How to tell if lungs are scarred

When we breathe, our lungs take in oxygen and expel carbon dioxide. But what happens when our lungs are damaged? Scarring can occur due to various factors, such as smoking, chronic lung diseases, or infections. Understanding the signs and symptoms of lung scarring is crucial for early detection and proper medical care. This article will explore the telltale signs that may indicate lung scarring, empowering individuals to seek timely medical advice and safeguard their respiratory health.
Identifying Signs of Lung Scarring
Determining if your lungs are scarred requires a combination of medical evaluations and understanding your symptoms. It's crucial to remember that self-diagnosis is unreliable and you should always consult a healthcare professional for proper assessment and diagnosis. Lung scarring, or pulmonary fibrosis, can have a wide range of presentations, making accurate identification challenging without professional medical input.
Symptoms of Lung Scarring
Many symptoms associated with lung scarring overlap with other respiratory conditions, making it difficult to distinguish without proper medical tests. Common symptoms include a chronic dry cough, shortness of breath, especially during exertion, wheezing, chest pain or tightness, and fatigue. The severity of these symptoms can vary widely depending on the extent and location of the scarring.
Imaging Tests for Lung Scarring
High-resolution computed tomography (HRCT) scans are the most effective imaging test for detecting lung scarring. These scans provide detailed images of the lungs, revealing patterns characteristic of fibrosis, such as honeycombing (the formation of small, cyst-like air spaces) and nodules (small, rounded masses). Chest X-rays can sometimes show abnormalities suggestive of scarring, but HRCT provides much greater detail and sensitivity. Other imaging techniques like magnetic resonance imaging (MRI) might be used in some specific cases, though HRCT is more commonly employed.
Pulmonary Function Tests (PFTs)
PFTs measure how well your lungs are working. In individuals with lung scarring, PFTs may reveal reduced lung volumes (total lung capacity, forced vital capacity), decreased airflow (FEV1/FVC ratio), and impaired gas exchange. These results, combined with imaging, help to quantify the severity of lung damage and guide treatment strategies. The specific abnormalities found on PFTs can vary significantly depending on the extent and location of the scarring.
Blood Tests
While blood tests alone cannot diagnose lung scarring, they can help rule out other conditions and assess overall lung health. Blood tests may be used to check for inflammation markers, signs of infection, or other potential underlying causes of respiratory symptoms. These tests aren't diagnostic for scarring themselves, but form part of a comprehensive evaluation.
Biopsy
In some cases, a lung biopsy might be necessary to confirm the diagnosis of lung scarring. This involves removing a small tissue sample from the lung for microscopic examination. A biopsy is generally considered when other tests are inconclusive or when the physician needs to definitively identify the type of lung disease. This is an invasive procedure and is only used when absolutely necessary.
| Test | Purpose | Results in Lung Scarring |
|---|---|---|
| HRCT Scan | Detailed imaging of the lungs | Shows honeycombing, nodules, and other characteristic patterns |
| Chest X-Ray | General imaging of the lungs | May show some abnormalities, but less detailed than HRCT |
| PFTs | Measures lung function | Shows reduced lung volumes, decreased airflow, and impaired gas exchange |
| Blood Tests | Assesses overall health and rules out other conditions | May show elevated inflammation markers or other abnormalities |
| Lung Biopsy | Confirms diagnosis through tissue examination | Shows evidence of fibrosis (scar tissue formation) |
Identifying Signs of Lung Scarring
Determining if your lungs are scarred requires a combination of medical evaluations and understanding your symptoms. It's crucial to remember that self-diagnosis is unreliable and you should always consult a healthcare professional for proper assessment and diagnosis. Lung scarring, or pulmonary fibrosis, can have a wide range of presentations, making accurate identification challenging without professional medical input.
Symptoms of Lung Scarring
Many symptoms associated with lung scarring overlap with other respiratory conditions, making it difficult to distinguish without proper medical tests. Common symptoms include a chronic dry cough, shortness of breath, especially during exertion, wheezing, chest pain or tightness, and fatigue. The severity of these symptoms can vary widely depending on the extent and location of the scarring.
