Is allergy a chronic disease

Allergy, an exaggerated response of the immune system to foreign substances, is a prevalent condition affecting millions worldwide. It can manifest in various forms, ranging from mild discomforts to life-threatening anaphylaxis. For many individuals, allergies are a chronic affliction that requires ongoing management and treatment to prevent and minimize symptoms.
Is Allergy a Chronic Disease?
Whether allergies are considered chronic diseases depends on the perspective and the specific definition used. While not always life-threatening in the same way as some other chronic diseases, allergies are indeed chronic conditions for many individuals. This means they are long-lasting and typically require ongoing management. The symptoms might fluctuate in severity, but the underlying allergic response remains. The condition persists indefinitely, and although some people experience remission or less frequent episodes, complete resolution is rarely observed. The term "chronic" emphasizes the persistent nature and the need for long-term strategies to control symptoms and prevent exacerbations. Therefore, while the severity might vary, the underlying predisposition and potential for recurrent reactions solidify its classification as a chronic condition, rather than an acute illness that resolves itself.
What Defines a Chronic Disease?
A chronic disease is generally defined as a health problem that is long-lasting and usually cannot be cured completely. It often requires ongoing medical attention and lifestyle changes for management. Conditions like heart disease, diabetes, and asthma fit this definition perfectly. Allergies share these characteristics because of their enduring nature and the need for ongoing strategies, like avoidance of allergens and/or medication, to manage symptoms. While acute illnesses resolve, allergies often persist throughout a person's life, necessitating chronic management.
The Persistence of Allergic Responses
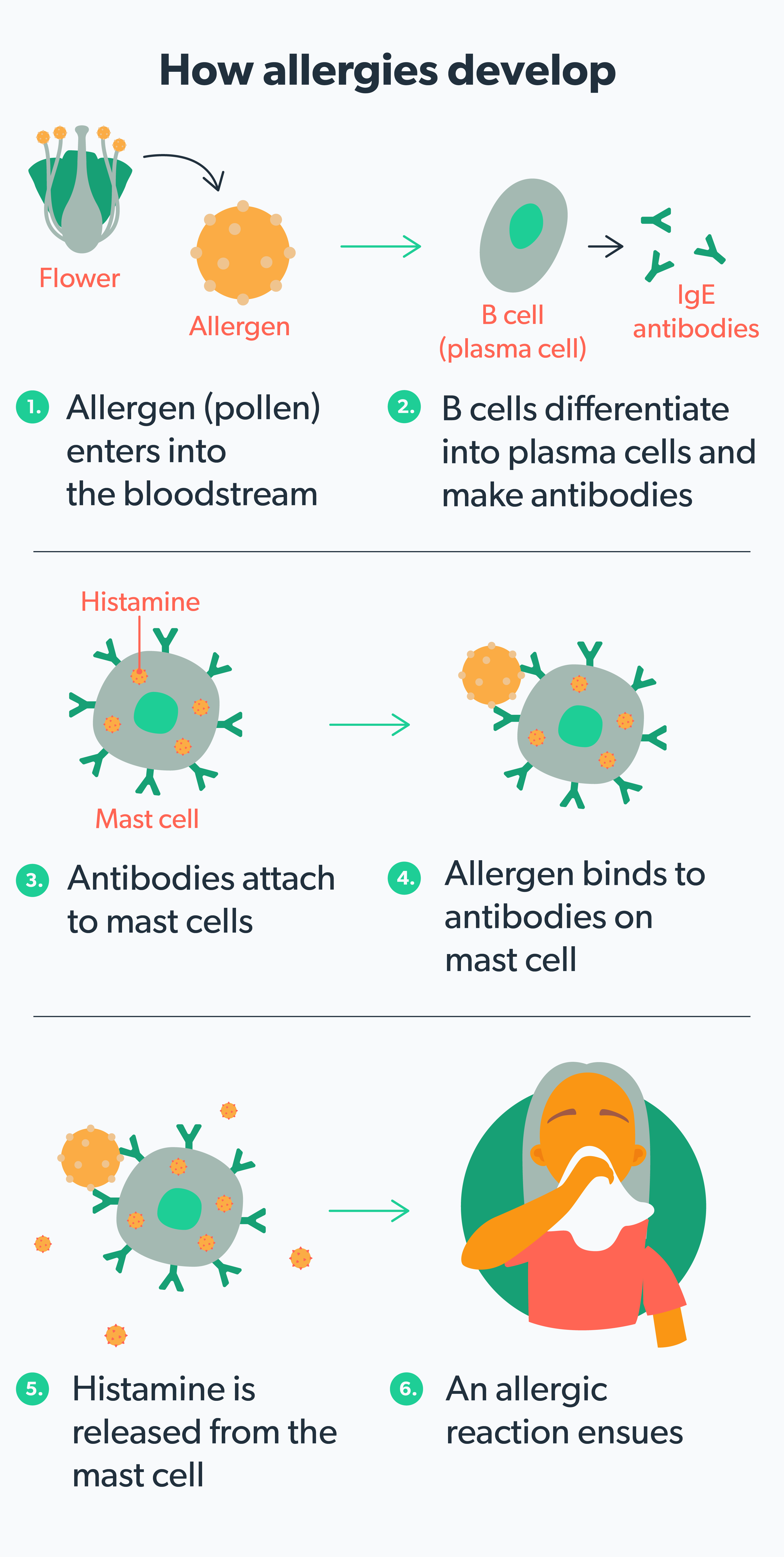
The immune system's response in allergy is the key here. Once sensitized to an allergen, the body retains this memory. Subsequent exposures trigger the release of histamine and other inflammatory mediators, leading to allergic symptoms. This memory response is what makes allergies persistent, meaning that the body's reaction to the allergen will likely recur whenever exposed. The allergic reaction itself isn't "cured," only managed.
