Does drinking water reduce histamine

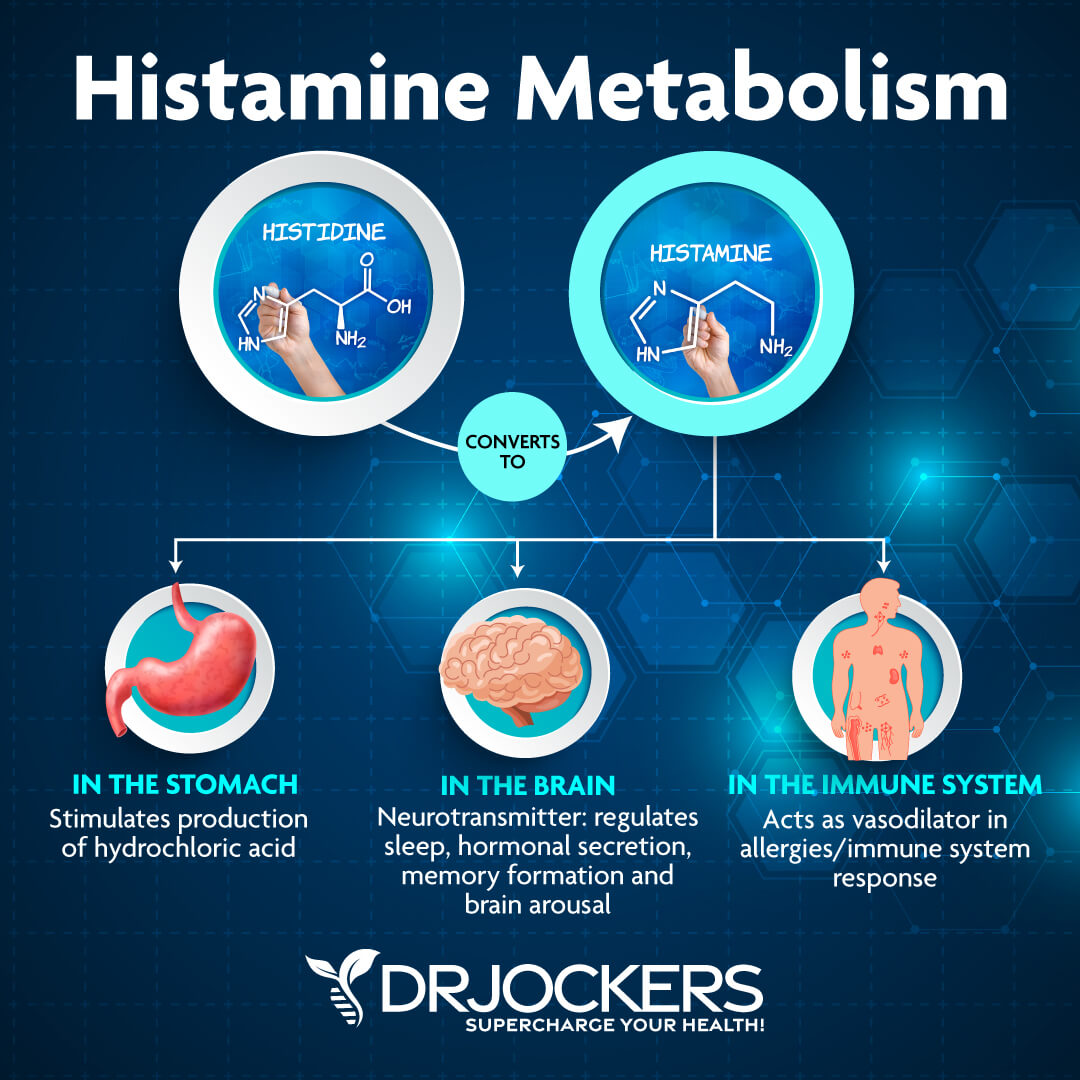
Does drinking water reduce histamine? This is a question that many people ask, especially those who suffer from histamine intolerance. Histamine is a compound that is produced by the body in response to allergens, and it can cause a variety of symptoms including headaches, nausea, and skin rashes. Drinking water is thought to help reduce histamine levels in the body by diluting it and helping it to be excreted. However, there is some debate about whether or not this is actually true. This article will examine the evidence for and against the claim that drinking water reduces histamine, and it will provide some tips for reducing histamine levels in the body.
Does Drinking Water Reduce Histamine Levels?