Imaging Tests for Lung Scarring
High-resolution computed tomography (HRCT) scans are the most effective imaging test for detecting lung scarring. These scans provide detailed images of the lungs, revealing patterns characteristic of fibrosis, such as honeycombing (the formation of small, cyst-like air spaces) and nodules (small, rounded masses). Chest X-rays can sometimes show abnormalities suggestive of scarring, but HRCT provides much greater detail and sensitivity. Other imaging techniques like magnetic resonance imaging (MRI) might be used in some specific cases, though HRCT is more commonly employed.
Pulmonary Function Tests (PFTs)
PFTs measure how well your lungs are working. In individuals with lung scarring, PFTs may reveal reduced lung volumes (total lung capacity, forced vital capacity), decreased airflow (FEV1/FVC ratio), and impaired gas exchange. These results, combined with imaging, help to quantify the severity of lung damage and guide treatment strategies. The specific abnormalities found on PFTs can vary significantly depending on the extent and location of the scarring.
Blood Tests
While blood tests alone cannot diagnose lung scarring, they can help rule out other conditions and assess overall lung health. Blood tests may be used to check for inflammation markers, signs of infection, or other potential underlying causes of respiratory symptoms. These tests aren't diagnostic for scarring themselves, but form part of a comprehensive evaluation.
Biopsy
In some cases, a lung biopsy might be necessary to confirm the diagnosis of lung scarring. This involves removing a small tissue sample from the lung for microscopic examination. A biopsy is generally considered when other tests are inconclusive or when the physician needs to definitively identify the type of lung disease. This is an invasive procedure and is only used when absolutely necessary.
| Test | Purpose | Results in Lung Scarring |
|---|---|---|
| HRCT Scan | Detailed imaging of the lungs | Shows honeycombing, nodules, and other characteristic patterns |
| Chest X-Ray | General imaging of the lungs | May show some abnormalities, but less detailed than HRCT |
| PFTs | Measures lung function | Shows reduced lung volumes, decreased airflow, and impaired gas exchange |
| Blood Tests | Assesses overall health and rules out other conditions | May show elevated inflammation markers or other abnormalities |
| Lung Biopsy | Confirms diagnosis through tissue examination | Shows evidence of fibrosis (scar tissue formation) |
How do you know if you have lung scarring?
Diagnosing lung scarring, or pulmonary fibrosis, isn't straightforward. It often requires a combination of tests and a careful review of your medical history and symptoms. There's no single test that definitively confirms lung scarring. Instead, the diagnosis is made through a process of elimination and assessment of various factors. The severity of symptoms and the extent of scarring can vary greatly from person to person. A doctor will rely on a combination of your medical history, a physical examination, imaging tests, and potentially a lung biopsy to reach a diagnosis.
Symptoms of Lung Scarring
Many individuals with mild lung scarring may experience no symptoms initially. As the scarring progresses, common symptoms include a persistent dry cough, shortness of breath, especially during exertion, fatigue, and chest pain or tightness. These symptoms can be subtle and easily mistaken for other conditions, delaying diagnosis. The severity of these symptoms is not always directly related to the extent of scarring. Some people with significant scarring may have minimal symptoms while others with less scarring may experience substantial difficulty.
- Shortness of breath (dyspnea): This is often the most prominent symptom, worsening with physical activity.
- Chronic dry cough: A persistent cough that doesn't produce mucus.
- Fatigue: Feeling unusually tired and weak.
Imaging Tests for Lung Scarring
Imaging techniques are crucial for visualizing the lungs and detecting scarring. High-resolution computed tomography (HRCT) scans are the gold standard for identifying lung scarring. These scans provide detailed images of the lungs, revealing characteristic patterns of scarring, such as honeycombing (the formation of small, cystic air spaces) or ground-glass opacities (areas of increased density). Chest X-rays can sometimes show signs of lung disease, but they are often less sensitive than HRCT scans in detecting the subtle changes associated with early-stage scarring. Other imaging tests may be used depending on individual circumstances.
- High-resolution computed tomography (HRCT) scan: Provides detailed images of the lungs to detect scarring patterns.
- Chest X-ray: A less sensitive imaging method that may show some signs of lung disease, but often misses subtle scarring.
- Pulmonary function tests (PFTs): These tests measure lung capacity and airflow to assess the severity of lung impairment.
