How to cure allergic rhinitis permanently

Are you tired of the constant sneezing, itchy nose, and congestion that comes with allergic rhinitis? This chronic condition affects millions worldwide, and while there is no single cure-all, there are a number of things you can do to manage your symptoms and potentially eliminate them for good. In this article, we will explore the causes of allergic rhinitis and provide detailed guidance on how to prevent, treat, and potentially cure this condition permanently. By understanding the underlying mechanisms and following comprehensive treatment plans, you can regain control of your respiratory health and enjoy a life free from the limitations of allergic rhinitis.
Is There a Permanent Cure for Allergic Rhinitis? Understanding the Possibilities
Unfortunately, there's currently no known permanent cure for allergic rhinitis (hay fever). While the condition can't be completely eradicated, effective management strategies can significantly reduce symptoms and improve quality of life. The goal of treatment isn't necessarily a cure, but rather long-term control and minimizing the impact of allergies on your daily life. This involves identifying and avoiding triggers, using medication to manage symptoms, and in some cases, considering immunotherapy. While some individuals may experience remission, it's crucial to understand that the underlying allergy remains, making recurrence possible.
Identifying and Avoiding Allergens
A cornerstone of allergic rhinitis management is identifying and minimizing exposure to your specific allergens. This involves allergy testing (skin prick test or blood test) to pinpoint the culprits, which are often pollen, dust mites, pet dander, or mold. Once identified, you can take steps to avoid or minimize contact. This might include: using air purifiers, regularly cleaning your home, washing bedding frequently in hot water, wearing a mask outdoors during high pollen seasons, and avoiding contact with specific pets. Consistent avoidance is key to reducing symptom severity.
Medication Management: Controlling Symptoms
Several medications effectively control allergic rhinitis symptoms. Antihistamines block histamine, a chemical released during allergic reactions, reducing symptoms like sneezing, itching, and runny nose. Decongestants relieve nasal congestion. Nasal corticosteroids are powerful anti-inflammatory medications that reduce inflammation in the nasal passages. Leukotriene inhibitors block leukotrienes, another inflammatory chemical. Your doctor can help determine the best medication regimen for your specific needs and symptom severity. It's important to follow your doctor's instructions carefully and discuss any side effects.
Immunotherapy: Altering the Immune Response
Immunotherapy, also known as allergy shots or sublingual immunotherapy (SLIT), aims to desensitize your immune system to specific allergens over time. This involves gradually increasing exposure to small amounts of the allergen, gradually reducing your sensitivity and improving tolerance. Immunotherapy is not a quick fix, and it requires a long-term commitment, typically several months or even years. However, it can provide long-lasting relief for many individuals, significantly reducing or eliminating the need for other medications.
Lifestyle Changes for Allergy Relief
Certain lifestyle modifications can support your allergy management plan. These may include maintaining good hygiene, managing stress levels (stress can worsen allergy symptoms), getting adequate sleep, and eating a healthy diet. While not a cure, these changes can contribute to a healthier immune system and improved overall well-being, potentially reducing symptom frequency and severity.
Understanding When to Seek Medical Attention
If your allergic rhinitis symptoms are severe, interfering with your daily life, or not adequately controlled with over-the-counter medications, it's crucial to seek medical attention. Your doctor can perform a proper diagnosis, develop a personalized treatment plan, and rule out other potential conditions. They can also help manage potential complications of untreated allergic rhinitis, such as sinusitis or ear infections. Regular check-ups with your doctor are essential, especially if you are undergoing immunotherapy.
| Treatment Option | Description | Effectiveness | Side Effects |
|---|---|---|---|
| Allergen Avoidance | Identifying and minimizing exposure to allergens. | Highly variable, depends on allergen identification and avoidance success. | Minimal, mainly related to inconvenience. |
| Antihistamines | Block histamine release, reducing sneezing, itching, and runny nose. | Generally effective for many people. | Drowsiness (for some), dry mouth. |
| Nasal Corticosteroids | Reduce nasal inflammation. | Very effective, often first-line treatment. | Nosebleeds (rare), nasal irritation (sometimes). |
| Immunotherapy | Desensitizes immune system to allergens. | Can provide long-lasting relief for many. | Injection site reactions, possible systemic reactions (rare). |
Is There a Permanent Cure for Allergic Rhinitis? Understanding the Possibilities
Unfortunately, there's currently no known permanent cure for allergic rhinitis (hay fever). While the condition can't be completely eradicated, effective management strategies can significantly reduce symptoms and improve quality of life. The goal of treatment isn't necessarily a cure, but rather long-term control and minimizing the impact of allergies on your daily life. This involves identifying and avoiding triggers, using medication to manage symptoms, and in some cases, considering immunotherapy. While some individuals may experience remission, it's crucial to understand that the underlying allergy remains, making recurrence possible.
