How do I know if I'm allergic

Have you ever wondered if you're allergic to something? Allergies are a common problem, affecting millions of people worldwide. They can cause a range of symptoms, from mild discomfort to life-threatening reactions. If you think you might be allergic to something, it's important to get tested so that you can take steps to avoid the allergen and prevent future reactions.
Recognizing Allergic Reactions: Signs and Symptoms
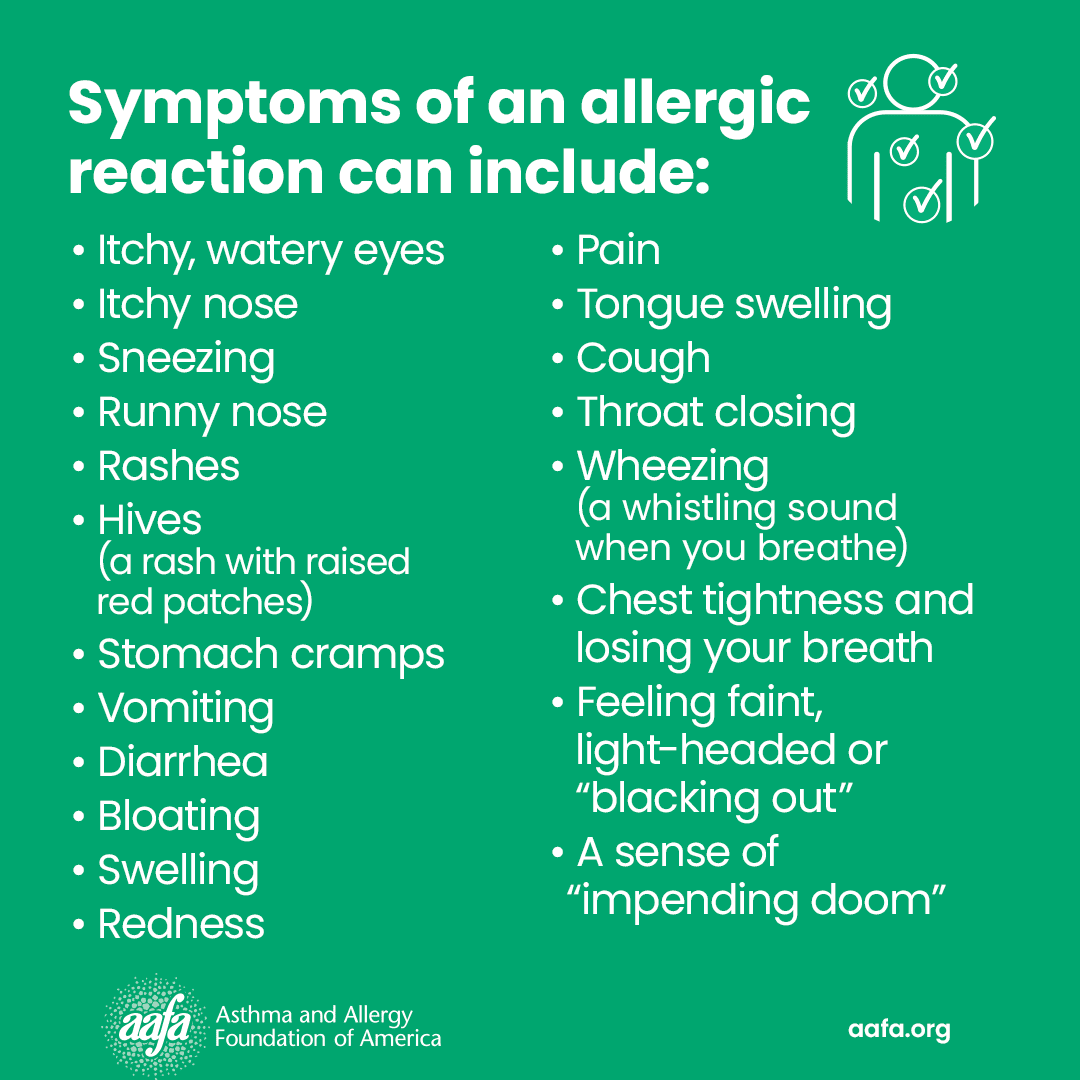
Determining if you have an allergy can be tricky, as symptoms vary greatly depending on the allergen and the individual. Many symptoms can mimic other illnesses, making self-diagnosis unreliable. It's crucial to consult a doctor or allergist for proper diagnosis and treatment. However, understanding common allergy symptoms can help you identify potential issues and seek medical attention promptly.
