How do you treat a nose allergy

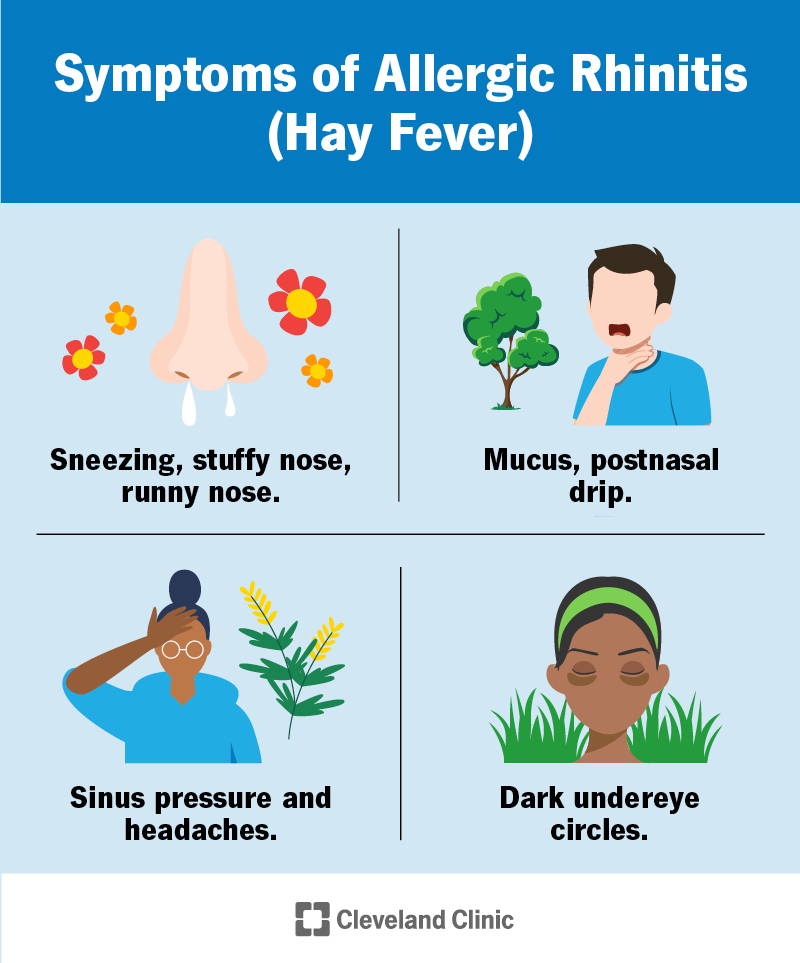
Every year, millions of people suffer from allergies, and for many, the nose is the primary target. Nasal allergies, also known as allergic rhinitis, can cause a range of unpleasant symptoms, including a runny or stuffy nose, sneezing, congestion, and itchy, watery eyes. These symptoms can make it difficult to breathe, sleep, and enjoy life to the fullest. While there is no cure for nasal allergies, there are a number of effective treatments available to help manage the symptoms.
How to Effectively Manage Your Nasal Allergies
Treating nasal allergies involves a multi-pronged approach focusing on both symptom relief and long-term allergy management. The best approach depends on the severity of your allergies and your individual triggers. It's crucial to identify your allergens to tailor your treatment plan effectively. Common triggers include pollen, dust mites, pet dander, and mold. A visit to an allergist can help determine your specific triggers and create a personalized management plan. This may involve allergy testing (skin prick test or blood test) to pinpoint the exact culprits. This allows for more targeted and effective treatment. Often a combination of methods yields the best results.
Over-the-Counter Medications
Many effective over-the-counter (OTC) medications can provide significant relief from nasal allergy symptoms. These include:
- Antihistamines: These medications block the effects of histamine, a chemical released by your body during an allergic reaction. They can effectively reduce sneezing, runny nose, and itchy eyes. Examples include cetirizine (Zyrtec), fexofenadine (Allegra), and loratadine (Claritin). Be aware that some antihistamines can cause drowsiness.