Pulmonary Function Tests (PFTs)
PFTs assess lung function and help determine the extent of lung impairment caused by scarring. These tests measure how well your lungs take in and expel air. Results may show reduced lung volumes, impaired airflow, and decreased diffusion capacity, indicative of restrictive lung disease which is commonly associated with pulmonary fibrosis. The results of PFTs, along with other diagnostic information, help to assess the severity of the lung scarring and guide treatment decisions.
- Forced vital capacity (FVC): Measures the total amount of air you can exhale after a deep breath.
- Forced expiratory volume in 1 second (FEV1): Measures the amount of air you can exhale in one second.
- Diffusion capacity (DLCO): Measures how well oxygen moves from the lungs into the blood.
Blood Tests for Lung Scarring
While blood tests alone cannot diagnose lung scarring, they can be helpful in ruling out other conditions and identifying potential causes. Blood tests may reveal elevated inflammatory markers or markers of autoimmune diseases that can be associated with lung scarring. These tests help doctors gain a more comprehensive understanding of your overall health and can be a crucial part of the diagnostic process. The results, however, are not definitive for lung scarring.
- Complete blood count (CBC): Checks for abnormalities in blood cells.
- Inflammatory markers: Measure levels of proteins indicative of inflammation in the body.
- Autoantibody tests: Check for antibodies associated with autoimmune diseases.
Lung Biopsy for Lung Scarring
In some cases, a lung biopsy may be necessary to confirm a diagnosis of lung scarring. This involves removing a small tissue sample from the lung for microscopic examination. A lung biopsy is considered a more invasive procedure and is typically only performed when other diagnostic tests are inconclusive or when the doctor suspects a specific type of lung disease. It provides the most definitive way to identify the type and severity of lung scarring and can help differentiate between different types of interstitial lung diseases.