Immediate Reactions: Anaphylaxis and Other Severe Symptoms
Some allergies cause immediate and severe reactions that can be life-threatening. These reactions, known as anaphylaxis, may include: difficulty breathing, swelling of the face, lips, tongue, or throat, hives or rash, rapid pulse, dizziness or lightheadedness, and nausea or vomiting. If you experience any of these symptoms after exposure to a potential allergen, seek immediate medical attention. This is a medical emergency.
Delayed Reactions: Symptoms That Appear Hours or Days Later
Not all allergic reactions are immediate. Some allergies trigger symptoms hours or even days after exposure to the allergen. These delayed reactions might include: skin rashes (eczema), itchy eyes, runny nose, digestive issues (like bloating, stomach cramps, or diarrhea), and fatigue. While less dramatic than immediate reactions, persistent symptoms warrant a doctor's visit.
Common Allergens: Identifying Potential Triggers
Knowing common allergens can help you narrow down potential causes of your symptoms. Common culprits include: foods (peanuts, milk, eggs, soy, wheat, shellfish), pollen, pet dander, dust mites, insect stings, and medications. Keeping a detailed diary of your symptoms and activities, noting any potential exposures, can be incredibly helpful in identifying triggers.
Skin Testing and Blood Tests: Diagnostic Methods
Your doctor might recommend skin prick tests or blood tests to determine specific allergies. Skin prick tests involve placing small amounts of potential allergens on your skin and observing for a reaction. Blood tests measure the levels of specific antibodies (IgE) in your blood that indicate an allergic response. These tests can help identify specific allergens responsible for your symptoms.
Elimination Diets and Environmental Controls: Management Strategies
Once you've identified your allergens, you can work with your doctor or allergist to develop a management plan. This may involve an elimination diet to remove specific foods, environmental controls to minimize exposure to allergens (e.g., using air purifiers, dust mite covers), and potentially, immunotherapy (allergy shots) to desensitize you to certain allergens.
| Symptom Category | Symptoms | Severity |
|---|---|---|
| Immediate Reactions (Anaphylaxis) | Difficulty breathing, swelling of face/throat, hives, rapid pulse, dizziness | Severe, requires immediate medical attention |
| Delayed Reactions | Skin rashes, itchy eyes, runny nose, digestive issues, fatigue | Can range from mild to moderate; consult a doctor |
| Other Symptoms | Itching, sneezing, coughing, watery eyes | Variable severity |
Recognizing Allergic Reactions: Signs and Symptoms
Determining if you have an allergy can be tricky, as symptoms vary greatly depending on the allergen and the individual. Many symptoms can mimic other illnesses, making self-diagnosis unreliable. It's crucial to consult a doctor or allergist for proper diagnosis and treatment. However, understanding common allergy symptoms can help you identify potential issues and seek medical attention promptly.
Immediate Reactions: Anaphylaxis and Other Severe Symptoms
Some allergies cause immediate and severe reactions that can be life-threatening. These reactions, known as anaphylaxis, may include: difficulty breathing, swelling of the face, lips, tongue, or throat, hives or rash, rapid pulse, dizziness or lightheadedness, and nausea or vomiting. If you experience any of these symptoms after exposure to a potential allergen, seek immediate medical attention. This is a medical emergency.
Delayed Reactions: Symptoms That Appear Hours or Days Later
Not all allergic reactions are immediate. Some allergies trigger symptoms hours or even days after exposure to the allergen. These delayed reactions might include: skin rashes (eczema), itchy eyes, runny nose, digestive issues (like bloating, stomach cramps, or diarrhea), and fatigue. While less dramatic than immediate reactions, persistent symptoms warrant a doctor's visit.