- Decongestants: These medications help to shrink swollen nasal passages, relieving stuffiness. They are available as nasal sprays (e.g., phenylephrine, oxymetazoline) or oral medications (e.g., pseudoephedrine). Avoid prolonged use of nasal decongestant sprays as they can lead to rebound congestion.
- Saline Nasal Sprays and Rinses: These are gentle ways to rinse nasal passages, flushing out allergens and irritants. They can provide relief from dryness and congestion. They are generally safe for regular use.
Prescription Medications
If OTC medications don't provide sufficient relief, your doctor may prescribe stronger medications, including:
- Nasal Corticosteroids: These are highly effective in reducing nasal inflammation and relieving symptoms like sneezing, runny nose, and congestion. Examples include fluticasone (Flonase), mometasone (Nasonex), and beclomethasone (Beconase AQ).
- Oral Corticosteroids: These are powerful anti-inflammatory medications that can be used for short periods to treat severe allergy symptoms. They are usually reserved for cases where other treatments have failed. Long-term use can have side effects, so they are generally only used for short-term bursts.
- Leukotriene Modifiers: These medications block the action of leukotrienes, chemicals involved in allergic inflammation. They can be helpful for both nasal and eye allergy symptoms.
Allergy Immunotherapy (Allergy Shots)
Allergy shots, also known as immunotherapy, are a long-term treatment option. It involves gradually introducing small amounts of your specific allergens into your body to desensitize your immune system. This can lead to a significant reduction in allergy symptoms over time. It requires regular injections over several months or years. This is generally a long term solution.
Lifestyle Changes and Environmental Control
Making changes to your lifestyle and environment can significantly reduce your exposure to allergens and lessen your symptoms:
- Monitor Pollen Counts: Pay attention to daily pollen forecasts and limit outdoor activities on high-pollen days.
- Keep Your Home Clean: Regularly dust, vacuum, and clean surfaces to minimize dust mites and pet dander. Use air purifiers with HEPA filters.
- Shower Before Bed: Removing pollen from your hair and skin can help you sleep better.
- Use Air Conditioning: Air conditioning can help filter out allergens from the air.
When to See a Doctor
It's important to see a doctor if your allergy symptoms are severe, interfering with your daily life, or not responding to over-the-counter treatments. A doctor can help you develop a comprehensive treatment plan that addresses your specific needs and may refer you to an allergist.
Severe allergy symptoms can include difficulty breathing, swelling of the face or throat, and hives. Seek immediate medical attention if you experience these.
| Treatment Type | Description | Benefits | Side Effects |
|---|---|---|---|
| Over-the-Counter Antihistamines | Oral medications that block histamine | Reduces sneezing, runny nose, itchy eyes | Drowsiness (some formulations) |
| Nasal Corticosteroids | Nasal sprays that reduce inflammation | Effective for congestion, sneezing, runny nose | Nosebleeds (rare), dryness |
| Allergy Immunotherapy | Injections to desensitize the immune system | Long-term symptom reduction | Injection site reactions, rarely serious systemic reactions |
| Saline Nasal Spray | Gentle nasal rinse | Removes irritants, moistens nasal passages | Minimal to none |
How to Effectively Manage Your Nasal Allergies
Treating nasal allergies involves a multi-pronged approach focusing on both symptom relief and long-term allergy management. The best approach depends on the severity of your allergies and your individual triggers. It's crucial to identify your allergens to tailor your treatment plan effectively. Common triggers include pollen, dust mites, pet dander, and mold. A visit to an allergist can help determine your specific triggers and create a personalized management plan. This may involve allergy testing (skin prick test or blood test) to pinpoint the exact culprits. This allows for more targeted and effective treatment. Often a combination of methods yields the best results.
Over-the-Counter Medications
Many effective over-the-counter (OTC) medications can provide significant relief from nasal allergy symptoms. These include:
- Antihistamines: These medications block the effects of histamine, a chemical released by your body during an allergic reaction. They can effectively reduce sneezing, runny nose, and itchy eyes. Examples include cetirizine (Zyrtec), fexofenadine (Allegra), and loratadine (Claritin). Be aware that some antihistamines can cause drowsiness.