Identifying and Avoiding Allergens
A cornerstone of allergic rhinitis management is identifying and minimizing exposure to your specific allergens. This involves allergy testing (skin prick test or blood test) to pinpoint the culprits, which are often pollen, dust mites, pet dander, or mold. Once identified, you can take steps to avoid or minimize contact. This might include: using air purifiers, regularly cleaning your home, washing bedding frequently in hot water, wearing a mask outdoors during high pollen seasons, and avoiding contact with specific pets. Consistent avoidance is key to reducing symptom severity.
Medication Management: Controlling Symptoms
Several medications effectively control allergic rhinitis symptoms. Antihistamines block histamine, a chemical released during allergic reactions, reducing symptoms like sneezing, itching, and runny nose. Decongestants relieve nasal congestion. Nasal corticosteroids are powerful anti-inflammatory medications that reduce inflammation in the nasal passages. Leukotriene inhibitors block leukotrienes, another inflammatory chemical. Your doctor can help determine the best medication regimen for your specific needs and symptom severity. It's important to follow your doctor's instructions carefully and discuss any side effects.
Immunotherapy: Altering the Immune Response
Immunotherapy, also known as allergy shots or sublingual immunotherapy (SLIT), aims to desensitize your immune system to specific allergens over time. This involves gradually increasing exposure to small amounts of the allergen, gradually reducing your sensitivity and improving tolerance. Immunotherapy is not a quick fix, and it requires a long-term commitment, typically several months or even years. However, it can provide long-lasting relief for many individuals, significantly reducing or eliminating the need for other medications.
Lifestyle Changes for Allergy Relief
Certain lifestyle modifications can support your allergy management plan. These may include maintaining good hygiene, managing stress levels (stress can worsen allergy symptoms), getting adequate sleep, and eating a healthy diet. While not a cure, these changes can contribute to a healthier immune system and improved overall well-being, potentially reducing symptom frequency and severity.
Understanding When to Seek Medical Attention
If your allergic rhinitis symptoms are severe, interfering with your daily life, or not adequately controlled with over-the-counter medications, it's crucial to seek medical attention. Your doctor can perform a proper diagnosis, develop a personalized treatment plan, and rule out other potential conditions. They can also help manage potential complications of untreated allergic rhinitis, such as sinusitis or ear infections. Regular check-ups with your doctor are essential, especially if you are undergoing immunotherapy.
| Treatment Option | Description | Effectiveness | Side Effects |
|---|---|---|---|
| Allergen Avoidance | Identifying and minimizing exposure to allergens. | Highly variable, depends on allergen identification and avoidance success. | Minimal, mainly related to inconvenience. |
| Antihistamines | Block histamine release, reducing sneezing, itching, and runny nose. | Generally effective for many people. | Drowsiness (for some), dry mouth. |
| Nasal Corticosteroids | Reduce nasal inflammation. | Very effective, often first-line treatment. | Nosebleeds (rare), nasal irritation (sometimes). |
| Immunotherapy | Desensitizes immune system to allergens. | Can provide long-lasting relief for many. | Injection site reactions, possible systemic reactions (rare). |
What is the root cause of allergic rhinitis?
:max_bytes(150000):strip_icc()/allergic-rhinitis-thyroid-disease-3233154-01-a4b8fd738d4f4285a35873bac52ff39c.png)
The root cause of allergic rhinitis, commonly known as hay fever, is an overreaction of the immune system to otherwise harmless substances called allergens. These allergens trigger a cascade of events that lead to the characteristic symptoms of allergic rhinitis, such as sneezing, runny nose, itchy eyes, and nasal congestion. The immune system mistakenly identifies these allergens as threats, leading to the production of IgE antibodies. This process is highly individualized, meaning different people react to different allergens. The intensity of the allergic reaction also varies greatly depending on factors like the amount of allergen exposure and individual genetic predisposition.