Common Allergens: Identifying Potential Triggers
Knowing common allergens can help you narrow down potential causes of your symptoms. Common culprits include: foods (peanuts, milk, eggs, soy, wheat, shellfish), pollen, pet dander, dust mites, insect stings, and medications. Keeping a detailed diary of your symptoms and activities, noting any potential exposures, can be incredibly helpful in identifying triggers.
Skin Testing and Blood Tests: Diagnostic Methods
Your doctor might recommend skin prick tests or blood tests to determine specific allergies. Skin prick tests involve placing small amounts of potential allergens on your skin and observing for a reaction. Blood tests measure the levels of specific antibodies (IgE) in your blood that indicate an allergic response. These tests can help identify specific allergens responsible for your symptoms.
Elimination Diets and Environmental Controls: Management Strategies
Once you've identified your allergens, you can work with your doctor or allergist to develop a management plan. This may involve an elimination diet to remove specific foods, environmental controls to minimize exposure to allergens (e.g., using air purifiers, dust mite covers), and potentially, immunotherapy (allergy shots) to desensitize you to certain allergens.
| Symptom Category | Symptoms | Severity |
|---|---|---|
| Immediate Reactions (Anaphylaxis) | Difficulty breathing, swelling of face/throat, hives, rapid pulse, dizziness | Severe, requires immediate medical attention |
| Delayed Reactions | Skin rashes, itchy eyes, runny nose, digestive issues, fatigue | Can range from mild to moderate; consult a doctor |
| Other Symptoms | Itching, sneezing, coughing, watery eyes | Variable severity |
How can I find out what I am allergic to?

Figuring out what you're allergic to requires a multi-step process involving careful observation, detailed record-keeping, and potentially medical testing. It's crucial to remember that self-diagnosing allergies can be dangerous, so professional guidance is vital. Never attempt to test for allergies yourself. The steps outlined below should be considered preliminary investigations to aid your discussion with a healthcare professional.
1. Keeping a Detailed Allergy Diary
The first step is meticulous record-keeping. A detailed allergy diary should track everything you eat, drink, touch, and are exposed to, noting any symptoms that follow. Include even seemingly unrelated things, like new laundry detergent, changes in weather, or new medications. Be precise with details. For food, note the type, brand, preparation method, and amount. Note the timing of exposure and the onset and duration of symptoms. This provides valuable information for your doctor.
- Record all potential allergens, including foods, medications, pollen, pet dander, and household products.
- Describe symptoms in detail, including their location, intensity, and duration.
- Note the timing of exposure and symptom onset, noting the latency period between exposure and reaction.
2. Identifying Common Allergens and Your Symptoms
Familiarize yourself with common allergens to see if your symptoms align with known allergic reactions. Typical symptoms include hives, swelling, itching, rash, runny nose, sneezing, coughing, wheezing, shortness of breath, and gastrointestinal issues. Understanding the typical symptoms associated with different allergens can help narrow down possibilities. This information will be helpful when discussing your concerns with a doctor.
- Common food allergens: peanuts, tree nuts, milk, eggs, soy, wheat, fish, and shellfish.
- Common environmental allergens: pollen, dust mites, pet dander, mold.
- Common medication allergens: certain antibiotics (penicillin), aspirin, NSAIDs.
3. Consulting a Doctor or Allergist
A doctor is essential for accurate diagnosis and safe management of allergies. They can review your allergy diary, assess your symptoms, and order appropriate tests. They can also discuss any pre-existing conditions that may interact with potential allergies. They are trained to interpret test results and provide appropriate treatment plans. A specialist allergist is particularly helpful for complex cases.
- Discuss your symptoms, medical history, and allergy diary with your doctor.
- Undergo recommended allergy tests (skin prick tests, blood tests).
- Develop a management plan for identified allergies, including medication and avoidance strategies.
4. Allergy Skin Prick Tests and Blood Tests
Your doctor might recommend allergy tests. Skin prick tests involve placing a small amount of allergen on your skin and pricking the skin to allow the allergen to enter. A positive reaction (wheal and flare) indicates an allergy. Blood tests measure the level of IgE antibodies (immunoglobulin E) specific to various allergens. These tests help pinpoint specific allergens causing your reactions.
- Skin prick tests are generally quick, inexpensive, and relatively painless.