Management, Not Cure: The Hallmark of Chronic Allergy
The treatment for allergies focuses on symptom management and preventative measures. This is typical of chronic disease management. Medication, immunotherapy, and avoidance strategies aim to reduce the frequency and severity of allergic reactions. Unlike acute illnesses with definitive cures, there is no "cure" for allergies. The focus remains on minimizing symptoms and improving the patient's quality of life, a hallmark of chronic disease care.
The Impact of Allergies on Daily Life
The significant impact of allergies on daily life further supports their classification as chronic conditions. Persistent symptoms like sneezing, coughing, congestion, skin rashes, or digestive problems can substantially affect a person's work, school, sleep, and overall well-being. This long-term disruption mirrors the impact observed in other chronic illnesses. The need for continuous attention and potential lifestyle changes to manage the disease points towards its chronic nature.
| Characteristic | Acute Illness | Chronic Allergy |
|---|---|---|
| Duration | Short-term, resolves | Long-term, persistent |
| Treatment | Cure is often possible | Symptom management and prevention |
| Impact on Daily Life | Usually temporary disruption | Significant and ongoing impact |
| Underlying Cause | Various, often infectious | Immune system overreaction to harmless substances |
| Recurrence | Unlikely after resolution | High likelihood of recurrence upon exposure |
Is Allergy a Chronic Disease?
Whether allergies are considered chronic diseases depends on the perspective and the specific definition used. While not always life-threatening in the same way as some other chronic diseases, allergies are indeed chronic conditions for many individuals. This means they are long-lasting and typically require ongoing management. The symptoms might fluctuate in severity, but the underlying allergic response remains. The condition persists indefinitely, and although some people experience remission or less frequent episodes, complete resolution is rarely observed. The term "chronic" emphasizes the persistent nature and the need for long-term strategies to control symptoms and prevent exacerbations. Therefore, while the severity might vary, the underlying predisposition and potential for recurrent reactions solidify its classification as a chronic condition, rather than an acute illness that resolves itself.
What Defines a Chronic Disease?