Immune System Dysfunction
The fundamental problem in allergic rhinitis lies in the dysfunction of the immune system. Instead of tolerating harmless substances, the body mounts a vigorous immune response. This involves the release of various inflammatory mediators, such as histamine, leukotrienes, and prostaglandins. These mediators cause the characteristic symptoms of allergic rhinitis. The exact mechanisms behind this immune dysfunction are complex and not fully understood, but genetic predisposition plays a significant role.
- Genetic predisposition: A family history of allergies significantly increases the risk of developing allergic rhinitis.
- Immune cell activation: Specific immune cells, like mast cells and basophils, become activated upon exposure to allergens.
- Inflammatory mediator release: The activated cells release inflammatory substances causing symptoms.
Role of Allergens
Allergens are the triggers of allergic rhinitis. Common culprits include pollen (from trees, grasses, and weeds), dust mites, pet dander, and mold spores. These allergens contain proteins that are recognized by the immune system as foreign invaders. The size and concentration of the allergen, as well as the route of exposure (inhalation, ingestion, or contact), can significantly influence the severity of the reaction. Exposure to high concentrations of allergens generally leads to a more intense allergic response.
- Pollen: A major cause, especially during specific seasons.
- Dust mites: Tiny creatures found in bedding and carpets.
- Pet dander: Tiny skin flakes shed by animals.
IgE Antibody Production
When an allergen enters the body, it binds to a type of antibody called IgE. This binding process stimulates mast cells and basophils to release inflammatory mediators. The subsequent inflammatory response is responsible for the classic symptoms of allergic rhinitis. Individuals with allergic rhinitis typically have higher levels of IgE antibodies compared to individuals without allergies. Measuring IgE levels to specific allergens can be a helpful diagnostic tool.
- IgE antibody binding: Allergens trigger IgE antibody binding to mast cells.
- Mast cell degranulation: This triggers the release of histamine and other inflammatory mediators.
- Inflammatory cascade: The released mediators cause the allergic symptoms.
Environmental Factors
While genetic predisposition is crucial, environmental factors significantly influence the development and severity of allergic rhinitis. Air pollution, exposure to smoke, and certain lifestyle choices can exacerbate symptoms. Similarly, climate change is expected to affect allergen levels, potentially worsening allergy seasons. These environmental factors can interact with genetic predispositions to modulate the immune response.
- Air pollution: Can worsen allergic symptoms.
- Exposure to irritants: Smoke and other airborne irritants exacerbate allergic reactions.
- Climate change: Affects pollen production and allergen levels.
Genetic Predisposition and Family History
A strong family history of allergic diseases, including allergic rhinitis, asthma, and eczema, significantly increases the risk of developing allergic rhinitis. This highlights the importance of genetic factors in determining an individual's susceptibility to this condition. Specific genes have been identified that influence immune system function and susceptibility to allergies, but the exact genetic mechanisms involved are still being researched.
- Inherited genes: Genes that influence immune system function play a significant role.
- Family history: A strong family history significantly increases risk.
- Genetic research: Ongoing research is identifying specific genes involved in allergic rhinitis.
What is the fastest way to cure allergic rhinitis?

There is no "cure" for allergic rhinitis (hay fever), but there are ways to manage symptoms quickly and effectively. The fastest way to alleviate symptoms focuses on immediate relief, rather than a permanent solution. This typically involves a combination of approaches targeting the underlying cause (allergen avoidance) and symptom control (medications). The speed of symptom relief depends on the severity of the allergy and the individual's response to treatment. Some individuals may experience relief within minutes of using certain medications, while others might need a few days or even weeks to find the optimal treatment plan.
Over-the-Counter Medications for Fast Relief
Over-the-counter (OTC) medications offer the quickest relief for many people. These are readily available and can provide almost immediate symptom reduction. However, it's important to follow the dosage instructions carefully and consult a doctor if symptoms persist or worsen.
- Antihistamines: These block the effects of histamine, a chemical released during an allergic reaction. They are available in various forms, including tablets, capsules, and nasal sprays, each offering different onset times. Some provide faster relief than others.
- Decongestants: These help to reduce nasal congestion by shrinking swollen blood vessels in the nasal passages. They're available as nasal sprays or oral medications, with nasal sprays often providing faster relief.
- Combination Medications: Many OTC products combine antihistamines and decongestants for broader symptom relief. Read labels carefully to determine the active ingredients and their potential interactions with other medications.