- Blood tests are more sensitive and useful for detecting allergies to multiple substances.
- Both tests have limitations and may produce false positives or negatives.
5. Managing Allergies and Avoidance Strategies
Once allergens are identified, developing a management strategy is key. This involves avoiding contact with identified allergens, using medication as prescribed (antihistamines, epinephrine), and potentially undergoing immunotherapy (allergy shots). This requires a collaborative approach with your healthcare provider and careful attention to detail.
- Read food labels carefully and be aware of cross-contamination risks.
- Use protective measures (masks, gloves) when exposed to environmental allergens.
- Carry an epinephrine auto-injector if advised by your doctor.
What are the 7 allergy symptoms?
What are the 7 Allergy Symptoms?
While there are many potential allergy symptoms, and the specific symptoms experienced can vary greatly depending on the allergen and the individual, seven common symptoms encompass a broad range of allergic reactions. It's important to note that experiencing these symptoms doesn't automatically mean you have an allergy; a proper diagnosis from a healthcare professional is crucial.
Skin Reactions
Allergic skin reactions are very common and can manifest in several ways. These reactions are often caused by direct contact with an allergen (contact dermatitis) or an allergic response triggered elsewhere in the body. The severity can range from mild irritation to severe, widespread reactions.
- Hives (urticaria): Raised, itchy welts on the skin.
- Eczema: Inflamed, itchy, dry skin.
- Rash: A widespread skin eruption.
Respiratory Symptoms
The respiratory system is frequently affected by allergies, leading to various symptoms that can significantly impact breathing and overall comfort. These reactions are often triggered by airborne allergens like pollen, dust mites, or pet dander. The severity can range from mild discomfort to life-threatening conditions.
- Runny nose (rhinorrhea): Excessive nasal mucus production.
- Sneezing: A reflex action to clear the nasal passages.
- Itchy, watery eyes: Inflammation and irritation of the conjunctiva.
Gastrointestinal Symptoms
While less common than skin or respiratory symptoms, allergies can also manifest in the gastrointestinal tract, causing discomfort and digestive issues. These reactions are often triggered by food allergens or certain medications. Symptoms can vary in severity, from mild discomfort to severe reactions.
- Nausea: A feeling of sickness or queasiness.
- Vomiting: Forcible expulsion of stomach contents.
- Diarrhea: Loose, watery stools.
- Abdominal cramps: Pain or discomfort in the abdomen.
Itching
Itching is a very common symptom across various allergic reactions. It can affect the skin, eyes, nose, throat, and other areas of the body, and is often caused by the release of histamine and other inflammatory mediators. The intensity of itching can range from mild discomfort to intense, unbearable sensations, leading to scratching and further skin irritation.
- Skin itching: An uncomfortable sensation prompting the urge to scratch.
- Itchy eyes: Irritation and discomfort in the eyes.
- Itchy nose and throat: Discomfort and irritation in the nasal passages and throat.
Swelling
Swelling, or edema, occurs when fluid accumulates in tissues. In allergic reactions, this swelling can affect different parts of the body, ranging from mild puffiness to severe, life-threatening conditions. The location and extent of swelling are crucial indicators of the severity of the allergic reaction.
- Facial swelling: Puffiness around the eyes, lips, or face.
- Tongue swelling: Enlargement of the tongue.
- Throat swelling (angioedema): Swelling of the tissues in the throat, which can cause breathing difficulties.
Breathing Difficulties
Allergic reactions can sometimes cause significant breathing problems. This can range from mild wheezing to severe difficulty breathing (anaphylaxis). Breathing difficulties are a medical emergency and require immediate medical attention.
- Wheezing: A whistling sound during breathing.
- Shortness of breath: Difficulty getting enough air.
- Tight chest: A feeling of constriction or pressure in the chest.
Anaphylaxis
Anaphylaxis is a severe, life-threatening allergic reaction that requires immediate medical attention. It's characterized by a sudden onset of multiple symptoms, including those mentioned above, and can lead to a rapid drop in blood pressure (shock) and potentially death if left untreated. This is a medical emergency requiring immediate epinephrine injection and transport to a hospital.
- Sudden onset of multiple symptoms (such as those listed above).