A chronic disease is generally defined as a health problem that is long-lasting and usually cannot be cured completely. It often requires ongoing medical attention and lifestyle changes for management. Conditions like heart disease, diabetes, and asthma fit this definition perfectly. Allergies share these characteristics because of their enduring nature and the need for ongoing strategies, like avoidance of allergens and/or medication, to manage symptoms. While acute illnesses resolve, allergies often persist throughout a person's life, necessitating chronic management.
The Persistence of Allergic Responses
The immune system's response in allergy is the key here. Once sensitized to an allergen, the body retains this memory. Subsequent exposures trigger the release of histamine and other inflammatory mediators, leading to allergic symptoms. This memory response is what makes allergies persistent, meaning that the body's reaction to the allergen will likely recur whenever exposed. The allergic reaction itself isn't "cured," only managed.
Management, Not Cure: The Hallmark of Chronic Allergy
The treatment for allergies focuses on symptom management and preventative measures. This is typical of chronic disease management. Medication, immunotherapy, and avoidance strategies aim to reduce the frequency and severity of allergic reactions. Unlike acute illnesses with definitive cures, there is no "cure" for allergies. The focus remains on minimizing symptoms and improving the patient's quality of life, a hallmark of chronic disease care.
The Impact of Allergies on Daily Life
The significant impact of allergies on daily life further supports their classification as chronic conditions. Persistent symptoms like sneezing, coughing, congestion, skin rashes, or digestive problems can substantially affect a person's work, school, sleep, and overall well-being. This long-term disruption mirrors the impact observed in other chronic illnesses. The need for continuous attention and potential lifestyle changes to manage the disease points towards its chronic nature.
| Characteristic | Acute Illness | Chronic Allergy |
|---|---|---|
| Duration | Short-term, resolves | Long-term, persistent |
| Treatment | Cure is often possible | Symptom management and prevention |
| Impact on Daily Life | Usually temporary disruption | Significant and ongoing impact |
| Underlying Cause | Various, often infectious | Immune system overreaction to harmless substances |
| Recurrence | Unlikely after resolution | High likelihood of recurrence upon exposure |
Are allergies considered chronic?
Yes, allergies are generally considered chronic conditions. This is because they represent a long-lasting hypersensitivity of the immune system to otherwise harmless substances (allergens). While symptoms might fluctuate in severity and frequency, the underlying predisposition to react to specific allergens typically persists throughout a person's life. This means that even if symptoms are well-managed or in remission for periods, the allergy itself remains a part of the individual's medical history and can potentially reactivate at any time. It's important to note that the severity and impact of allergies can vary greatly from person to person, and some individuals may experience a reduction or even disappearance of their allergic responses over time, but this does not necessarily mean the allergy itself is cured.
What Defines a Chronic Condition?
A chronic condition is generally defined as a health problem that is long-lasting and usually cannot be cured completely. This contrasts with acute conditions, which have a relatively short duration. Chronic conditions often require ongoing medical management to control symptoms and prevent complications. Allergic conditions fit this definition because they are long-lasting, often requiring ongoing management with medications, avoidance strategies, and potentially immunotherapy.
- Persistence: The underlying immune system sensitivity persists, even if symptoms are absent.
- Long-term management: Treatment often involves ongoing medication, avoidance strategies, or other interventions.
- Relapse potential: Symptoms can reappear at any time upon exposure to the allergen.
The Variability of Allergic Responses
It's crucial to understand that allergic reactions can vary widely in their severity and presentation. Some individuals might experience mild symptoms like a runny nose and itchy eyes, while others can suffer from life-threatening anaphylaxis. Even within the same individual, the severity of reactions can change over time, influenced by factors like allergen exposure, overall health, and environmental conditions. This variability doesn't change the fact that the underlying allergic condition remains chronic.
- Mild symptoms: Runny nose, sneezing, itching.
- Moderate symptoms: Hives, swelling, wheezing.
- Severe symptoms: Anaphylaxis, requiring immediate medical attention.