Prescription Medications for More Severe Cases
If OTC medications don't provide sufficient relief, a doctor can prescribe stronger medications. These can be significantly more effective, but require a doctor's assessment and prescription.
- Nasal Corticosteroids: These are highly effective in reducing nasal inflammation and are often the first line of treatment for moderate-to-severe allergic rhinitis. While they don't offer immediate relief like antihistamines, their effect builds over time, providing significant long-term improvement in symptoms.
- Leukotriene Modifiers: These medications reduce inflammation throughout the body and can be helpful for individuals who experience persistent symptoms despite other treatments. Their effects are not instantaneous.
- Immunotherapy (Allergy Shots): This is a long-term treatment involving injections of gradually increasing doses of allergens. It aims to desensitize the immune system to allergens, reducing the severity of allergic reactions over time. It's not a quick fix, but it can significantly reduce symptoms in the long run.
Identifying and Avoiding Allergens
Identifying and avoiding allergens is crucial for long-term management. This isn't a quick solution for immediate symptom relief but dramatically impacts long-term allergy control. Understanding what triggers your symptoms is key.
- Allergy Testing: Skin prick tests or blood tests can help identify specific allergens, allowing for targeted avoidance strategies.
- Environmental Controls: Removing allergens from your home, such as dust mites, pet dander, and mold, can significantly reduce symptoms. This includes regular cleaning, using allergen-proof bedding, and maintaining good air quality.
- Seasonal Avoidance: During peak allergy seasons, staying indoors during peak pollen times, or minimizing outdoor activity during those periods, is a very important measure. You may also need to use air conditioning indoors.
Lifestyle Changes and Home Remedies
While not a direct cure, lifestyle changes and home remedies can complement medication and allergen avoidance. These can help manage symptoms naturally but aren't always fast-acting.
- Saline Nasal Rinse: This can help to flush out allergens and irritants from the nasal passages, providing some relief from congestion. It's often best done daily, or as frequently as needed.
- Humidifier: A humidifier adds moisture to the air, helping to alleviate dryness and irritation in the nasal passages. This may offer some relief from symptoms.
- Sufficient Sleep and Hydration: Adequate rest and hydration support overall immune function, possibly making you less susceptible to severe allergic reactions, though it won't offer immediate symptom relief.
Seeking Professional Medical Advice
Consulting an allergist or doctor is essential for accurate diagnosis and personalized treatment. A doctor can perform allergy testing to identify specific allergens and recommend the most appropriate course of action. While seeking immediate relief is important, a proper diagnosis and long-term management plan are crucial for effective allergy control.
- Comprehensive Evaluation: A doctor can perform a physical exam, review your medical history, and perform allergy tests to determine the causes of your symptoms.
- Personalized Treatment Plan: Based on your specific allergies and symptoms, your doctor will recommend the most suitable combination of medications, allergen avoidance strategies, and other management techniques.
- Ongoing Monitoring: Regular check-ups with your doctor allow for monitoring of your symptoms and adjustments to your treatment plan as needed.