The relationship between water intake and histamine levels is complex and not fully understood. While there's no definitive scientific consensus stating that drinking water directly reduces histamine levels in the body, there are several indirect ways in which adequate hydration can influence histamine production and its effects.
How Hydration Affects Histamine Metabolism
The body's ability to metabolize histamine relies on several enzymatic processes. Dehydration can impair these processes, potentially leading to a buildup of histamine. Sufficient water intake ensures optimal enzyme function, aiding in the breakdown and removal of histamine. However, it's crucial to note that this is an indirect effect; water doesn't directly neutralize histamine molecules.
Water's Role in Flushing Out Histamine
Histamine is excreted from the body through urine. Adequate hydration supports efficient kidney function, facilitating the elimination of histamine and other metabolic waste products. This can contribute to a reduction in circulating histamine levels, although it doesn't directly lower histamine production.
The Impact of Water on Inflammation
Histamine is a key player in inflammatory responses. Chronic inflammation can lead to increased histamine release. Proper hydration plays a role in reducing inflammation throughout the body. By promoting healthy cell function and reducing oxidative stress, adequate water intake can indirectly contribute to lower histamine release triggered by inflammatory processes.
Water and Digestive Health: Minimizing Histamine Intake
Many foods high in histamine are also known to cause dehydration. Therefore, drinking plenty of water while consuming these foods can help to dilute the histamine concentration and potentially minimize the symptoms associated with high histamine intake.
The Limitations of Water in Histamine Management
It's essential to emphasize that drinking water alone is not a sufficient treatment for histamine intolerance or conditions characterized by excessive histamine release. While hydration plays a supportive role, managing histamine levels effectively often requires a multi-pronged approach, including dietary modifications, medication (if necessary), and stress management.
| Factor | Effect on Histamine |
|---|---|
| Adequate Hydration | Supports histamine metabolism, excretion, and reduces inflammation indirectly. |
| Dehydration | Can impair histamine metabolism, leading to potential buildup. |
| Water's Direct Effect on Histamine | Minimal to None |
| Overall Histamine Management | Water is a supportive factor, but not a primary treatment. |
Does Drinking Water Reduce Histamine Levels?
The relationship between water intake and histamine levels is complex and not fully understood. While there's no definitive scientific consensus stating that drinking water directly reduces histamine levels in the body, there are several indirect ways in which adequate hydration can influence histamine production and its effects.
How Hydration Affects Histamine Metabolism
The body's ability to metabolize histamine relies on several enzymatic processes. Dehydration can impair these processes, potentially leading to a buildup of histamine. Sufficient water intake ensures optimal enzyme function, aiding in the breakdown and removal of histamine. However, it's crucial to note that this is an indirect effect; water doesn't directly neutralize histamine molecules.
Water's Role in Flushing Out Histamine
Histamine is excreted from the body through urine. Adequate hydration supports efficient kidney function, facilitating the elimination of histamine and other metabolic waste products. This can contribute to a reduction in circulating histamine levels, although it doesn't directly lower histamine production.
The Impact of Water on Inflammation
Histamine is a key player in inflammatory responses. Chronic inflammation can lead to increased histamine release. Proper hydration plays a role in reducing inflammation throughout the body. By promoting healthy cell function and reducing oxidative stress, adequate water intake can indirectly contribute to lower histamine release triggered by inflammatory processes.
Water and Digestive Health: Minimizing Histamine Intake
Many foods high in histamine are also known to cause dehydration. Therefore, drinking plenty of water while consuming these foods can help to dilute the histamine concentration and potentially minimize the symptoms associated with high histamine intake.
The Limitations of Water in Histamine Management
It's essential to emphasize that drinking water alone is not a sufficient treatment for histamine intolerance or conditions characterized by excessive histamine release. While hydration plays a supportive role, managing histamine levels effectively often requires a multi-pronged approach, including dietary modifications, medication (if necessary), and stress management.
| Factor | Effect on Histamine |
|---|---|
| Adequate Hydration | Supports histamine metabolism, excretion, and reduces inflammation indirectly. |
| Dehydration | Can impair histamine metabolism, leading to potential buildup. |
| Water's Direct Effect on Histamine | Minimal to None |
| Overall Histamine Management | Water is a supportive factor, but not a primary treatment. |
Can you flush out histamine with water?
