worsen milk allergies and lactose intolerance symptoms.
- Milk allergy symptoms can range from mild to severe.
- Lactose intolerance is not life-threatening, but can cause discomfort.
- Proper diagnosis by a medical professional is essential to determine the specific issue.
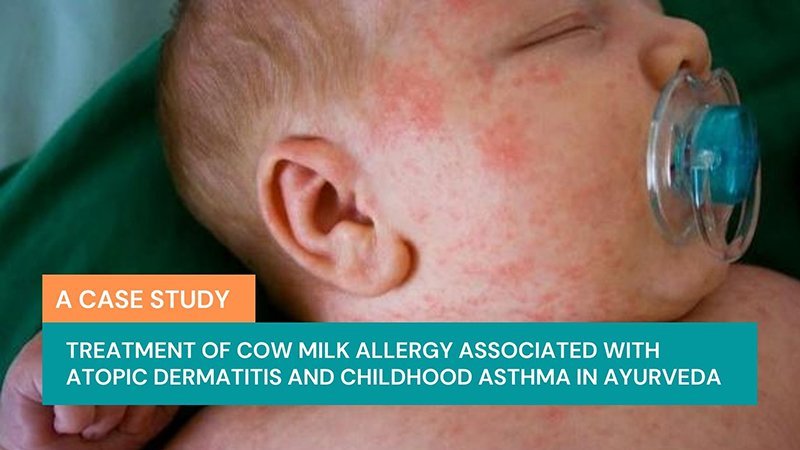
Milk and Atopic Dermatitis (Eczema)
Some studies suggest a potential link between milk consumption and atopic dermatitis (eczema), a common inflammatory skin condition often associated with allergies. While some research suggests that removing dairy from the diet might improve eczema symptoms in susceptible individuals, other studies have shown no significant effect. The mechanisms behind any potential association are not fully understood. It’s crucial to remember that the severity and response to dairy varies significantly between individuals.
- Eczema is characterized by itchy, inflamed skin.
- Eliminating dairy may help some children but not others.
- Consult a dermatologist or allergist for personalized advice.
Milk and Other Allergies (Asthma, Hay Fever)
The impact of milk on other allergic conditions, such as asthma and hay fever, is less clear. Some research indicates a potential protective effect of milk consumption in early childhood against the development of asthma and other atopic diseases, possibly related to the introduction of certain proteins. However, this remains a complex area of research with inconsistent findings. More research is needed to establish a definitive link.
- Asthma is a chronic respiratory condition.
- Hay fever is an allergic reaction to pollen.
- The role of milk in these conditions needs further investigation.
The Hygiene Hypothesis and Milk Consumption
The hygiene hypothesis suggests that early exposure to certain substances, including potential allergens like milk proteins, might help train the immune system and reduce the risk of developing allergies later in life. This is a controversial theory, and while some studies support the idea of a possible protective effect of early exposure to milk, there is no consensus on the role of milk within this hypothesis. More research is needed to understand the complex interactions between early life exposure and immune system development.
- The hygiene hypothesis is a complex and evolving theory.
- Early exposure to allergens can have both positive and negative effects.
- Further studies are crucial to understand the mechanisms involved.
Individual Responses to Milk
It's important to remember that individual responses to milk vary significantly. What might be beneficial for one person could be harmful to another. Factors such as genetic predisposition, the type and amount of milk consumed, and the presence of other allergies can influence the outcome. Therefore, personalized advice from a healthcare professional is essential to determine whether milk consumption is appropriate for an individual’s specific circumstances.
- Genetic factors influence allergic responses.
- Amount and type of milk consumed matter.
- Individual reactions can vary widely.
What can I drink to relieve allergies?
:max_bytes(150000):strip_icc()/natural-allergy-remedies-89245_final-afc2c7d8000b4df183653b6b2af84f41.jpg)
There's no single magic drink to cure allergies, but certain beverages can help alleviate symptoms by addressing underlying issues like dehydration, inflammation, and histamine release. These drinks often work best in conjunction with other allergy management strategies like medication and environmental controls. It's crucial to remember that these are supportive measures and not replacements for medical advice. If your allergies are severe, consult a doctor or allergist.
Water
Staying hydrated is paramount when dealing with allergies. Allergic reactions often lead to increased mucus production and watery eyes, contributing to dehydration. Drinking plenty of water helps thin mucus, making it easier to clear from your system. It also helps your body function optimally, supporting your immune system's response to allergens.
- Drink at least eight glasses of water daily, more if you're experiencing excessive sweating or nasal discharge.
- Consider adding a slice of lemon or lime for added flavor and Vitamin C, an antioxidant that may help support immune function.
- Carry a reusable water bottle to remind yourself to drink throughout the day.