The Role of the Immune System in Chronic Allergies
Allergies are fundamentally driven by an overactive immune response. The immune system mistakenly identifies harmless substances (allergens) as threats, triggering a cascade of reactions that lead to the characteristic symptoms. This abnormal immune response is a core feature that defines the chronic nature of the condition. Even when symptoms are absent, the underlying immune sensitivity remains, predisposing the individual to future allergic reactions.
- Immunoglobulin E (IgE) antibodies: Play a central role in allergic reactions.
- Mast cell degranulation: Releases histamine and other inflammatory mediators.
- Inflammation: Underlying process causing allergic symptoms.
Management Strategies for Chronic Allergies
Managing chronic allergies often involves a multi-pronged approach focused on both symptom control and allergen avoidance. Effective management can significantly improve quality of life for individuals with allergies, reducing the frequency and severity of symptoms. Strategies include medications (antihistamines, corticosteroids, etc.), immunotherapy (allergy shots), and environmental control measures to minimize exposure to allergens.
- Medication: Antihistamines, decongestants, corticosteroids.
- Immunotherapy: Allergy shots or sublingual immunotherapy.
- Allergen avoidance: Identifying and avoiding triggers.
The Potential for Remission, But Not Cure
While some individuals might experience a significant reduction in allergic symptoms or even periods of remission, it's important to distinguish between remission and cure. Remission implies a temporary lessening or disappearance of symptoms, but the underlying allergic predisposition remains. A true cure for allergies is currently not possible, meaning that even with successful management, the potential for future allergic reactions persists throughout a person’s lifetime.
- Remission: Temporary reduction or absence of symptoms.
- Cure: Complete elimination of the allergic predisposition (currently not achievable).
- Continued vigilance: Even with remission, monitoring and management are important.
How to permanently get rid of allergies?
:max_bytes(150000):strip_icc()/VWH_Illustration_Preventing-and-Treating-Seasonal-Allergies_Danie-Drankwalter_Final-884166d09ac94425ad7e7a3b68a14249.jpg)
There is currently no known way to permanently get rid of allergies. Allergies are a result of your immune system mistakenly identifying harmless substances (allergens) as threats. While you can't completely eliminate this response, you can manage and significantly reduce your symptoms through various methods. These methods aim to either minimize your exposure to allergens or to desensitize your immune system to them. The effectiveness of these approaches varies depending on the individual and the specific allergen.
Immunotherapy (Allergy Shots)
Immunotherapy, also known as allergy shots, is a long-term treatment that gradually exposes you to increasing amounts of the allergen over time. This process aims to desensitize your immune system, reducing your allergic reaction to the allergen. While not a permanent cure, it can significantly reduce symptoms and even lead to long-term remission in some cases after treatment is completed.
- Gradual exposure: The process begins with small doses of the allergen and gradually increases over time.
- Maintenance phase: After the build-up phase, you'll receive maintenance doses to keep your immune system desensitized.
- Potential for long-term relief: Some individuals experience lasting relief from their allergy symptoms even after completing immunotherapy.
Allergen Avoidance
Avoiding allergens is crucial in managing allergies. This involves identifying the specific allergens triggering your reactions and minimizing your exposure to them. This approach is particularly effective for common allergens like pollen, pet dander, and dust mites. While not a cure, strict avoidance can drastically reduce symptom frequency and severity. Careful attention to detail is key.
- Identify triggers: Allergy testing can help determine specific allergens.
- Environmental controls: Using air purifiers, HEPA filters, and regular cleaning can minimize indoor allergens.
- Lifestyle changes: Avoiding specific foods, activities, or locations depending on the specific trigger.
Medication Management
Various medications can effectively control allergy symptoms. These medications don't cure allergies but provide relief from symptoms such as sneezing, itching, and congestion. Antihistamines, decongestants, and nasal corticosteroids are commonly used. It's vital to follow a doctor's prescription and guidance.
- Antihistamines: Block the effects of histamine, a chemical released during an allergic reaction.
- Decongestants: Help relieve nasal congestion.
- Nasal corticosteroids: Reduce inflammation in the nasal passages.