- Transbronchial lung biopsy (TBLB): A minimally invasive procedure where a small sample is taken through a bronchoscope.
- Surgical lung biopsy (open lung biopsy or video-assisted thoracoscopic surgery (VATS)): A more invasive procedure that may be necessary for larger samples or deeper tissue.
- Analysis of the biopsy sample: The tissue is examined under a microscope to identify the type and severity of lung scarring.
How do you check for lung scars?
How Do You Check for Lung Scars?
Lung scarring, or pulmonary fibrosis, is a condition where scar tissue forms in the lungs, hindering their ability to function properly. Detecting lung scars requires a multi-faceted approach involving several diagnostic tests. There's no single definitive test; rather, a combination of methods is used to confirm the diagnosis and assess the severity of the scarring. The process typically begins with a thorough medical history review, including symptoms and potential risk factors. This is followed by various imaging and functional tests to visualize the lung tissue and assess its capacity.
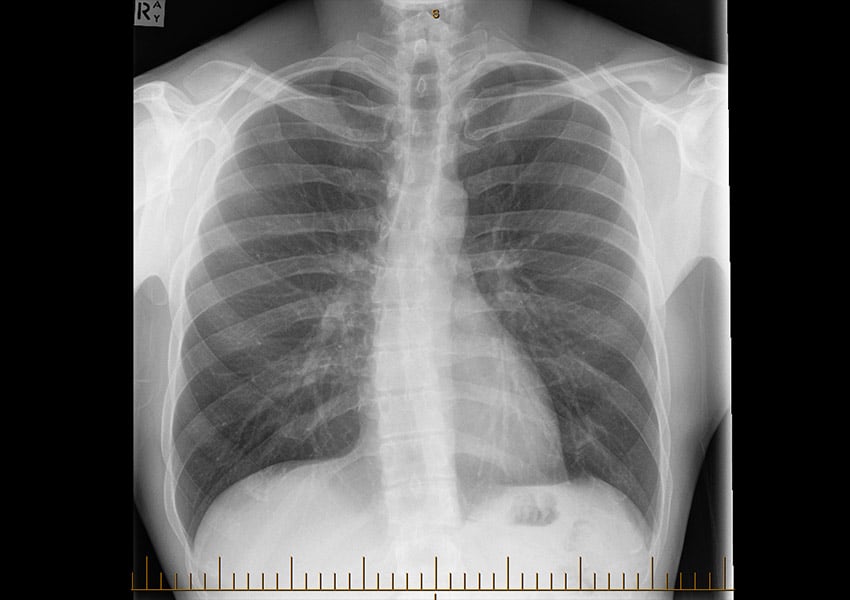
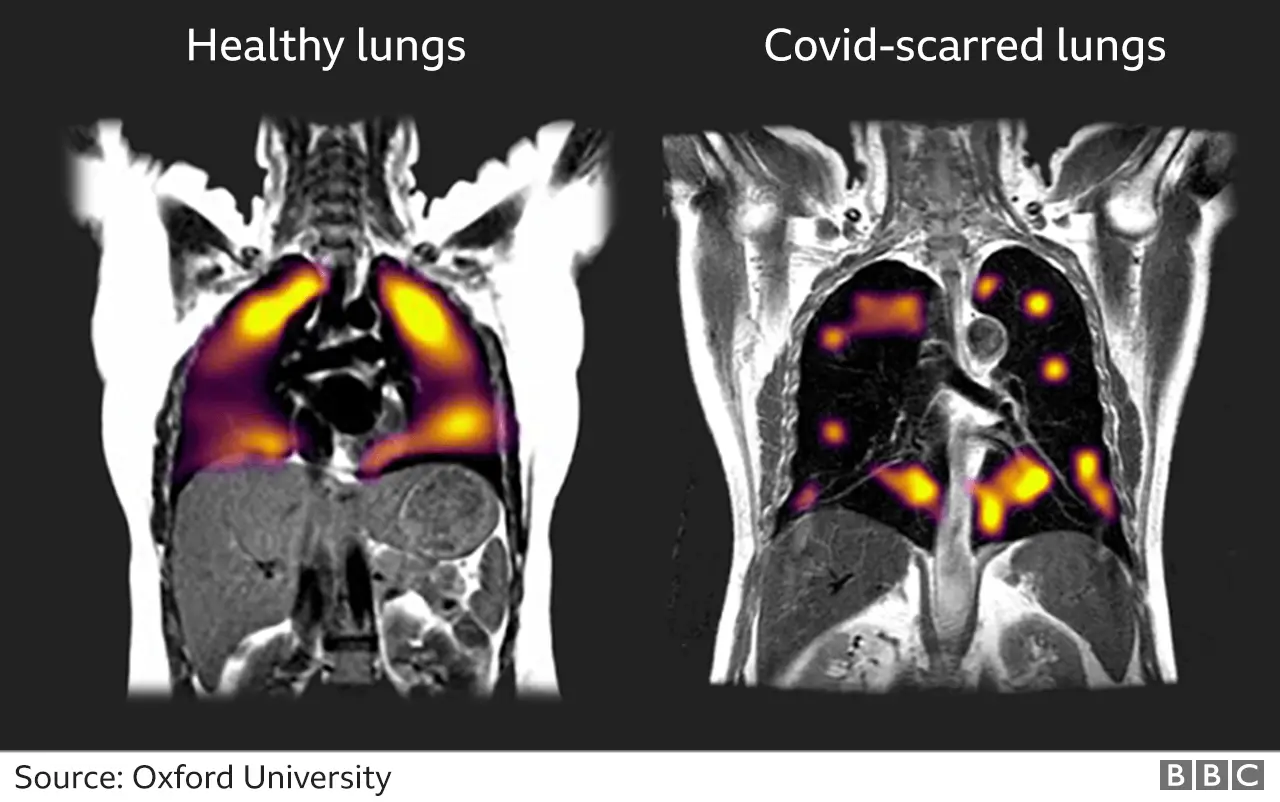
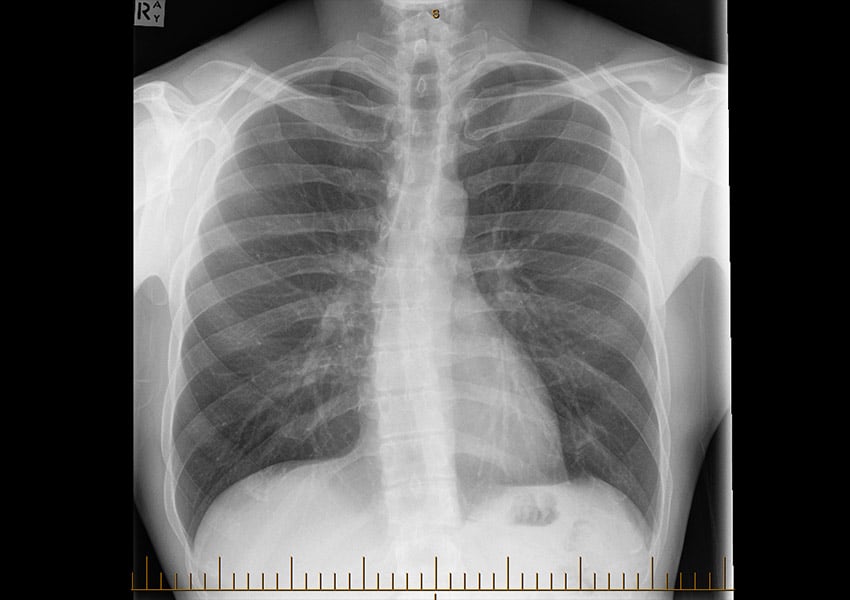
Chest X-Ray
A chest X-ray is often the initial imaging test used to look for abnormalities in the lungs. While it might not show subtle scarring, it can reveal significant changes like large areas of fibrosis that appear as opacities (white areas) on the image. However, a normal X-ray doesn't rule out scarring, particularly in its early stages. The X-ray provides a general overview and can help guide further investigations.