Herbal Teas
Certain herbal teas contain compounds with anti-inflammatory and antihistamine properties that may help soothe allergy symptoms. Note that these are not scientifically proven to cure allergies but may offer some relief for mild symptoms. Always check for potential interactions with other medications.
- Chamomile tea: Known for its calming and anti-inflammatory effects.
- Ginger tea: Possesses anti-inflammatory properties that may help reduce swelling and inflammation associated with allergies.
- Nettle tea: Contains compounds that may act as natural antihistamines, although more research is needed to confirm its effectiveness.
Broth-Based Soups
Warm broths, especially those made with bone broth, can be incredibly soothing during allergy season. The warmth can help relieve congestion, and the electrolytes can help combat dehydration. Bone broth, in particular, is rich in nutrients that may support immune health.
- Chicken broth is a classic choice, easily digestible and comforting.
- Vegetable broth provides vitamins and minerals without the added protein of meat broths.
- Consider adding spices like turmeric or ginger, known for their anti-inflammatory properties.
Fruit and Vegetable Juices
Juices rich in Vitamin C and antioxidants may help support immune function and potentially reduce inflammation. However, be mindful of added sugars in commercially produced juices; opt for freshly squeezed or minimally processed options. The fiber in whole fruits and vegetables is also beneficial.
- Orange juice is a good source of Vitamin C.
- Pomegranate juice is rich in antioxidants.
- Beet juice has anti-inflammatory properties.
Electrolyte Drinks
If you're experiencing significant fluid loss due to watery eyes, sneezing, and runny nose, electrolyte drinks can help replenish essential minerals lost through dehydration. Choose electrolyte drinks without added sugar, as sugar can exacerbate inflammation. Plain water is still the best choice for most people.
- Low-sugar sports drinks can provide electrolytes like sodium and potassium.
- Homemade electrolyte drinks can be made with water, salt, and a touch of honey or fruit juice.
- Consult a healthcare professional about appropriate electrolyte replenishment if you have severe allergy symptoms.
Can milk make seasonal allergies worse?

The relationship between milk consumption and seasonal allergies is complex and not fully understood. While there's no definitive evidence that milk directly causesseasonal allergies to worsen, some research suggests a potential correlation or indirect influence. This is primarily due to the interaction between milk and the immune system, which is already stressed during allergy season. Some individuals might experience an increase in mucus production or exacerbate existing respiratory symptoms after consuming milk, but this is often linked to individual sensitivities or intolerances rather than a direct allergic reaction to milk proteins themselves. The effects, if any, are likely to be subtle and vary significantly between individuals. More research is needed to establish a clear causal link.
Milk and Mucus Production
Milk, particularly cow's milk, contains proteins that can stimulate mucus production in some individuals. This is not a true allergic reaction in the same way as pollen allergies, but rather a form of intolerance. Increased mucus can worsen symptoms of seasonal allergies like a runny nose and congestion, making it seem like milk is directly aggravating the allergy. This effect is more pronounced in individuals with pre-existing sensitivities to dairy products. Increased mucus production might be mistaken for a worsening of allergy symptoms.
- Individuals with lactose intolerance may experience increased mucus due to digestive discomfort.
- Milk proteins can trigger inflammation in the gut, potentially leading to increased mucus production throughout the body.
- This increased mucus can clog nasal passages and exacerbate allergy symptoms.
The Role of Inflammation
Dairy products, including milk, can contribute to systemic inflammation in the body. Inflammation plays a significant role in allergic reactions, and increased inflammation from milk consumption could potentially worsen the inflammatory response triggered by allergens. However, the extent to which milk-induced inflammation contributes to seasonal allergy symptoms needs further investigation. It's crucial to differentiate between a direct effect of milk on allergies and its indirect role through inflammation.
- Certain milk proteins have been associated with inflammatory responses in some individuals.
- Chronic inflammation can increase the body's sensitivity to allergens.
- Reducing inflammation through diet might indirectly improve allergy symptoms, but more research is needed to isolate the effect of milk.
Milk and Immune System Function
The immune system is heavily involved in both allergies and the body's response to milk proteins. During allergy season, the immune system is already working overtime. Consuming milk might add further stress on the immune system, potentially influencing the severity of allergic reactions, although this is speculative and requires more research. The body's response to both allergens and milk proteins can be quite individualized and complex.
- The immune system's response to allergens is often amplified during allergy season.
- Adding milk consumption might put additional strain on immune system resources.
- This added strain could theoretically exacerbate allergic symptoms, although this is not definitively proven.
Individual Sensitivities and Intolerances
The impact of milk on seasonal allergies is strongly influenced by individual sensitivities and intolerances. Some people are lactose intolerant, meaning they lack the enzyme needed to digest lactose (a milk sugar). This can lead to digestive distress, which might mimic or worsen allergy symptoms. Others might have less severe sensitivities to milk proteins, leading to milder symptoms like increased mucus. Individual variations in immune system responses are significant.