No, you cannot directly "flush out" histamine with water. Histamine is a molecule produced by your body and released in response to various stimuli, such as allergic reactions or injuries. While water is essential for overall bodily functions, including waste elimination, it doesn't specifically target or remove histamine from the body. The body's own systems, primarily the liver and enzymes like diamine oxidase (DAO), are responsible for breaking down and metabolizing histamine. Increased water intake might contribute to overall better hydration and potentially aid in the removal of waste products through urination, but it won't directly affect histamine levels in a significant way. The focus on managing histamine levels should be on addressing the underlying cause of histamine release or improving the body's capacity to process it, rather than relying on water alone.
How the Body Processes Histamine
The body employs several mechanisms to manage histamine levels. The liver plays a crucial role in the metabolism of histamine, converting it into less active metabolites. Additionally, enzymes like diamine oxidase (DAO) are responsible for breaking down histamine in the gut and other tissues. The effectiveness of these mechanisms can vary between individuals, and factors like genetics and gut health can significantly influence histamine processing.
- Liver metabolism: The liver is the primary site for histamine degradation, converting it to inactive compounds that can be excreted.
- Enzyme activity (DAO): Diamine oxidase (DAO) is a crucial enzyme responsible for breaking down histamine in the intestines.
- Kidney excretion: Some histamine metabolites are excreted by the kidneys through urine.
The Role of Hydration in Overall Health
Adequate hydration is crucial for maintaining overall health and supporting various bodily functions. Water is involved in numerous processes, including nutrient transport, waste removal, and temperature regulation. While it doesn't directly target histamine, good hydration is important for the proper function of the liver and kidneys, which are involved in histamine metabolism and excretion. Maintaining optimal hydration supports overall bodily functions but does not act as a specific histamine-removal mechanism.
- Waste removal: Water aids in flushing out various waste products through urination.
- Kidney function: Proper hydration is essential for optimal kidney function, which is vital in waste excretion.
- Liver function: Sufficient hydration supports liver function, impacting the liver's ability to metabolize histamine.
Dietary Strategies for Histamine Intolerance
If you experience symptoms associated with histamine intolerance, dietary modifications might be more effective than simply increasing water intake. A low-histamine diet involves limiting foods that are high in histamine or contain compounds that can promote histamine release. It’s important to consult with a healthcare professional or registered dietitian for personalized dietary advice.
- Restricting high-histamine foods: This includes fermented foods, aged cheeses, cured meats, and certain seafood.
- Incorporating histamine-reducing foods: Foods such as pineapple and ginger may help support the body's histamine processing capabilities.
- Consulting a professional: Working with a registered dietitian can ensure safe and effective dietary changes.
Medical Treatments for Histamine-Related Conditions
For individuals with conditions involving excessive histamine release, such as allergies, medical treatments may be necessary. Antihistamines are medications that block the effects of histamine, reducing symptoms. Other treatments may target the underlying cause of the condition, such as immunotherapy for allergies or medications to manage mast cell activation disorders. Always consult a healthcare professional for diagnosis and treatment.
- Antihistamines: These medications effectively block the action of histamine in the body.
- Immunotherapy: This treatment is used for allergies, and it can help desensitize the body to allergens.
- Other medications: Depending on the underlying condition, other medications may be used to manage histamine release and associated symptoms.
How do you flush histamines out of your body?
There's no single, quick way to "flush" histamines out of your body. Histamine is a naturally occurring chemical in your body involved in immune responses and other bodily functions. The feeling of being "histamine overloaded" usually stems from an overproduction or an inability to properly metabolize histamine, often triggered by foods, allergens, or certain medical conditions. Treating the underlying cause is crucial, and focusing on management rather than "flushing" is key. The body naturally breaks down histamine, but you can support this process through various approaches.
Supporting Histamine Metabolism
Your body relies on enzymes like diamine oxidase (DAO) and histamine N-methyltransferase (HNMT) to break down histamine. Supporting the function of these enzymes is a primary way to manage histamine levels. This can be achieved through dietary and lifestyle changes.
- Consume foods rich in DAO: Fermented foods like sauerkraut, kimchi, and kefir often contain beneficial bacteria that can aid in digestion and potentially improve DAO levels.
- Avoid histamine-releasing foods and drinks: This includes aged cheeses, cured meats, fermented fish (like sardines and anchovies), spinach, tomatoes, and alcoholic beverages. The list is extensive and varies from person to person.
- Consider DAO supplementation: If DAO levels are suspected to be low, a doctor might recommend supplementation to aid in histamine breakdown.