- Shows large areas of fibrosis as opacities.
- Provides a general overview of the lungs.
- Not sensitive enough to detect subtle or early-stage scarring.
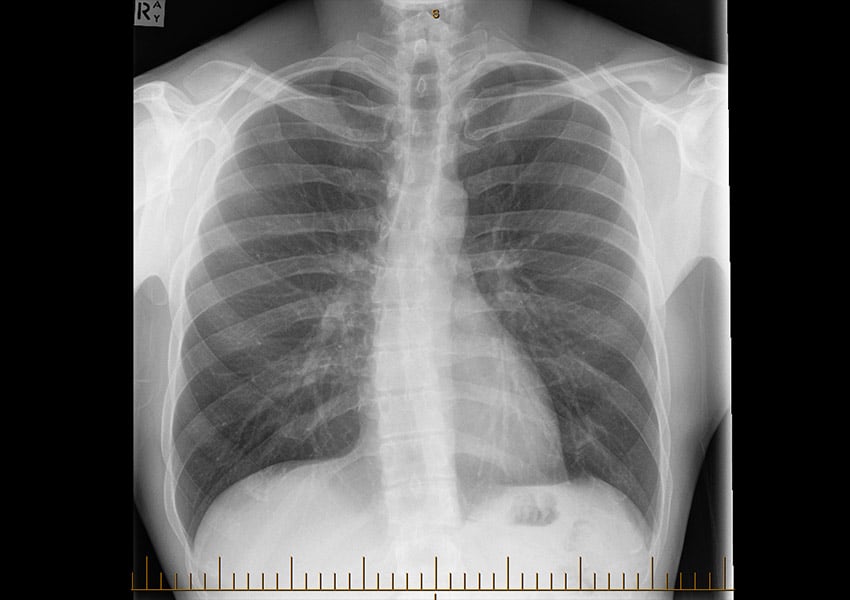
High-Resolution Computed Tomography (HRCT) Scan
HRCT is a more detailed imaging technique than a standard X-ray. It provides much higher resolution images of the lungs, allowing for the detection of smaller and more subtle lung scarring. The images reveal patterns indicative of fibrosis, such as honeycombing (a characteristic cystic appearance) and ground-glass opacities (a hazy appearance). HRCT is the gold standard for identifying and assessing the extent of lung scarring.
- Provides detailed images, revealing subtle scarring.
- Identifies characteristic patterns of fibrosis, such as honeycombing.
- Allows for precise assessment of the extent and location of scarring.
Pulmonary Function Tests (PFTs)
PFTs measure how well your lungs are functioning. These tests assess various parameters such as lung volumes (how much air your lungs can hold), airflow rates (how quickly you can breathe in and out), and diffusion capacity (how well oxygen moves from your lungs into your blood). In cases of lung scarring, PFTs often reveal restrictive lung disease, characterized by reduced lung volumes and airflow rates. This indicates that the scarred lung tissue restricts the lungs’ ability to expand fully.
- Measure lung volumes and airflow rates.
- Assess diffusion capacity of oxygen into the blood.
- Detect restrictive lung disease often associated with fibrosis.