- Decongestants: These medications help to shrink swollen nasal passages, relieving stuffiness. They are available as nasal sprays (e.g., phenylephrine, oxymetazoline) or oral medications (e.g., pseudoephedrine). Avoid prolonged use of nasal decongestant sprays as they can lead to rebound congestion.
- Saline Nasal Sprays and Rinses: These are gentle ways to rinse nasal passages, flushing out allergens and irritants. They can provide relief from dryness and congestion. They are generally safe for regular use.
Prescription Medications
If OTC medications don't provide sufficient relief, your doctor may prescribe stronger medications, including:
- Nasal Corticosteroids: These are highly effective in reducing nasal inflammation and relieving symptoms like sneezing, runny nose, and congestion. Examples include fluticasone (Flonase), mometasone (Nasonex), and beclomethasone (Beconase AQ).
- Oral Corticosteroids: These are powerful anti-inflammatory medications that can be used for short periods to treat severe allergy symptoms. They are usually reserved for cases where other treatments have failed. Long-term use can have side effects, so they are generally only used for short-term bursts.
- Leukotriene Modifiers: These medications block the action of leukotrienes, chemicals involved in allergic inflammation. They can be helpful for both nasal and eye allergy symptoms.
Allergy Immunotherapy (Allergy Shots)
Allergy shots, also known as immunotherapy, are a long-term treatment option. It involves gradually introducing small amounts of your specific allergens into your body to desensitize your immune system. This can lead to a significant reduction in allergy symptoms over time. It requires regular injections over several months or years. This is generally a long term solution.
Lifestyle Changes and Environmental Control
Making changes to your lifestyle and environment can significantly reduce your exposure to allergens and lessen your symptoms:
- Monitor Pollen Counts: Pay attention to daily pollen forecasts and limit outdoor activities on high-pollen days.
- Keep Your Home Clean: Regularly dust, vacuum, and clean surfaces to minimize dust mites and pet dander. Use air purifiers with HEPA filters.
- Shower Before Bed: Removing pollen from your hair and skin can help you sleep better.
- Use Air Conditioning: Air conditioning can help filter out allergens from the air.
When to See a Doctor
It's important to see a doctor if your allergy symptoms are severe, interfering with your daily life, or not responding to over-the-counter treatments. A doctor can help you develop a comprehensive treatment plan that addresses your specific needs and may refer you to an allergist.
Severe allergy symptoms can include difficulty breathing, swelling of the face or throat, and hives. Seek immediate medical attention if you experience these.
| Treatment Type | Description | Benefits | Side Effects |
|---|---|---|---|
| Over-the-Counter Antihistamines | Oral medications that block histamine | Reduces sneezing, runny nose, itchy eyes | Drowsiness (some formulations) |
| Nasal Corticosteroids | Nasal sprays that reduce inflammation | Effective for congestion, sneezing, runny nose | Nosebleeds (rare), dryness |
| Allergy Immunotherapy | Injections to desensitize the immune system | Long-term symptom reduction | Injection site reactions, rarely serious systemic reactions |
| Saline Nasal Spray | Gentle nasal rinse | Removes irritants, moistens nasal passages | Minimal to none |
How can I make my nose allergies go away?

There's no single cure for nasal allergies, but you can significantly reduce symptoms and improve your quality of life through a combination of strategies. The goal is to minimize your exposure to allergens and manage your body's reaction to them. Complete eradication is unlikely, but effective management is achievable.
Identify and Avoid Your Allergens
This is the most crucial step. Knowing what specifically triggers your allergies allows for targeted avoidance. Common allergens include pollen (trees, grasses, weeds), dust mites, pet dander, and mold. Allergy testing (skin prick test or blood test) can help pinpoint your specific triggers. Once identified, you can take steps to minimize exposure.
- Keep your home clean: Regularly dust, vacuum, and clean surfaces to reduce dust mites and pet dander.
- Use air purifiers with HEPA filters: These filters can remove airborne allergens from your home.
- Manage mold: Fix leaks promptly, use dehumidifiers in damp areas, and clean moldy areas thoroughly.