Hydration and Dietary Strategies
Adequate hydration and specific dietary choices can indirectly help manage histamine levels. Staying well-hydrated helps with overall bodily functions, including the efficient processing and removal of substances like histamine. Careful attention to diet plays a critical role.
- Drink plenty of water: Water helps to flush out toxins and waste products from the body, potentially helping to dilute histamine.
- Eat a diet rich in anti-inflammatory foods: Foods like berries, leafy greens, and fatty fish can help reduce overall inflammation, which can indirectly impact histamine levels. This is because inflammation can increase histamine release.
- Consider a low-histamine diet: Working with a doctor or registered dietitian to implement a carefully planned low-histamine diet can significantly reduce the amount of histamine you are ingesting.
Managing Allergic Reactions
If your elevated histamine levels are due to allergies, addressing the allergic response is crucial. This will help reduce histamine production stemming from the allergic reaction itself.
- Identify and avoid allergens: Allergy testing can help identify specific triggers. Avoiding these allergens will significantly reduce histamine release.
- Take antihistamines: Over-the-counter or prescription antihistamines can block the effects of histamine, providing relief from allergy symptoms. This doesn't remove the histamine, but mitigates its effects.
- Use other allergy treatments: Depending on the type of allergy, other treatments like immunotherapy may be considered to reduce the body's allergic response in the long term.
Addressing Underlying Medical Conditions
Certain medical conditions can cause increased histamine levels or impaired histamine metabolism. Addressing these conditions is vital for managing histamine levels.
- Seek medical advice: If you suspect an underlying medical condition is contributing to high histamine levels, consulting a doctor is crucial for proper diagnosis and treatment.
- Manage chronic illnesses: Conditions like mast cell activation syndrome (MCAS) or autoimmune disorders can affect histamine levels; managing these conditions through appropriate medical care is essential.
- Discuss medication interactions: Some medications can affect histamine levels either by increasing or decreasing them; discussing medications with a doctor is important to avoid any potential negative interactions.
Lifestyle Modifications
Besides diet, lifestyle changes can play a supporting role in managing histamine. Reducing stress and prioritizing sleep contribute to overall well-being and can indirectly influence histamine production.
- Manage stress levels: Chronic stress can worsen inflammation and potentially increase histamine release. Stress-reducing techniques like yoga, meditation, or deep breathing can be helpful.
- Prioritize sleep: Adequate sleep is essential for various bodily functions, including the regulation of the immune system and histamine production. Aim for 7-9 hours of quality sleep each night.
- Regular exercise: Moderate exercise can improve overall health and reduce inflammation. However, be mindful that intense exercise might trigger histamine release in some individuals, so moderation is key.
Does dehydration increase histamine?
Does Dehydration Increase Histamine?
The relationship between dehydration and histamine levels is complex and not fully understood. While there isn't direct evidence showing dehydration directlyincreases histamine production, there's a growing body of research suggesting an indirect link. Dehydration can lead to various physiological changes that might influence histamine release or the body's response to it. These changes could potentially exacerbate symptoms in individuals prone to histamine-related issues, like allergies or mast cell activation syndrome.
Histamine Release and Dehydration's Impact on Blood Volume
Dehydration reduces blood volume, which can lead to increased blood viscosity (thickness). This thicker blood can impair the efficient circulation of immune cells and other factors that usually regulate histamine release. Reduced blood flow might also hinder the removal of histamine from tissues, potentially leading to a higher concentration in certain areas. This isn't a direct increase in histamine production, but rather a shift in its distribution and clearance.
- Reduced blood flow can lead to localized histamine buildup.
- Increased blood viscosity makes it harder for immune cells to effectively patrol and regulate inflammation.
- Impaired circulation can delay the removal of histamine from affected areas.
Dehydration and the Gut Microbiome
The gut microbiome plays a crucial role in immune function and histamine metabolism. Dehydration can disrupt the gut microbiome's delicate balance, leading to dysbiosis (an imbalance of beneficial and harmful bacteria). Changes in gut flora could influence histamine production by bacteria or the body's ability to metabolize histamine effectively. This could potentially lead to higher circulating histamine levels, although the mechanisms are not fully elucidated.
- Gut dysbiosis can result from dehydration-induced changes in gut transit time and nutrient absorption.
- Certain gut bacteria can produce histamine.
- An imbalanced gut microbiome can impact the body's ability to process and eliminate histamine.