Lifestyle Modifications
Certain lifestyle changes can help manage allergies. Regular exercise, a healthy diet, and sufficient sleep can strengthen your immune system and may improve its tolerance to allergens. While not a direct cure, these contribute to overall well-being and potentially reduce allergy severity.
- Exercise: Improves overall health and can positively impact immune function.
- Diet: A balanced diet can support immune function.
- Sleep: Adequate sleep is vital for a healthy immune system.
Sublingual Immunotherapy (SLIT)
SLIT involves placing allergen extracts under your tongue. This method aims to desensitize your immune system in a similar manner to allergy shots, but it's generally administered at home. It is a convenient alternative but may not be effective for all types of allergies.
- Convenient home administration: Eliminates the need for frequent clinic visits.
- Gradual exposure: Similar to allergy shots, it involves a gradual increase in allergen dosage.
- Not suitable for all allergies: May not be effective for all types of allergens or for individuals with certain medical conditions.
Can adults grow out of allergies?
Can Adults Grow Out of Allergies?
While it's less common than in children, adults can sometimes experience a lessening of allergy symptoms or even a complete remission. However, it's crucial to understand that allergies don't simply disappear in adulthood for most people. The immune system's reaction to allergens, while potentially less severe over time, usually remains present. The reduction in symptoms is often linked to changes in exposure, lifestyle, or the natural progression of the immune system, rather than a complete eradication of the allergy itself. Developing tolerance to specific allergens is possible for some individuals, but this is not the same as "growing out" of the allergy entirely. It's more accurate to say that the symptoms might become less bothersome, less frequent, or less severe.
Allergy Development and Changes Over Time
The development of allergies is a complex process involving genetic predisposition and environmental triggers. While some childhood allergies, like those to milk or soy, might lessen with age as the immune system matures and the body develops tolerance, others, like pollen or pet dander allergies, often persist into adulthood. The severity of symptoms can fluctuate throughout life due to various factors, including changes in exposure levels, overall health, and even stress levels. However, the underlying immune response usually remains.
- Genetic factors play a significant role in allergy development.
- Environmental factors, such as exposure to allergens, can trigger or worsen allergies.
- Age-related changes in the immune system can influence allergy severity.
Factors Affecting Allergy Severity in Adults
Several factors can influence how allergies manifest in adults. Exposure to allergens is a major one; frequent and prolonged exposure often leads to more significant symptoms. Similarly, overall health is crucial – individuals with underlying health conditions might experience more severe reactions. Environmental factors such as air pollution or stress can also exacerbate symptoms. Finally, the type of allergen plays a role – some allergies, like pollen, are more likely to persist, while others may become less noticeable with age.
- Exposure level: High exposure generally means more severe symptoms.
- Overall health status: Weakened immune systems can lead to more intense reactions.
- Environmental factors: Pollution and stress can exacerbate allergy symptoms.
The Role of the Immune System in Adult Allergies
The immune system’s response to allergens is central to allergies. While the intensity of the immune response might decrease over time for some, it rarely vanishes completely. The body's ability to regulate inflammatory responses can improve with age in some individuals, leading to less severe symptoms. However, the underlying allergic sensitivity remains. This means that even if symptoms are minimal, exposure to significant levels of an allergen could still trigger a reaction.
- Immune system maturity can affect the intensity of allergic responses.
- Inflammation regulation plays a vital role in determining symptom severity.
- Underlying sensitivity to specific allergens usually remains present throughout adulthood.
Treatment and Management of Adult Allergies
Effective management of adult allergies is essential for maintaining a good quality of life. Allergy testing can help identify specific triggers, allowing for better targeted treatment. Treatment options range from over-the-counter antihistamines and nasal sprays to immunotherapy (allergy shots). Lifestyle modifications, such as avoiding known allergens and using air purifiers, also significantly impact symptom control. Working closely with an allergist is crucial for creating a personalized management plan.
- Allergy testing is vital for accurate diagnosis and tailored treatment.
- Medication and immunotherapy can effectively manage symptoms.