Medications for Allergy Relief
Various over-the-counter (OTC) and prescription medications can effectively manage allergy symptoms. These work through different mechanisms, either blocking histamine release (antihistamines) or reducing inflammation (corticosteroids).
- Antihistamines: These are available as pills, liquids, nasal sprays, and eye drops. They relieve sneezing, runny nose, and itchy eyes. Choose formulations based on your needs and potential side effects (e.g., drowsiness).
- Decongestants: These can help relieve nasal congestion but should be used cautiously and for short periods, as overuse can lead to rebound congestion.
- Nasal corticosteroids: These are prescription nasal sprays that reduce inflammation in the nasal passages, providing longer-lasting relief than antihistamines. They're very effective but can take a few days to show full effect.
Immunotherapy (Allergy Shots)
For those with persistent, severe allergies, immunotherapy might be an option. This involves gradually introducing increasing amounts of allergen extracts to desensitize your immune system over time. It's a long-term commitment, but can lead to significant long-term allergy relief, even after treatment is completed.
- Subcutaneous immunotherapy (SCIT): Injections administered by a healthcare professional.
- Sublingual immunotherapy (SLIT): Allergen tablets or drops placed under the tongue.
- Requires consultation with an allergist: It's crucial to discuss the risks and benefits with a specialist before starting immunotherapy.
Lifestyle Changes for Allergy Management
Beyond medication and avoidance, lifestyle changes can contribute to better allergy control. These often involve simple adjustments that can make a noticeable difference in your daily comfort.
- Showering before bed: This helps remove pollen and other allergens that may have accumulated on your skin and hair throughout the day.
- Changing clothes after being outdoors: Remove clothing that may have collected pollen and wash it separately.
- Using saline nasal rinse: This can help clear nasal passages of allergens and irritants.
When to See a Doctor
While many allergy symptoms can be managed at home, it’s important to seek medical attention if your symptoms are severe, interfere significantly with daily life, or don't respond to over-the-counter treatments. Severe allergic reactions (anaphylaxis) require immediate medical care.
- Difficulty breathing: This is a serious symptom and requires immediate medical attention.
- Severe swelling: Swelling of the face, lips, or tongue indicates a potential severe allergic reaction.
- Uncontrolled symptoms: If your symptoms persist despite using over-the-counter medications, consult a doctor or allergist.
What is the best medicine for nose allergy?

There's no single "best" medicine for nose allergies (allergic rhinitis) as the ideal treatment depends on the severity of your symptoms, your overall health, and your preferences. However, several effective options exist. Treatment often involves a combination of approaches. Over-the-counter (OTC) medications are usually the first line of defense, while prescription medications are reserved for more severe cases or when OTC options prove insufficient.
Types of Over-the-Counter Medications
Over-the-counter medications primarily consist of antihistamines and nasal corticosteroids. Antihistamines block the effects of histamine, a chemical released by your body during an allergic reaction, reducing symptoms like sneezing, itching, and runny nose. Nasal corticosteroids are sprays that reduce inflammation in the nasal passages. Choosing between these depends on your individual needs and preferences.
- Oral Antihistamines: Cetirizine (Zyrtec), fexofenadine (Allegra), loratadine (Claritin) are common choices. They are generally well-tolerated but may cause drowsiness in some individuals.
- Nasal Corticosteroids: Fluticasone (Flonase, Veramyst), mometasone (Nasonex), and others are effective at reducing nasal inflammation. They take a few days to become fully effective but are generally well-tolerated.
- Decongestants: Pseudoephedrine (Sudafed) and phenylephrine are available and can provide temporary relief from nasal congestion, but they should be used cautiously and only for short periods as prolonged use can lead to rebound congestion.
Prescription Medications for Severe Allergies
If OTC medications don't adequately manage your symptoms, your doctor may prescribe stronger medications. These include stronger nasal corticosteroids, leukotriene modifiers, and in some cases, allergy shots (immunotherapy).
- Prescription Nasal Corticosteroids: These are often stronger formulations than OTC options.
- Leukotriene Modifiers: These medications (like montelukast, Singulair) block leukotrienes, another substance involved in allergic reactions, providing relief from symptoms such as nasal congestion and coughing.