Lung Biopsy
A lung biopsy involves removing a small sample of lung tissue for microscopic examination. This is an invasive procedure, typically reserved for cases where the diagnosis is uncertain or when detailed information about the type of scarring is needed. The biopsy can definitively identify the presence of fibrosis and its specific characteristics, which is critical in determining the underlying cause and appropriate treatment.
- Provides definitive diagnosis of fibrosis.
- Allows for detailed analysis of scar tissue characteristics.
- Identifies underlying cause of scarring in some cases.
Blood Tests
While blood tests don't directly visualize lung scars, they can help identify potential underlying causes or associated conditions. Certain blood tests may reveal markers of inflammation or autoimmunity, which can be related to some types of pulmonary fibrosis. These tests are valuable in the overall assessment and management of the condition but are not used to directly identify lung scarring itself.
- May reveal markers of inflammation or autoimmunity.
- Help identify underlying causes of pulmonary fibrosis.
- Used in conjunction with other tests for a complete assessment.
Can you tell if your lungs are damaged?
Can You Tell if Your Lungs are Damaged?
Whether you can tell if your lungs are damaged depends on the extent and type of damage. Many instances of lung damage occur subtly, with no immediately noticeable symptoms. However, some cases present with clear and significant signs. The body's response to lung damage varies widely, from asymptomatic cases to life-threatening conditions. A proper diagnosis requires professional medical evaluation. Self-diagnosis based on symptoms alone is unreliable and potentially dangerous. It's crucial to seek medical attention if you suspect lung damage.
Symptoms of Lung Damage
Various symptoms can indicate potential lung damage, but their presence doesn't confirm damage. Some individuals with significant lung issues may experience few or no noticeable symptoms, particularly in the early stages. However, common signs can include: a persistent cough, shortness of breath (dyspnea), especially during exertion, chest pain or tightness, wheezing, fatigue and weakness, and recurring respiratory infections. The severity and combination of these symptoms can vary greatly depending on the underlying cause and the extent of the damage.
- Persistent cough: A cough that lasts for several weeks or months, especially if producing mucus, may indicate an issue.
- Shortness of breath: Difficulty breathing, even at rest or during light activity, warrants medical attention.
- Chest pain or tightness: Sharp, stabbing pain, or a feeling of tightness or pressure in the chest, might signal lung problems.
Causes of Lung Damage
Lung damage can stem from a wide array of causes, both acute and chronic. Identifying the cause is vital for effective treatment. Smoking remains a leading cause of lung damage, leading to conditions like emphysema and chronic bronchitis. Environmental pollutants, including air pollution and occupational hazards, can also contribute. Infections, such as pneumonia and tuberculosis, can cause significant lung damage. Certain autoimmune diseases, genetic disorders, and prolonged exposure to irritants can also inflict damage.
- Smoking: The most common and preventable cause of lung damage.
- Environmental pollutants: Exposure to airborne toxins can lead to serious lung issues.
- Infections: Bacterial, viral, or fungal infections can severely damage lung tissue.
Diagnostic Tests for Lung Damage
Accurate diagnosis relies on various medical tests, not on self-assessment. Doctors use a range of techniques to evaluate lung health and identify the nature and extent of any damage. Chest X-rays provide images of the lungs, revealing abnormalities like infections or tumors. Computed tomography (CT) scans offer more detailed images. Pulmonary function tests (PFTs) assess how well the lungs are working. Bronchoscopy involves inserting a thin, flexible tube into the lungs to examine airways and collect samples. Blood tests may help identify infections or other underlying conditions.
- Chest X-ray: A standard imaging technique for detecting lung abnormalities.
- CT scan: Provides more detailed images than X-rays for better visualization.
- Pulmonary function tests (PFTs): Measure lung capacity and airflow.
Treatment Options for Lung Damage
Treatment for lung damage is highly dependent on the underlying cause and the severity of the damage. Treatment strategies aim to address the root cause, manage symptoms, and prevent further damage. For infections, antibiotics or antiviral medications may be prescribed. If lung damage results from smoking, quitting smoking is crucial. Inhaled medications can help manage symptoms of conditions like asthma and COPD. For more severe damage, surgery or other interventions may be necessary. Oxygen therapy might be required to supplement breathing.
- Medications: Antibiotics, antivirals, or inhaled medications may be prescribed.