- Lifestyle changes, such as avoiding triggers, are crucial for symptom control.
Misconceptions about Outgrowing Allergies
There's a common misconception that allergies are something people simply "grow out of." While some symptoms might become less noticeable, this doesn't equate to a complete resolution. The underlying allergic sensitization persists in most cases. This means even though an adult may experience minimal or infrequent symptoms, exposure to high levels of the allergen could still trigger a significant reaction. Understanding this is critical for responsible management of allergies in adulthood.
- Symptom reduction is not the same as allergy resolution.
- Underlying sensitization often remains.
- Severe reactions can still occur despite minimal symptoms.
Why do we develop allergies?
Allergies develop due to a complex interplay of genetic predisposition and environmental factors. Our immune system, designed to protect us from harmful substances, mistakenly identifies harmless substances, such as pollen, pet dander, or certain foods, as threats. This misidentification triggers an immune response, leading to the characteristic allergic symptoms. The exact mechanisms are not fully understood, but several key processes are involved, including the role of IgE antibodies, mast cells, and genetic factors that influence immune system development and reactivity.
Genetic Predisposition
A family history of allergies significantly increases your risk of developing them yourself. This suggests a strong genetic component. While no single "allergy gene" exists, several genes influence the development and regulation of the immune system, impacting the likelihood of an allergic response. These genes can affect the production of IgE antibodies, the activity of immune cells, and the overall sensitivity of your immune system. Inherited traits that influence immune system development play a pivotal role in determining an individual's susceptibility to allergies.
- Genes influencing IgE antibody production.
- Genes affecting immune cell activity (e.g., mast cells).
- Genes regulating immune system development and maturation.
Environmental Factors
Exposure to various environmental triggers, also known as allergens, is crucial in allergy development. The timing and nature of these exposures interact with genetic predisposition. Early-life exposure to certain allergens, particularly in infants and young children, can shape the immune system's response later in life. Exposure to allergens and environmental pollutants can significantly influence the likelihood of developing allergies.
- Exposure to pollen, dust mites, pet dander, and mold.
- Air pollution and environmental toxins.
- Diet and early-life exposure to certain foods.
The Role of IgE Antibodies
Immunoglobulin E (IgE) antibodies are a type of antibody specifically involved in allergic reactions. When exposed to an allergen, the immune system produces IgE antibodies that bind to mast cells, which are immune cells found in tissues throughout the body. The binding of IgE antibodies to mast cells is a crucial step in the allergic response. When the allergen is encountered again, it binds to the IgE antibodies on mast cells, triggering the release of histamine and other inflammatory mediators.
- IgE antibody production upon initial allergen exposure.
- Binding of IgE antibodies to mast cells.
- Subsequent allergen exposure triggering mast cell degranulation.
The Hygiene Hypothesis
The hygiene hypothesis suggests that a lack of exposure to microbes and parasites in early childhood might increase the risk of allergies. Reduced exposure to diverse microorganisms may disrupt the normal development of the immune system, leading to a heightened allergic response. This theory proposes that early exposure to infections helps regulate the immune system, preventing it from overreacting to harmless substances.
- Limited exposure to bacteria and viruses in early life.
- Increased prevalence of allergies in cleaner, more hygienic environments.
- The role of gut microbiota in immune system development.
The Inflammatory Response
The release of histamine and other inflammatory mediators from mast cells causes the characteristic symptoms of an allergic reaction. These mediators act on blood vessels and other tissues, causing inflammation, itching, swelling, and other allergic manifestations. The inflammatory cascade triggered by allergen exposure is responsible for the various symptoms of allergies. The severity of the allergic response varies depending on the amount of allergen exposure, the individual's sensitivity, and the specific mediators involved.
- Histamine release and its effects on blood vessels.
- Release of other inflammatory mediators (e.g., leukotrienes, prostaglandins).
- Development of inflammation in affected tissues.
Is an allergy a chronic disease?