- Allergy Shots (Immunotherapy): This is a long-term treatment that involves gradually exposing your body to allergens to desensitize your immune system. It's a very effective treatment for many, but it does require multiple injections over a period of time.
Lifestyle Changes to Manage Allergies
In addition to medication, several lifestyle adjustments can help manage allergy symptoms. These non-pharmacological strategies work best when used alongside medication for comprehensive symptom management.
- Identify and Avoid Allergens: Knowing your triggers (pollens, dust mites, pet dander, etc.) is crucial. This involves allergy testing if needed.
- Improve Indoor Air Quality: Use air purifiers with HEPA filters, regularly clean your home, and use dust mite-proof covers for bedding.
- Nasal Irrigation: Rinsing your nasal passages with saline solution can help remove allergens and irritants, offering relief from congestion and stuffiness.
Considering Allergy Testing
Allergy testing is essential to accurately determine your specific triggers. Skin prick tests or blood tests can identify the substances causing your allergic reaction. This information empowers you to make informed decisions about avoidance strategies and appropriate treatment choices. Knowing your allergens helps target treatment more effectively and avoids unnecessary medication use.
- Skin Prick Test: A small amount of allergen is placed on your skin, and a prick is made to introduce it. A wheal (a raised bump) indicates a positive reaction.
- Blood Test: This test measures the levels of specific IgE antibodies in your blood, indicating sensitivity to various allergens.
- Accurate Diagnosis: Accurate allergy testing is crucial for developing a personalized and effective treatment plan, maximizing results and minimizing side effects.
When to See a Doctor
While many allergy symptoms can be managed with OTC medications, it is important to see a doctor if your symptoms are severe, don't respond to OTC treatments, or worsen over time. A doctor can provide a proper diagnosis, prescribe stronger medications if needed, and rule out other potential causes of your symptoms.
- Severe Symptoms: Difficulty breathing, swelling of the face or throat, persistent high fever.
- Ineffective OTC Treatment: If over-the-counter medications don't provide adequate relief after a reasonable trial period.
- Worsening Symptoms: If your allergy symptoms are getting progressively worse or are impacting your daily life.
How do you treat an allergic reaction to your nose?
Treatment for an allergic reaction in your nose depends on the severity of the reaction and the identified allergen. Mild reactions often respond well to over-the-counter medications and self-care strategies. However, more severe reactions may require immediate medical attention. The goal of treatment is to alleviate symptoms like sneezing, itching, runny nose, congestion, and post-nasal drip, while also managing any potential complications.
Identifying and Avoiding Allergens
The first and most important step in treating a nasal allergy is identifying the allergen triggering the reaction. Common culprits include pollen, dust mites, pet dander, and mold. Once identified, avoiding exposure becomes crucial. This may involve:
- Staying indoors on high-pollen days.
- Using air purifiers with HEPA filters to remove airborne allergens from your home.
- Regularly cleaning your home and bedding to reduce dust mites and other allergens.
Over-the-Counter Medications
Several over-the-counter medications can effectively manage nasal allergy symptoms. These include:
- Antihistamines (e.g., cetirizine, loratadine, fexofenadine): These help reduce sneezing, itching, and runny nose by blocking the effects of histamine, a chemical released during an allergic reaction.
- Nasal corticosteroids (e.g., fluticasone, mometasone): These are steroid nasal sprays that reduce inflammation in the nasal passages, thereby relieving congestion and other symptoms. They are generally more effective than oral antihistamines for nasal congestion.
- Decongestants (e.g., pseudoephedrine, phenylephrine): These temporarily relieve nasal congestion but should be used cautiously and not for extended periods, as prolonged use can lead to rebound congestion.
Prescription Medications
If over-the-counter medications prove ineffective, your doctor might prescribe stronger medications. These can include:
- Higher-potency nasal corticosteroids: These offer stronger anti-inflammatory effects than over-the-counter options.
- Leukotriene modifiers: These medications block the action of leukotrienes, substances involved in inflammation and allergic reactions. They can be particularly effective for people who don’t respond well to other treatments.