- Lifestyle changes: Quitting smoking and avoiding environmental pollutants are essential.
- Surgery: In severe cases, surgery or other procedures may be required.
When to Seek Medical Attention
Prompt medical evaluation is crucial if you experience any concerning respiratory symptoms, even if they seem mild. Don't delay seeking help if you have a persistent cough, shortness of breath, chest pain, or wheezing. Regular checkups are advisable for individuals with known risk factors for lung disease, such as smokers or those exposed to environmental pollutants. Early diagnosis and treatment significantly improve outcomes in many cases of lung damage.
- Persistent cough or shortness of breath: These warrant immediate medical attention.
- Chest pain or tightness: Never ignore unexplained chest pain.
- Recurring respiratory infections: Frequent infections may indicate underlying lung issues.
Can a person survive with scarred lungs?
Whether a person can survive with scarred lungs depends heavily on the extent and location of the scarring, the underlying cause, and the individual's overall health. Scarring, or fibrosis, in the lungs replaces healthy lung tissue with stiff, non-functional tissue. This reduces the lungs' ability to expand and contract, leading to decreased oxygen intake and impaired breathing. Mild scarring might cause minimal symptoms and allow for a relatively normal life, while extensive scarring can be life-threatening.
Severity of Lung Scarring
The severity of lung scarring is a crucial factor. Mild scarring might only cause shortness of breath during exertion, while severe scarring can lead to debilitating breathlessness even at rest. The location of the scarring also matters; scarring in areas crucial for gas exchange will have a more significant impact than scarring in less critical regions. Furthermore, the underlying cause of the scarring, such as infections, autoimmune diseases, or environmental factors, can influence the prognosis.
- Severity is graded based on imaging tests and pulmonary function tests.
- Mild scarring may require minimal treatment or lifestyle adjustments.
- Severe scarring might necessitate advanced treatments like oxygen therapy, lung transplantation, or other supportive care.
Underlying Causes of Lung Scarring
The cause of the lung scarring is another key determinant of survival. Some causes, like idiopathic pulmonary fibrosis (IPF), have a poorer prognosis than others. Others, such as scarring resulting from a resolved pneumonia, might lead to minimal long-term effects. Identifying the underlying cause is critical for appropriate management and prediction of the disease's progression. Some common causes include infections (tuberculosis, pneumonia), autoimmune diseases (rheumatoid arthritis, lupus), environmental toxins (asbestos, silica), and genetic disorders.
- Infections can often be treated with antibiotics, improving prognosis if caught early.
- Autoimmune diseases often require ongoing management with immunosuppressants.
- Environmental toxins necessitate removal from exposure to prevent further damage.
Treatment Options for Scarred Lungs
Treatment focuses on managing symptoms and slowing disease progression. There's no cure for many types of lung scarring, but various treatments can improve quality of life. These include medications to reduce inflammation and slow fibrosis, supplemental oxygen, pulmonary rehabilitation programs, and lung transplantation in severe cases. Early diagnosis and intervention are essential for optimal outcomes. The effectiveness of treatment varies significantly depending on the type and severity of scarring.
- Medications like antifibrotics aim to slow down the scarring process.
- Oxygen therapy helps improve blood oxygen levels.
- Pulmonary rehabilitation enhances lung function and overall fitness.
Impact on Daily Life
The impact of scarred lungs on daily life can vary greatly depending on severity. Individuals with mild scarring may experience few limitations, while those with severe scarring might face significant challenges. Daily activities like walking, climbing stairs, and even breathing might become difficult. Quality of life can be significantly affected, requiring adjustments to work, social activities, and overall lifestyle. Supportive care, including psychological support, is crucial for coping with the challenges.
- Shortness of breath can affect physical activity and daily routines.
- Fatigue is a common symptom requiring rest and pacing of activities.
- Psychological impact can lead to anxiety, depression, and reduced quality of life.
Prognosis and Life Expectancy
The prognosis for individuals with scarred lungs is highly variable and depends on the factors already discussed. Some individuals with mild scarring might have a near-normal life expectancy, while others with severe scarring, particularly from diseases like IPF, have a significantly reduced life expectancy. Regular monitoring of lung function and adherence to treatment plans are crucial for maximizing survival and quality of life. Accurate prognostication requires careful consideration of multiple factors by a healthcare professional.