- Lactose intolerance causes digestive problems that can overlap with allergy symptoms.
- Milk protein sensitivities can lead to various symptoms, some resembling allergic reactions.
- It's essential to consider individual reactions when assessing the relationship between milk and allergies.
Distinguishing Milk Intolerance from Allergy
It’s crucial to differentiate between a true milk allergy (a rare but serious condition) and milk intolerance. A true milk allergy involves a reaction of the immune system to milk proteins, resulting in potentially severe symptoms. Milk intolerance, on the other hand, involves digestive issues due to the inability to properly digest lactose. Symptoms of milk intolerance might be mistaken for worsened allergy symptoms, but these are distinct conditions with different underlying mechanisms.
- Milk allergy is a true immune response involving IgE antibodies, leading to potentially severe reactions.
- Milk intolerance is due to a lack of lactase enzyme, causing digestive discomfort.
- Proper diagnosis is needed to distinguish between these conditions to determine if milk is truly worsening allergies or causing unrelated symptoms.
Is milk good for skin allergies?
The relationship between milk consumption and skin allergies is complex and not definitively understood. While milk itself doesn't directly causeskin allergies, it can exacerbate existing conditions or trigger reactions in susceptible individuals. Many people with eczema, a common skin allergy, find that dairy products worsen their symptoms. This is likely due to several factors, not just a direct allergic reaction. Some individuals may have a true milk allergy, exhibiting symptoms like hives, itching, swelling, or difficulty breathing. Others may experience intolerance, characterized by digestive issues such as bloating or diarrhea, which can indirectly affect skin health. Still others may have a sensitivity to components within milk, such as casein, whey protein, or lactose. These components can trigger inflammation throughout the body, including the skin, leading to symptoms like redness, dryness, and increased itching. Therefore, a definitive "yes" or "no" answer to whether milk is good for skin allergies is impossible. It depends greatly on the individual and the nature of their skin condition. A dermatologist or allergist can help determine if dairy is contributing to an individual's skin problems.
Milk Allergy vs. Lactose Intolerance vs. Milk Sensitivity
It's crucial to distinguish between a true milk allergy, lactose intolerance, and a sensitivity to milk proteins. A milk allergy is an immune system reaction to milk proteins, often causing severe symptoms. Lactose intolerance, on the other hand, involves difficulty digesting the sugar in milk, typically leading to gastrointestinal discomfort. Milk sensitivity is a broader term encompassing a range of reactions to milk components, often less severe than allergies but still impacting skin health. Understanding the difference is key in determining whether or not milk is a problem.
- Milk Allergy: Involves an IgE-mediated immune response, resulting in potentially life-threatening reactions.
- Lactose Intolerance: A digestive issue caused by a deficiency in the lactase enzyme, responsible for breaking down lactose.
- Milk Sensitivity: A broader term that includes non-IgE mediated reactions and intolerances to components beyond lactose.
The Role of Inflammation in Skin Allergies and Milk Consumption
Many skin allergies, including eczema and psoriasis, are characterized by inflammation. Milk, particularly its proteins, can trigger inflammatory responses in the body. This inflammation can worsen existing skin conditions or contribute to the development of new ones. The exact mechanisms aren't fully understood, but it's thought that milk proteins can activate immune cells, leading to the release of inflammatory mediators that affect the skin.
- Inflammatory Mediators: Milk proteins can stimulate the release of substances like cytokines and histamines, which contribute to inflammation.
- Immune Cell Activation: Certain components in milk can activate immune cells, leading to a cascade of inflammatory events.
- Gut-Skin Axis: Inflammation in the gut, triggered by milk consumption, can affect skin health through the gut-skin axis.
Casein and Whey Protein: Potential Culprits in Skin Allergy Exacerbation
Casein and whey are the major proteins found in milk and are frequently implicated in skin allergy reactions. These proteins are known to be highly allergenic in some individuals. They can trigger inflammatory responses and exacerbate existing skin conditions. The specific mechanisms by which they contribute to skin problems remain an area of ongoing research.
- Casein: A slow-digesting protein that can trigger reactions in susceptible individuals.
- Whey: A fast-digesting protein, also a common allergen.
- Individual Variations: The impact of casein and whey varies significantly between individuals.
The Importance of an Elimination Diet and Consultation with a Healthcare Professional
If you suspect milk is contributing to your skin allergies, an elimination diet can be a valuable tool for identifying trigger foods. This involves temporarily removing milk from your diet and observing whether your skin symptoms improve. However, it’s vital to consult with a dermatologist or allergist before starting any elimination diet, especially if you have severe allergies. They can help determine if milk is indeed a problem and guide you through the process safely and effectively.
- Elimination Diet: Systematically removing milk and observing for changes in skin symptoms.