- Immunotherapy (allergy shots): This is a long-term treatment option that involves gradually introducing increasing doses of allergens to your system to build tolerance. This is a more significant commitment but can provide long-lasting relief for severe allergies.
Home Remedies and Self-Care
In addition to medication, several home remedies can help manage nasal allergy symptoms:
- Saline nasal spray or rinse: This helps to flush out allergens and irritants from the nasal passages, providing immediate relief from congestion and dryness.
- Warm compress: Applying a warm compress to the sinuses can help soothe discomfort and reduce inflammation.
- Humidifier: Using a humidifier can add moisture to the air, particularly helpful during dry winter months or when using decongestants, which can dry out nasal passages.
When to Seek Medical Attention
While many nasal allergies are easily managed at home, it's crucial to seek medical attention if:
- Symptoms are severe and don't improve with over-the-counter medications.
- You experience difficulty breathing or wheezing, which could indicate a more serious allergic reaction.
- You develop facial swelling or hives, suggesting a more widespread allergic reaction.
How long does it take for nose allergies to go away?
There's no single answer to how long nose allergies last. The duration depends on several factors, including the allergen, the severity of the allergy, and the individual's response. Allergic rhinitis, the medical term for hay fever, can be seasonal or perennial. Seasonal allergies typically last only during the time of year when specific plants release pollen (e.g., spring, summer, fall), while perennial allergies persist year-round, often triggered by indoor allergens like dust mites or pet dander.
What triggers my nose allergies?
Identifying your specific triggers is crucial for managing your symptoms. Common allergens include pollen (trees, grasses, weeds), dust mites, pet dander, mold spores, and cockroach droppings. Understanding what causes your allergies allows for targeted avoidance strategies. For example, if you're allergic to pollen, you might use air purifiers or limit outdoor activities during peak pollen times.
- Pollen: Tree, grass, and weed pollens are common culprits, varying seasonally.
- Dust mites: Microscopic creatures found in bedding, carpets, and upholstered furniture.
- Pet dander: Tiny skin flakes shed by pets, particularly cats and dogs.
How can I treat my nose allergies?
Treatment options aim to reduce symptoms and improve quality of life. These range from over-the-counter medications like antihistamines and nasal corticosteroids to prescription medications such as leukotriene inhibitors or immunotherapy (allergy shots). Choosing the right treatment depends on allergy severity and individual needs. Your doctor can help determine the most appropriate approach.
- Over-the-counter medications: Antihistamines, decongestants, and nasal sprays provide temporary relief.
- Prescription medications: Stronger antihistamines, nasal corticosteroids, and leukotriene inhibitors offer more effective symptom control.
- Immunotherapy (allergy shots): A long-term treatment that gradually desensitizes the immune system to allergens.
How long does it take for allergy medications to work?
The onset of action varies depending on the medication. Antihistamines often provide relief within an hour or two, while nasal corticosteroids may take several days or even weeks to achieve their full effect. It’s important to follow your doctor’s instructions and be patient with the medication. Consistent use is crucial for optimal results.
- Antihistamines: Rapid onset of action, typically within 30-60 minutes.
- Nasal corticosteroids: Slower onset of action, taking several days or weeks for maximum benefit.
- Decongestants: Provide immediate relief but can have rebound effects with prolonged use.
When should I seek medical attention for nose allergies?
While many allergy symptoms can be managed at home, it's essential to seek medical attention when symptoms are severe, persistent, or interfere significantly with daily life. Symptoms such as difficulty breathing, facial swelling, or severe sinus pain warrant immediate medical attention. A doctor can accurately diagnose the allergy and create a personalized treatment plan.
- Severe or persistent symptoms: Symptoms that don't respond to over-the-counter treatments.
- Difficulty breathing: A sign of a serious allergic reaction.
- Facial swelling: Indicates a potential allergic reaction requiring immediate medical care.
Can I prevent nose allergies?
While it's impossible to completely prevent allergies, you can take steps to minimize exposure to allergens. This involves strategies such as frequent cleaning, using air purifiers, avoiding known triggers, and practicing good hygiene. Prevention focuses on reducing contact with allergens to minimize symptoms. Regular allergy testing can help identify specific triggers for better management.