- Regular follow-up appointments allow for timely adjustments to treatment plans.
- Early detection of complications can improve outcomes.
- Prognosis varies greatly depending on the severity of lung scarring and underlying cause.
What are the common signs and symptoms of lung scarring (pulmonary fibrosis)?
Lung scarring, or pulmonary fibrosis, doesn't always present with obvious symptoms, especially in its early stages. However, as the scarring progresses, several signs and symptoms may become apparent. One of the most common is shortness of breath, which often worsens with exertion. This is because the scarred lung tissue is less elastic and less efficient at transferring oxygen into the bloodstream. Dry, hacking cough is another frequent symptom; it's often persistent and doesn't necessarily produce phlegm. Fatigue and weakness are also common, as the body struggles to get enough oxygen to function properly. Some individuals experience chest pain, which might be described as a tightness or aching sensation. Advanced stages can lead to clubbing of the fingers and toes (widening and rounding of the fingertips and toes), cyanosis (a bluish discoloration of the skin due to low oxygen levels), and weight loss. It's crucial to understand that these symptoms can be subtle and mimic other respiratory conditions, making early diagnosis challenging. If you experience any of these symptoms, particularly shortness of breath or a persistent cough, it's vital to seek medical attention to undergo proper evaluation and testing.
How is lung scarring diagnosed?
Diagnosing lung scarring requires a combination of tests and evaluations. Your doctor will likely begin by taking a thorough medical history, inquiring about your symptoms, risk factors (like exposure to environmental toxins or certain medications), and family history. A physical examination will follow, including listening to your lungs with a stethoscope to detect any abnormal sounds. Chest X-rays provide initial imaging to assess the lungs' structure and identify any abnormalities. However, X-rays might not always reveal subtle scarring. Therefore, high-resolution computed tomography (HRCT) scans are often employed to provide more detailed images of the lungs and reveal the presence and extent of scarring. Pulmonary function tests (PFTs) measure how well your lungs are functioning, assessing your lung capacity and airflow. These tests can show reduced lung volume and airflow, characteristic of pulmonary fibrosis. In some cases, a lung biopsy may be necessary. This involves removing a small sample of lung tissue for examination under a microscope to confirm the diagnosis and determine the type of scarring. Blood tests can help rule out other conditions and assess overall lung health. The diagnostic process is often iterative, involving several tests to reach a definitive conclusion.
Can lung scarring be reversed?
Unfortunately, there's currently no cure for pulmonary fibrosis, and the scarring itself is generally irreversible. The underlying cause of the scarring may be treatable in some cases, but the damage to the lung tissue itself cannot be undone. However, treatments are available to help manage symptoms, slow the progression of the disease, and improve the overall quality of life for those affected. These treatments may include medications such as anti-fibrotic drugs, which aim to slow down the scarring process. Oxygen therapy can supplement oxygen levels in the blood, alleviating shortness of breath. Pulmonary rehabilitation programs can improve lung function, exercise tolerance, and overall physical fitness. In severe cases, lung transplantation might be considered as a last resort. The focus of treatment is on managing symptoms, improving quality of life, and slowing the progression of the disease, rather than reversing the scarring itself. Regular medical check-ups are essential for monitoring disease progression and adjusting treatment as needed.
What are the risk factors for developing lung scarring?
Several factors can increase the risk of developing lung scarring (pulmonary fibrosis). Exposure to environmental toxins, such as asbestos, silica, and coal dust, is a significant risk factor. Genetic predisposition plays a role; some individuals have a genetic predisposition that makes them more susceptible to developing pulmonary fibrosis. Certain autoimmune diseases, such as rheumatoid arthritis and lupus, are associated with an increased risk. Long-term exposure to certain medications, particularly some chemotherapy drugs and certain heartburn medications, can also contribute to lung scarring. Radiation therapy to the chest area, as used in cancer treatment, can sometimes damage lung tissue. Smoking is another major risk factor, as it contributes to overall lung damage and inflammation. Age is also a significant risk factor, with the incidence of pulmonary fibrosis increasing with age. While some risk factors are unavoidable, minimizing exposure to environmental toxins, avoiding smoking, and discussing potential medication side effects with a doctor can help reduce the risk of developing this condition. Early detection and treatment are crucial in managing the disease's progression.
Deja una respuesta