- Rapid drop in blood pressure (shock).
- Loss of consciousness.
How do I know if I'm having allergies?
:max_bytes(150000):strip_icc()/how-do-you-know-if-you-have-allergies-5202927-FINAL-c74839b604b942b1ba9a658f0fc245d2.jpg)
How Do I Know If I'm Having Allergies?
Identifying allergies can be tricky, as symptoms can vary widely depending on the allergen and the individual. However, some common signs and symptoms can help you determine if you might be experiencing an allergic reaction. The key is to pay attention to the timing of your symptoms – do they occur after exposure to a specific substance, such as pollen, pet dander, or certain foods? If so, it’s worth investigating further. Keep a detailed record of your symptoms and when they occur to help your doctor make a diagnosis. Seek medical advice if your symptoms are severe or concerning, particularly if you experience difficulty breathing or swelling of the face, lips, or tongue.
Common Allergy Symptoms
Allergic reactions manifest in various ways. Some common symptoms include: sneezing, runny or stuffy nose, itchy eyes, watery eyes, skin rash (hives), itching, and coughing. The severity of these symptoms can range from mild discomfort to severe reactions. It is crucial to note the pattern and severity of these symptoms to help determine the possible cause. For example, if sneezing and a runny nose occur only during specific seasons, it may point towards seasonal allergies (hay fever).
- Sneezing fits: Frequent, repetitive sneezing is a classic allergy symptom.
- Itchy, watery eyes: This often accompanies a runny nose.
- Runny nose with clear mucus: Unlike a cold, allergic rhinitis typically produces clear mucus.
Food Allergies vs. Intolerances
It's important to differentiate between food allergies and food intolerances. Food allergies involve a reaction of the immune system, triggering a potentially life-threatening response. Symptoms can include hives, swelling, difficulty breathing, and even anaphylaxis. Food intolerances, on the other hand, are not immune-mediated, and symptoms are typically milder, such as digestive upset (bloating, gas, diarrhea). While both can be uncomfortable, food allergies require much more careful management.
- Anaphylaxis: A severe, life-threatening allergic reaction.
- Hives (urticaria): Raised, itchy welts on the skin.
- Gastrointestinal distress: Bloating, cramping, diarrhea, vomiting.
Environmental Allergens
Many people suffer from allergies triggered by environmental factors. Common culprits include pollen (from trees, grasses, and weeds), dust mites, pet dander (animal skin flakes), and mold spores. Seasonal changes often exacerbate these allergies, with symptoms peaking during specific times of the year. Identifying and minimizing exposure to these allergens can significantly improve symptoms.
- Pollen counts: Check local pollen forecasts to anticipate symptom flares.
- Dust mite avoidance: Use dust-mite-proof covers for mattresses and pillows.
- Pet dander control: Regularly clean your home and consider restricting pet access to certain areas.
Skin Allergy Manifestations
Allergies can also manifest as skin reactions. Contact dermatitis is a common type of skin allergy caused by direct contact with an irritant or allergen, such as certain plants (poison ivy), metals (nickel), or chemicals in cosmetics or cleaning products. Symptoms include redness, itching, rash, and swelling. Eczema (atopic dermatitis) is a chronic inflammatory skin condition that often has an allergic component. It can cause dry, itchy, and inflamed skin.
- Rashes: Red, itchy, bumpy skin.
- Hives: Raised, itchy welts.
- Eczema: Chronic inflammatory skin condition with dry, itchy skin.
Diagnosing Allergies
A doctor can help diagnose allergies through a combination of methods. A thorough medical history and physical examination are crucial first steps. Allergy tests, such as skin prick tests or blood tests, can identify specific allergens that trigger a reaction. Patch tests might be used to diagnose contact dermatitis. The specific diagnostic approach depends on the suspected allergens and the individual's symptoms. Accurate diagnosis is essential for effective management of allergic conditions.
- Skin prick test: A small amount of allergen is pricked onto the skin.
- Blood test: Measures the levels of specific IgE antibodies.
- Patch test: Allergens are applied to the skin under a patch for 48 hours.
How do you know if you're allergic to come?