- Professional Guidance: A dermatologist or allergist can provide personalized advice and manage potential risks.
- Reintroduction Phase: Once milk is removed, a controlled reintroduction helps confirm the diagnosis.
Managing Skin Allergies Related to Milk Consumption
If milk is identified as a trigger for your skin allergy, management strategies will depend on the severity of your reaction. Options might include completely eliminating dairy from your diet, substituting with dairy alternatives (like almond or soy milk), or using over-the-counter or prescription medications to manage skin symptoms. In some cases, allergy immunotherapy might be considered, but this is typically reserved for severe, persistent allergies.
- Dairy Elimination: Completely removing milk and dairy products from the diet.
- Dairy Alternatives: Substituting cow's milk with plant-based alternatives.
- Medication: Using topical corticosteroids or other medications to manage skin symptoms.
Does drinking milk actually help reduce allergies?
The relationship between milk consumption and allergy reduction is complex and not definitively proven. While some studies suggest a possible link between early introduction of cow's milk and a reduced risk of developing certain allergies, like eczema and asthma, in some children, these findings are not universally consistent. Many factors influence allergy development, including genetics, exposure to environmental allergens, and hygiene hypothesis. A significant body of research indicates that introducing allergens early, like in the case of peanut allergies, can actually reduce the risk of sensitization and developing allergies. However, this does not necessarily translate to all foods. Cow's milk, in particular, contains a variety of proteins that are known allergens, which can trigger allergic reactions in some individuals. Therefore, the idea that drinking milk reduces allergies is a simplification, and more research is needed to establish a clear causal relationship. In fact, for many children, cow's milk itself is a common allergen, making it counterintuitive to suggest it as a preventative measure. Parents concerned about allergies should always consult a pediatrician or allergist before making dietary decisions for their children. The timing and manner of introducing potential allergens should be carefully considered and guided by professional medical advice tailored to the individual child's risk factors and family history.
Is there any scientific evidence supporting the claim that milk reduces allergies?
The scientific evidence regarding milk's role in allergy reduction is inconclusive and often contradictory. While some observational studies have shown a correlation between early milk introduction and a lower incidence of certain allergies, these studies are often hampered by confounding factors. It's difficult to isolate the effect of milk consumption from other dietary factors, family history of allergies, and environmental exposures. Furthermore, correlation doesn't equal causation. Even if a statistical association is found, it doesn't prove that drinking milk causes a reduction in allergies. Conversely, other research has indicated that milk consumption may actually increase the risk of certain allergies in susceptible individuals, particularly cow's milk protein allergy. The protein structure of cow's milk can be a strong trigger for allergic reactions in infants and young children. Therefore, the current scientific consensus does not support the claim that drinking milk reduces allergies. More robust, well-designed studies are needed to explore this complex relationship and clarify its impact on different types of allergies and populations.
Can drinking milk prevent allergies in babies?
The idea of using milk to prevent allergies in babies is not supported by current scientific evidence. In fact, for some babies, introducing cow's milk too early can actually increase their risk of developing a cow's milk allergy. The timing of introducing potential allergens, including cow's milk, is a crucial factor to consider. Some studies suggest that introducing certain allergenic foods, like peanuts, early in a baby's life may be beneficial in reducing the risk of developing an allergy to that specific food. However, this approach isn't universally recommended for all foods and doesn't apply to cow's milk. The best course of action is to consult with a pediatrician or allergist to determine the appropriate time to introduce allergenic foods based on the baby's individual risk factors and family history. Early introduction of cow's milk could potentially lead to an allergic reaction in vulnerable children, so a cautious and individualized approach is always best. Rushing the introduction of potential allergens, including cow's milk, may have unintended consequences. It's crucial to prioritize a baby's health and safety and follow expert medical advice.
What are the potential risks of drinking milk if you have allergies?
For individuals with known allergies, drinking milk can pose significant risks. Cow's milk is a common allergen, containing several proteins that can trigger allergic reactions ranging from mild to severe. These reactions can manifest as skin rashes (eczema), gastrointestinal problems (vomiting, diarrhea, abdominal pain), respiratory issues (wheezing, coughing), and in severe cases, anaphylaxis, a life-threatening condition requiring immediate medical attention. Even individuals who don't have a diagnosed milk allergy can experience lactose intolerance, which causes digestive discomfort due to the inability to digest lactose, a sugar in milk. If you suspect you have a milk allergy or lactose intolerance, it's crucial to seek a professional diagnosis from a doctor or allergist. They can perform appropriate tests and recommend the best course of action, which may include avoiding milk and milk products altogether or substituting with alternative milk options like soy, almond, or oat milk. Ignoring potential allergic reactions to milk can be dangerous and can lead to serious health complications. Always prioritize your health and safety when dealing with allergies.
Deja una respuesta