Dehydration and Mast Cell Activation
Mast cells are immune cells that release histamine in response to various stimuli, including allergens and inflammation. Dehydration could indirectly impact mast cell activity. For example, dehydration-induced stress might increase the likelihood of mast cell degranulation (the release of histamine), particularly in individuals with mast cell activation syndrome or other conditions characterized by heightened mast cell reactivity. Stress related to dehydration can trigger the release of hormones that affect mast cell activity.
- Dehydration triggers the body’s stress response, potentially increasing cortisol and other stress hormones.
- These stress hormones can indirectly stimulate mast cell degranulation and histamine release.
- Individuals with underlying mast cell disorders might be more susceptible to this effect.
Dehydration and Inflammation
Dehydration is associated with increased inflammation throughout the body. Chronic inflammation can, in turn, lead to increased histamine release. While not a direct causal link, the inflammatory state induced by dehydration creates an environment where histamine release is more likely. The body's response to dehydration involves inflammatory processes aiming to restore fluid balance, which might involve histamine release as part of this response. Chronic dehydration fosters a pro-inflammatory state.
- Dehydration contributes to systemic inflammation.
- Inflammation itself can trigger histamine release from mast cells and other immune cells.
- This inflammatory response related to dehydration is a complex process involving multiple mediators, including histamine.
Individual Variability in Response to Dehydration
It's important to acknowledge that individual responses to dehydration vary considerably. Factors like pre-existing medical conditions (e.g., allergies, mast cell activation syndrome), genetic predisposition, and overall health status significantly influence how the body handles both dehydration and histamine regulation. Individual differences in histamine metabolism and immune responses modify the effect of dehydration on histamine levels. Some individuals might be more susceptible to experiencing histamine-related symptoms with dehydration than others.
- Genetic factors influence histamine metabolism and immune responses.
- Pre-existing conditions like allergies or mast cell activation syndrome increase sensitivity to histamine.
- Overall health and nutritional status impact the body's ability to cope with dehydration and regulate histamine.
Does drinking water flush out allergens?

No, drinking water does not directly flush out allergens in the way that, say, urination flushes out waste products from the bloodstream. Allergens, which are typically proteins or other substances that trigger an immune response, enter the body through various routes – inhalation (pollen, dust mites), ingestion (food), or contact (skin). Once these allergens are in the body, they trigger an immune response and inflammation. While adequate hydration is essential for overall health and proper bodily functions, including the immune system, the process of eliminating allergens is more complex than simply "flushing" them out with water.
How the Body Responds to Allergens
The body's response to allergens involves several complex processes. When an allergen enters the body, the immune system recognizes it as a foreign substance. This triggers the release of antibodies, particularly IgE antibodies. These antibodies bind to mast cells, which then release histamine and other inflammatory mediators. These mediators are responsible for the symptoms of allergic reactions, such as sneezing, itching, and swelling. Water doesn't directly counteract these immune responses.
- Antibody Production: The immune system produces antibodies (IgE) to target specific allergens.
- Mast Cell Activation: IgE antibodies bind to mast cells, triggering their activation.
- Histamine Release: Activated mast cells release histamine and other inflammatory mediators causing allergic symptoms.
The Role of Hydration in Immune Function
While water doesn't directly remove allergens, adequate hydration is crucial for overall immune function. The lymphatic system, a key component of the immune system, relies on proper fluid balance to effectively transport immune cells and remove waste products from tissues. Dehydration can impair lymphatic drainage, potentially hindering the body's ability to clear out allergens and other waste. However, this is an indirect effect, not a direct flushing mechanism.
- Lymphatic System Function: Proper hydration is vital for efficient lymphatic drainage.
- Immune Cell Transport: Water aids in the transport of immune cells throughout the body.
- Waste Removal: Hydration supports the removal of cellular waste, although not specifically allergens.
Other Ways the Body Eliminates Allergens
The body uses various mechanisms to eliminate allergens. For inhaled allergens, the respiratory system's mucus and cilia work together to trap and remove them. The digestive system processes ingested allergens, and the skin's barrier function helps protect against contact allergens. These processes are independent of hydration levels, although adequate hydration may support overall bodily function.
- Mucus and Cilia: The respiratory system traps and expels inhaled allergens.
- Digestive System: The digestive system processes and eliminates ingested allergens.
- Skin Barrier: The skin's protective barrier prevents allergen entry.