What foods should you avoid with allergic rhinitis?
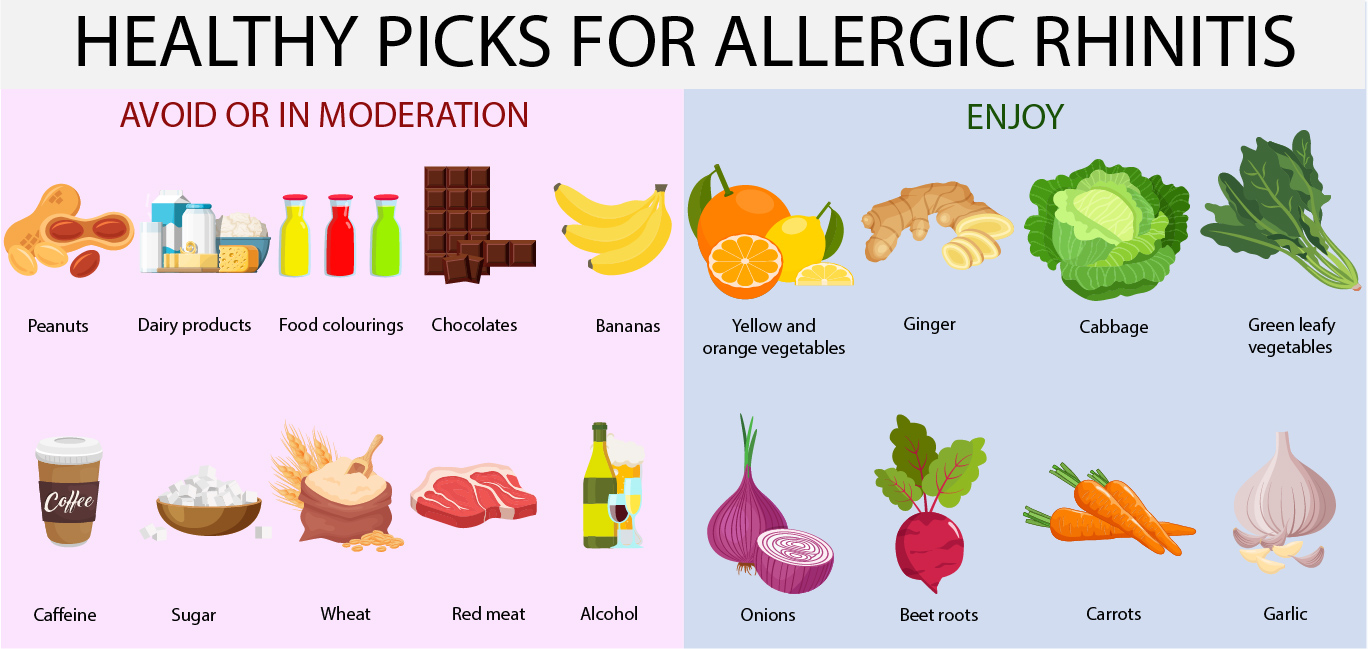
What Foods Should You Avoid with Allergic Rhinitis?
There's no single definitive list of foods to avoid for everyone with allergic rhinitis, as individual triggers vary greatly. However, certain foods are more commonly associated with triggering or exacerbating symptoms due to cross-reactivity with pollen or other allergens. This means that proteins in certain foods share similar structures to allergens like pollen, leading to an immune response. It's crucial to keep a food diary to identify your personal triggers. If symptoms worsen after eating specific foods, you may want to consider eliminating them from your diet and consulting an allergist or doctor to confirm the food allergy or intolerance and develop an appropriate management plan. Remember that avoiding suspected foods may reduce symptoms, but may not eliminate them entirely, as environmental allergens often play a significant role in allergic rhinitis.
Foods High in Histamine
Histamine is a chemical compound involved in allergic reactions, and consuming foods high in histamine can worsen symptoms of allergic rhinitis. While your body naturally produces histamine, ingesting large quantities from foods can exacerbate inflammation and increase mucus production. Therefore, monitoring your histamine intake, especially during allergy season, might be beneficial. Limiting or eliminating these foods may provide relief from congestion and other symptoms.
- Fermented foods: Sauerkraut, kimchi, yogurt, kefir, and kombucha.
- Aged cheeses: Cheddar, Swiss, Parmesan, and Brie.
- Smoked and cured meats: Bacon, ham, salami, and sausages.
Foods Containing Salicylates
Salicylates are naturally occurring compounds found in many plants. While some people are sensitive to them, a direct causal relationship between salicylate consumption and allergic rhinitis symptoms is not always clear-cut. However, those with allergies might experience increased nasal congestion and other allergic symptoms after eating high-salicylate foods. It’s important to note that salicylates are also found in many over-the-counter medications, such as aspirin. If you suspect a sensitivity, gradually eliminating high-salicylate foods and observing any changes in your symptoms is a good approach.
- Tomatoes: A common ingredient in many dishes.
- Apples: Especially those with red skin.
- Citrus fruits: Oranges, lemons, and grapefruits.
Foods Cross-Reactive with Pollen
Cross-reactivity occurs when your immune system reacts to a food allergen that shares similar proteins with an inhalant allergen, such as pollen. This can trigger allergic rhinitis symptoms even without direct exposure to the pollen. The level of cross-reactivity varies from person to person, and even the same food may have varying effects.
- Birch pollen: Cross-reacts with apples, celery, carrots, and hazelnuts.
- Ragweed pollen: Cross-reacts with melons, bananas, and cucumbers.
- Grass pollen: Cross-reacts with tomatoes, oranges, and peaches.
Foods That Can Increase Mucus Production
Certain foods can increase mucus production, potentially worsening congestion in individuals with allergic rhinitis. While not directly causing the allergic reaction, increased mucus can exacerbate existing symptoms, making breathing more difficult and overall discomfort greater. Reducing consumption of these foods during allergy season may offer some relief, although it won't address the root cause of the allergy.