Diagnosing a true allergy to semen (also known as seminal fluid) is complex and requires a professional medical evaluation. There's no single, definitive test, and reactions can vary greatly in severity. A person might experience a reaction to semen from one individual but not another. Many women experience mild discomfort, such as burning or itching after intercourse, which isn't necessarily an allergy. True allergic reactions typically involve a more significant immune system response.
Symptoms of a Semen Allergy
Allergic reactions to semen can manifest in various ways, ranging from mild to severe. Mild symptoms might be easily dismissed, while severe ones necessitate immediate medical attention. It's crucial to differentiate between a true allergy and other causes of discomfort during or after sexual intercourse. A doctor can help determine the underlying cause.
- Genital Irritation: Itching, burning, swelling, or redness of the vulva or vagina.
- Skin Reactions: Hives (urticaria), rash, or eczema in the genital area or other parts of the body.
- Respiratory Symptoms: In rare cases, more serious reactions can include shortness of breath, wheezing, or difficulty breathing.
Testing for Semen Allergy
There isn't a single, definitive test to diagnose a semen allergy. Diagnosing a true allergy involves a process of elimination and careful assessment of symptoms. Skin prick testing and blood tests can sometimes help identify specific allergens within semen, but results aren't always conclusive. A detailed medical history and a thorough physical examination are crucial steps.
- Skin Prick Test: A small amount of diluted semen is applied to the skin, and the area is pricked. A reaction indicates a possible allergy.
- Blood Tests: Blood tests can measure the level of specific antibodies in the blood that might indicate an allergic reaction to semen proteins.
- Elimination Diet: While not strictly a test, avoiding sexual contact for a period and gradually reintroducing it can sometimes help determine if symptoms are related to semen.
Differentiating Allergy from Other Conditions
Many conditions can mimic the symptoms of a semen allergy, making accurate diagnosis challenging. It's vital to rule out other potential causes before concluding a semen allergy. Some conditions that might present similar symptoms include infections, STIs, and other forms of irritation.
- Vaginal Infections: Yeast infections, bacterial vaginosis, and other vaginal infections can cause itching, burning, and discharge.
- Sexually Transmitted Infections (STIs): STIs can lead to various genital symptoms, including inflammation and discomfort.
- Irritants: Certain lubricants, soaps, or detergents can irritate the genitals and mimic allergy symptoms.
Treatment Options for Semen Allergy
Treatment for a semen allergy often focuses on managing symptoms and avoiding exposure to the allergen. The severity of the allergy will dictate the appropriate treatment approach. For mild reactions, over-the-counter remedies might suffice; severe reactions may require more intensive medical intervention.
- Antihistamines: Over-the-counter antihistamines can help alleviate mild symptoms like itching and hives.
- Corticosteroids: For more severe reactions, corticosteroids may be prescribed to reduce inflammation.
- Immunotherapy (Allergy Shots): In some cases, immunotherapy might be considered to desensitize the immune system to semen proteins, but this is less common for semen allergies.
Seeking Medical Advice
If you suspect you have a semen allergy, it's crucial to seek medical advice from a healthcare professional, such as a gynecologist or allergist. Self-diagnosing and treating can be risky, and a proper diagnosis ensures appropriate management of symptoms and avoidance of potential complications. They can properly assess your symptoms, conduct appropriate tests, and recommend the most suitable treatment strategy.
- Accurate Diagnosis: A healthcare professional can help determine if your symptoms are actually related to a semen allergy.
- Personalized Treatment Plan: They can create a treatment plan tailored to your specific needs and the severity of your reaction.
- Prevention Strategies: Your doctor can provide guidance on how to best avoid exposure to semen to prevent future reactions.
What are the common signs and symptoms of an allergic reaction?