The Importance of Managing Allergic Reactions
Managing allergic reactions effectively involves various strategies, including allergen avoidance, medication (antihistamines, corticosteroids), and immunotherapy. Drinking plenty of water is a beneficial part of overall health but not a primary method for removing allergens. Focusing on these targeted approaches is far more effective in reducing symptoms and managing allergies.
- Allergen Avoidance: Reducing exposure to known allergens.
- Medication: Utilizing antihistamines and other allergy medications.
- Immunotherapy: Building tolerance to specific allergens over time.
Misconceptions about Water and Allergens
A common misconception is that drinking lots of water will magically eliminate allergens. This isn't supported by scientific evidence. While hydration supports overall health and immune function, it doesn't directly flush out allergens from the body. The mechanisms for allergen removal are complex and involve multiple systems within the body.
- No Direct Flushing Effect: Water doesn't directly remove allergens from the body.
- Indirect Support for Immune Function: Hydration supports overall immune function, but this is not the same as allergen removal.
- Focus on Effective Allergy Management: Prioritize proven allergy management strategies over relying on simple hydration.
Does drinking water help reduce histamine levels in the body?
The relationship between water intake and histamine levels is complex and not definitively established. While there's no direct evidence showing that drinking water significantly lowers histamine levels, hydration plays a crucial role in several bodily processes that indirectly influence histamine levels. Adequate hydration supports the proper functioning of the kidneys and liver, both of which are vital in processing and eliminating waste products, including histamine metabolites. When your kidneys and liver are functioning optimally due to sufficient hydration, they may be more efficient at removing histamine from the system. However, it's important to note that this is an indirect effect; drinking water doesn't directly neutralize histamine molecules. Furthermore, dehydration can exacerbate inflammatory responses, potentially leading to increased histamine release. Therefore, maintaining proper hydration is crucial for overall health and may indirectly contribute to better histamine management, but it shouldn't be considered a primary treatment for histamine intolerance or related conditions. More research is needed to fully understand the nuanced interaction between hydration and histamine levels.
Can drinking too much water worsen histamine intolerance symptoms?
While adequate hydration is generally beneficial, excessive water intake can potentially worsen symptoms associated with histamine intolerance in certain situations. This isn't directly due to the water itself, but rather due to potential complications it may trigger. For example, overhydration can lead to a dilution of electrolytes, impacting various bodily functions. Electrolyte imbalances can contribute to inflammation and, potentially, exacerbate histamine responses. Furthermore, if excessive water intake leads to frequent urination, it could lead to dehydration in the long run if not accompanied by proper electrolyte replacement. Dehydration, as previously mentioned, can actually increase histamine production and worsen symptoms. Therefore, while drinking enough water is important, it's crucial to maintain a balanced fluid intake and consume electrolytes to avoid potential negative consequences. The optimal water intake varies from individual to individual, so it's best to consult a healthcare professional to determine your personal needs.
Are there specific types of water that are better for managing histamine?
There is currently no scientific evidence suggesting that certain types of water (e.g., filtered water, spring water, alkaline water) are inherently better than others for managing histamine levels. The purported benefits of various types of water are often based on anecdotal evidence or marketing claims rather than rigorous scientific studies. While some individuals might feel that specific water types improve their symptoms, this is likely due to other factors, such as improved hydration in general or the avoidance of contaminants that could contribute to inflammation. For individuals with histamine intolerance, it's more crucial to focus on overall hydration and the quality of the water, making sure it's free of contaminants and heavy metals. Avoiding chlorinated water could be helpful for some individuals as chlorine can be irritating for sensitive people, but this doesn't directly impact histamine levels. Focus on drinking clean, filtered water in moderation, rather than relying on specific water types as a cure-all.
Can drinking water with added electrolytes help with histamine-related symptoms?
Drinking water with added electrolytes can be beneficial for individuals experiencing histamine-related symptoms, particularly those who struggle with maintaining proper hydration or experience electrolyte imbalances. As mentioned before, electrolyte imbalances can contribute to inflammation and potentially exacerbate histamine responses. By replenishing electrolytes lost through sweating or frequent urination (which can occur with excessive water intake or certain medical conditions), individuals can help maintain a balanced internal environment and improve overall health. However, it's important to note that adding electrolytes to water doesn't directly neutralize histamine. The benefit comes from supporting overall bodily functions and preventing dehydration, which in turn can help mitigate some of the adverse effects of histamine. It's advisable to consult a doctor or registered dietitian to determine the appropriate electrolyte balance for individual needs, especially if dealing with specific medical conditions or severe histamine intolerance.

Deja una respuesta