- Dairy products: Milk, cheese, and ice cream.
- Wheat products: Bread, pasta, and pastries.
- Sugar-rich foods: Can increase inflammation.
Foods Containing Sulfites
Sulfites are preservatives commonly added to processed foods and drinks to prevent spoilage. Some individuals are sensitive to sulfites, experiencing symptoms similar to those of allergic rhinitis including nasal congestion, sneezing, and itching. While not strictly an allergen in the same way as pollen, sulfites can trigger an inflammatory response in sensitive individuals and should be considered for elimination or reduction in the diet if symptoms are suspected.
- Dried fruits: Often contain sulfites to prevent browning.
- Processed meats: Many processed meats contain sulfites as preservatives.
- Wine: Often contains added sulfites.
How do you calm down rhinitis?
:max_bytes(150000):strip_icc()/allergic-rhinitis-thyroid-disease-3233154-01-a4b8fd738d4f4285a35873bac52ff39c.png)
Rhinitis, or inflammation of the nasal lining, can be effectively managed through various strategies. The approach depends on the type of rhinitis (allergic, non-allergic, or medication-induced) and the severity of symptoms. However, several methods can help calm down rhinitis symptoms, focusing on reducing inflammation and relieving congestion.
Identifying and Avoiding Triggers
Identifying and avoiding your triggers is crucial for managing rhinitis. Keeping a diary to track your symptoms and potential exposures (pollens, dust mites, pet dander, specific foods, etc.) can significantly help pinpoint the causes. Once you know what triggers your rhinitis, you can actively avoid them or minimize your exposure. This proactive approach significantly reduces the frequency and intensity of your symptoms.
- Maintain a detailed diary of your symptoms and activities.
- Consider allergy testing to identify specific allergens.
- Implement measures to remove allergens from your home environment (dust mite covers, regular cleaning, air purifiers).
Over-the-Counter Medications
Numerous over-the-counter (OTC) medications can provide relief from rhinitis symptoms. Decongestants, such as pseudoephedrine or phenylephrine, can effectively reduce nasal congestion, though prolonged use can lead to rebound congestion. Antihistamines, like cetirizine or fexofenadine, are effective in controlling allergic rhinitis symptoms, particularly sneezing and itching. Nasal saline sprays can help rinse irritants from your nasal passages and relieve dryness.
- Choose decongestants cautiously, avoiding prolonged use.
- Select antihistamines based on their sedating or non-sedating properties, depending on your needs.
- Use nasal saline sprays regularly to maintain nasal moisture and clear irritants.
Lifestyle Changes
Simple lifestyle modifications can significantly impact rhinitis management. Maintaining good hydration by drinking plenty of water helps thin nasal mucus, making it easier to drain. Regular exercise can boost your immune system and overall well-being, potentially making you less susceptible to rhinitis exacerbations. Getting sufficient sleep is also vital for a strong immune system, which aids in fighting off inflammation.
- Drink plenty of water throughout the day.
- Engage in regular physical activity.
- Prioritize getting adequate sleep each night.
Prescription Medications
For more severe or persistent rhinitis symptoms, your doctor may prescribe stronger medications. Nasal corticosteroids, such as fluticasone or mometasone, are potent anti-inflammatory medications that effectively reduce nasal inflammation. Leukotriene inhibitors, like montelukast, can help control allergic inflammation, while immunotherapy (allergy shots) can desensitize your immune system to specific allergens over time.
- Nasal corticosteroids are highly effective but should be used as directed.
- Leukotriene inhibitors can be a valuable addition to other treatments.
- Immunotherapy offers long-term relief for allergic rhinitis.
Home Remedies
Several home remedies can provide temporary relief from rhinitis symptoms. Warm compresses applied to your forehead and sinuses can help relieve congestion. A warm shower or bath can create a humid environment, loosening mucus and making it easier to breathe. Using a humidifier at night can also help maintain nasal moisture. Gargling with warm saltwater can also soothe irritated throats often associated with rhinitis.
- Use warm compresses to alleviate sinus pressure.
- Take warm showers or baths to loosen nasal mucus.
- Employ a humidifier to keep nasal passages moist.
- Gently gargle with warm salt water to ease throat irritation.
Can allergic rhinitis be cured permanently?