Whether an allergy is considered a chronic disease depends on the definition used and the severity of the allergic reaction. While some allergic reactions are short-lived and easily managed, many allergies are indeed chronic conditions. This means the underlying predisposition to react to a specific allergen remains throughout a person's life, even if symptoms are well-controlled. The chronic nature lies in the persistent presence of IgE antibodies and mast cells, primed to react to the allergen upon re-exposure. This can manifest as recurring symptoms like sneezing, itching, rash, or even life-threatening anaphylaxis. While effective treatments can significantly reduce symptom severity and frequency, the allergy itself usually doesn't disappear completely. So, while an individual might experience periods of remission or effectively manage their allergy symptoms, the underlying condition persists, making it a chronic disease in many cases. The chronic nature of allergies should not be underestimated. It can significantly impact quality of life, leading to persistent discomfort, disruptions to daily activities, and increased healthcare costs. Effective management through medication, immunotherapy, and avoidance strategies is crucial for individuals with chronic allergies to maintain their well-being.
Can allergies develop later in life?
Yes, absolutely. While many allergies develop during childhood, it's a common misconception that allergies are only a childhood problem. Allergies can, and often do, develop later in life, even in adulthood. This can be due to several factors, including new exposures to allergens, changes in the immune system, or interactions with environmental factors. For example, someone might not develop a pollen allergy until they move to an area with a high pollen count. Similarly, new sensitivities to foods or certain chemicals can emerge at any point. The immune system's complex interplay with various factors makes it possible for new allergies to appear throughout a person's lifetime. There are instances where a latent sensitivity may manifest later in life due to environmental triggers or changes in gut microbiome composition, influencing immune responses. Therefore, it's crucial to be aware that the onset of allergies is not limited to childhood, and individuals experiencing new symptoms of allergic reactions, regardless of age, should seek medical advice for proper diagnosis and management. Regular checkups and open communication with healthcare professionals are essential to monitor for and manage the development of allergies throughout life.
Are all allergies chronic conditions?
No, not all allergies are necessarily chronic conditions. While many allergies persist throughout a person's life, some allergic reactions can be transient or self-limiting. For instance, a mild reaction to a specific food might not recur upon subsequent exposure, especially if the exposure was limited. Likewise, some contact dermatitis may resolve after the skin has healed and the allergen is removed. However, it's important to distinguish between a single occurrence and a true allergic reaction. A one-time reaction that doesn't involve IgE antibodies isn't truly an allergy. The classification of an allergy as chronic hinges on the persistent nature of the immune response and the recurrence of symptoms following exposure to the allergen. Many allergies are chronic due to the sustained presence of IgE antibodies and sensitized mast cells, constantly poised to respond to the allergen. This implies that while a particular allergic reaction might be transient, the underlying allergic predisposition remains. Therefore, while some allergic reactions might not be chronic, the potential for chronicity should always be considered, especially if symptoms recur or worsen.
How are chronic allergies managed?
Managing chronic allergies involves a multi-pronged approach focused on both symptom relief and long-term disease control. Allergy management strategies are highly individualized and depend on the severity and type of allergy, as well as individual patient factors. The cornerstone of management is often allergen avoidance, which involves identifying and eliminating exposure to known allergens. This can range from simple steps like avoiding certain foods or using hypoallergenic cleaning products to more significant changes such as relocation to areas with lower pollen counts. Pharmacological interventions play a crucial role, with antihistamines, corticosteroids, and leukotriene inhibitors being commonly used to alleviate symptoms like sneezing, itching, and inflammation. For severe allergies, emergency medications like epinephrine are essential to counteract life-threatening anaphylaxis. Immunotherapy, or allergy shots, is another effective long-term treatment option that aims to desensitize the immune system to specific allergens. This approach can significantly reduce the severity and frequency of allergic reactions over time. Finally, regular monitoring and communication with an allergist are crucial for adjusting treatment plans as needed and addressing any emerging concerns. The goal of chronic allergy management is not necessarily to eliminate the allergy itself, but rather to effectively control symptoms, minimize disruptions to daily life, and prevent serious complications.

Deja una respuesta