- Regular cleaning: Dusting, vacuuming, and washing bedding frequently.
- Air purifiers: Reducing airborne allergens in the home.
- Allergen avoidance: Identifying and avoiding specific triggers.
What are the common symptoms of a nose allergy?
Nose allergies, also known as allergic rhinitis, present a range of symptoms, with severity varying from person to person. The most common symptom is a runny nose, producing a clear, watery discharge. This is often accompanied by sneezing, which can be frequent and forceful. Many sufferers also experience itching, affecting the nose, eyes, throat, and even the roof of the mouth. Congestion is another hallmark symptom, leading to difficulty breathing through the nose and a feeling of stuffiness. Furthermore, individuals with nose allergies may experience post-nasal drip, a sensation of mucus dripping down the back of the throat. This can cause a cough, sore throat, and even contribute to ear infections. Less common symptoms include dark circles under the eyes (allergic shiners) and fatigue. The intensity of these symptoms can fluctuate depending on the allergen exposure level and the individual's sensitivity. It's crucial to note that some of these symptoms can overlap with other illnesses, making proper diagnosis essential.
What are the most effective treatments for nose allergies?
Treatment for nose allergies focuses on managing symptoms and reducing exposure to allergens. Over-the-counter (OTC) medications are often the first line of defense. These include antihistamines, which block the effects of histamine, a chemical released during an allergic reaction, thus reducing sneezing, itching, and runny nose. Decongestants, available as nasal sprays or oral medications, help to shrink swollen nasal passages and relieve congestion. Nasal corticosteroids, available as prescription nasal sprays, are highly effective in reducing inflammation and are often recommended for more severe allergies. Oral corticosteroids, while effective, are usually reserved for short-term use due to potential side effects. Allergy immunotherapy, also known as allergy shots, involves gradually exposing the body to increasing amounts of the allergen to build tolerance and reduce allergic reactions over time. This is a long-term treatment option that offers significant benefits for many individuals. In addition to medication, lifestyle changes can help. This includes regular cleaning of the home to minimize allergen exposure, avoiding known triggers, and using air purifiers. Finally, saline nasal rinses can help clear nasal passages of allergens and mucus.
When should I see a doctor about my nose allergy?
While many nose allergy symptoms can be managed at home with OTC medications, it's important to seek professional medical attention under certain circumstances. If your symptoms are severe, interfering significantly with your daily life, sleep, or work, it's best to consult a doctor. If OTC medications fail to provide adequate relief, or if your symptoms worsen despite treatment, a doctor can evaluate your condition and suggest more effective strategies. Similarly, if you experience new or unusual symptoms in conjunction with your allergy symptoms, such as fever, facial pain, or breathing difficulties, it's crucial to consult a doctor to rule out other potential causes. Furthermore, if you suspect a severe allergic reaction, characterized by difficulty breathing, swelling of the face or throat, or dizziness, seek immediate medical attention, as this could be a life-threatening situation. Regular check-ups are also recommended for individuals with persistent or recurring allergy symptoms, especially if they need to use medication frequently.
Can nose allergies be prevented?
While completely preventing nose allergies is often impossible, as they're typically caused by a genetic predisposition and exposure to environmental allergens, significant steps can be taken to minimize their impact. Identifying and avoiding known triggers is paramount. This involves identifying specific allergens like pollen, pet dander, dust mites, or mold that exacerbate your symptoms, and then taking steps to limit your exposure. This could include using air purifiers and filters in your home, regularly cleaning your living spaces, washing bedding frequently, and avoiding outdoor activities during peak pollen seasons. Maintaining good hygiene practices can also play a role. Regularly washing your hands, especially after being outdoors, can help prevent allergens from entering your body. For some individuals, allergy immunotherapy can be highly effective in reducing the severity and frequency of allergic reactions over time, representing a preventative strategy for long-term management. While complete prevention might not always be achievable, proactive strategies can significantly reduce symptom severity and improve overall quality of life for individuals struggling with nose allergies.
Deja una respuesta