Unfortunately, there's no single cure for allergic rhinitis that works for everyone permanently. While many treatments effectively manage symptoms and improve quality of life, achieving a complete and lasting cure is currently not possible. Allergic rhinitis, also known as hay fever, is a chronic condition triggered by an immune system response to allergens like pollen, dust mites, pet dander, or mold. This means the underlying sensitivity to these allergens generally remains. Treatments focus on reducing the severity and frequency of symptoms, such as sneezing, runny nose, itchy eyes, and congestion. These approaches can significantly improve your daily life, allowing you to live relatively symptom-free. However, it's vital to understand that if you have an allergy, you will always have that allergy, and exposure to your specific allergens will always carry the potential for symptoms. While some individuals may experience a spontaneous remission of symptoms as they age, it's not predictable and not something to rely on for a permanent cure. Successful management, using a combination of avoidance strategies, medications, and immunotherapy, is the most realistic long-term goal.
What are the most effective long-term management strategies for allergic rhinitis?
Long-term management of allergic rhinitis focuses on minimizing exposure to allergens and controlling symptoms. This involves a multi-pronged approach. Firstly, allergen avoidance is crucial. This means identifying your specific triggers (through allergy testing) and minimizing contact with them. For example, if you're allergic to pollen, staying indoors during peak pollen hours, using air filters, and regularly changing bed linens can significantly reduce exposure. Secondly, medication plays a vital role. This may include antihistamines (both oral and nasal sprays), decongestants, nasal corticosteroids (which are very effective in reducing inflammation), and leukotriene modifiers. Your doctor will help determine the best medication regimen for your specific needs and symptom severity. Thirdly, immunotherapy (allergy shots or sublingual immunotherapy) is a long-term treatment that aims to desensitize your immune system to specific allergens. This treatment involves regular injections or sublingual drops of diluted allergens over a period of several months or years, gradually increasing the dose. Immunotherapy can significantly reduce allergy symptoms and may even lead to long-term remission in some individuals, although it's not a guaranteed cure. Finally, maintaining a healthy lifestyle, including sufficient sleep, stress management, and a balanced diet, can improve your body's ability to cope with allergy symptoms. The combination of these strategies, tailored to your individual needs, is key to effective long-term management.
Is there a natural cure for allergic rhinitis?
While there's no scientifically proven "natural cure" for allergic rhinitis that provides permanent relief for everyone, several natural remedies can help manage symptoms. These approaches often address symptom relief rather than targeting the root cause of the allergy. Some common natural remedies include: nettle leaf extract (which can have antihistamine-like effects), butterbur (another herb with potential anti-inflammatory properties—but use cautiously as it may contain hepatotoxic pyrrolizidine alkaloids), quercetin (a flavonoid with antioxidant and anti-inflammatory capabilities), and probiotics (beneficial gut bacteria that might have a modulating effect on the immune system). It’s important to note that the efficacy of these remedies varies greatly among individuals. The scientific evidence supporting their effectiveness is often limited or inconclusive, and results are typically less robust than those seen with conventional medications. Furthermore, interactions with other medications or underlying health conditions are potential concerns. It’s crucial to consult your doctor before using any natural remedies, especially if you're already taking other medications or have pre-existing health issues. Natural remedies should be considered as supportive measures in conjunction with, and not as replacements for, proven medical treatments.
Can diet affect allergic rhinitis?
While diet doesn't directly cure allergic rhinitis, it can indirectly influence the severity of symptoms. A healthy diet, rich in fruits, vegetables, and whole grains, contributes to a stronger immune system. This can make your body better equipped to handle allergic reactions and potentially reduce the severity of symptoms. Conversely, certain foods can trigger or worsen symptoms for some people, although this is not directly related to the allergic reaction itself. For example, some individuals report a worsening of allergy symptoms after consuming histamine-rich foods (such as fermented foods, aged cheeses, and processed meats). The relationship between diet and allergy symptoms is complex and not fully understood. Elimination diets, where you temporarily remove certain foods from your diet to see if it affects your symptoms, are sometimes used to identify potential triggers. However, these diets should always be done under the guidance of a doctor or registered dietitian, as they can be restrictive and may lead to nutritional deficiencies if not carefully planned. Although diet is not a cure, maintaining a healthy, balanced diet as part of an overall management plan can contribute to improved well-being and potentially milder symptoms for some individuals.
Deja una respuesta