Allergic reactions manifest in a wide variety of ways, depending on the allergen and the individual's sensitivity. Some reactions are mild and easily manageable, while others can be severe and life-threatening. Common mild symptoms include: sneezing, runny nose, itchy eyes, and a rash. These are often associated with allergies like pollen (hay fever) or pet dander. A more severe reaction might involve swelling, particularly of the face, lips, or tongue (angioedema). You might also experience hives (urticaria), which appear as raised, itchy welts on the skin. Difficulty breathing, wheezing, and a drop in blood pressure are indicators of a serious allergic reaction called anaphylaxis, which requires immediate medical attention. It's important to note that not everyone experiences all of these symptoms, and the severity can vary greatly even with the same allergen. Some people might only experience mild itching, while others experience a cascade of severe symptoms. If you suspect you're experiencing an allergic reaction, keeping a detailed record of your symptoms can be very helpful for your doctor in determining the cause and appropriate treatment. Gastrointestinal symptoms such as nausea, vomiting, and diarrhea can also be associated with allergies, though less frequently than skin or respiratory symptoms. It is crucial to differentiate between a simple intolerance and a true allergic reaction. While intolerance can cause discomfort, it usually doesn't involve the immune system in the same way an allergic reaction does.
How can I tell the difference between an allergy and a food intolerance?
While both allergies and intolerances cause unpleasant reactions after consuming certain foods, there's a crucial difference. Food allergies involve the body's immune system. When a person with a food allergy ingests the allergen, their immune system overreacts, releasing histamine and other chemicals that cause a range of symptoms, from mild to life-threatening. These symptoms often appear quickly, sometimes within minutes of ingestion. In contrast, food intolerances are not immune-mediated. They involve difficulty digesting a specific food, resulting in symptoms like bloating, gas, diarrhea, or stomach cramps. These symptoms usually develop more slowly, often hours after eating the problematic food. The severity of food intolerance symptoms tends to be milder than allergic reactions. It's important to remember that even though a food intolerance isn't as immediately dangerous as a food allergy, it can still significantly impact a person's quality of life. If you experience symptoms after eating certain foods, it's vital to seek professional medical advice to determine the nature of your reaction – whether it's an allergy or intolerance – and develop an appropriate management plan. Self-diagnosing can be risky, and a healthcare professional can conduct tests to distinguish between the two and offer personalized recommendations.
What kind of tests can determine if I have an allergy?
Diagnosing allergies requires a thorough evaluation by a healthcare professional, usually an allergist or immunologist. They'll start by taking a detailed medical history, asking about your symptoms, the timing of their onset, and any potential triggers. Several tests can then be performed to confirm the presence of an allergy. One common test is a skin prick test, where a small amount of allergen is applied to the skin, and the area is pricked. A raised, wheal-like reaction indicates a possible allergy. Another test is a blood test, specifically a radioallergosorbent test (RAST) or an enzyme-linked immunosorbent assay (ELISA), which measures the level of allergen-specific antibodies in your blood. These blood tests are especially useful for people who can't have skin prick tests due to medication or skin conditions. A food challenge, conducted under medical supervision, involves consuming increasing amounts of the suspected allergen to observe the body’s reaction. This is a more definitive test but carries the risk of a severe allergic reaction, so it’s only performed when necessary and in a controlled environment. The choice of test depends on several factors, including the suspected allergen, the patient's medical history, and the availability of testing resources. It's crucial to work closely with your doctor to determine the most appropriate testing strategy and to interpret the results accurately.
What should I do if I think I'm having an allergic reaction?
If you suspect you are experiencing an allergic reaction, immediate action is crucial, particularly if the symptoms are severe. Mild reactions, such as a mild rash or runny nose, might be manageable with over-the-counter antihistamines. However, if you experience symptoms like difficulty breathing, swelling of the face or throat, dizziness, or hives, seek immediate medical attention. Call emergency services immediately. If you've been diagnosed with a specific allergy and carry an epinephrine auto-injector (like an EpiPen), use it as instructed. Epinephrine is a life-saving medication that can counteract the effects of a severe allergic reaction (anaphylaxis). While waiting for medical help, keep the affected person comfortable, monitoring their breathing and vital signs. Avoid giving the person food or drink unless instructed to do so by medical personnel. After receiving emergency medical care, follow up with your allergist to discuss your experience and adjust your allergy management plan if necessary. Prevention is key to managing allergies; understanding your triggers and avoiding them whenever possible is the most effective way to prevent future reactions. Keeping a detailed record of your symptoms and potential triggers is essential in helping your doctor manage your allergies effectively. Remember, taking allergy symptoms seriously is crucial.

Deja una respuesta