Is cheese bad for allergies
Is cheese bad for allergies? It is a common question that many people ask. Cheese is a dairy product that is made from milk. Milk is a common allergen, so it is understandable that people with allergies might be concerned about eating cheese. However, not all cheeses are created equal. Some cheeses are lower in lactose than others, and lactose is the sugar in milk that most people with allergies react to. Additionally, some people with allergies can tolerate certain types of cheese without experiencing any symptoms. In this article, we will explore the relationship between cheese and allergies. We will discuss the different types of cheese and their lactose content, and we will provide tips for people with allergies who want to enjoy cheese.
Is Cheese a Trigger for Allergies?
Cheese and allergies are a complex relationship. While cheese itself doesn't usually cause a direct allergic reaction in the way that, say, peanuts do, it can be a significant problem for individuals with certain allergies or intolerances. This is primarily due to the ingredients used in cheese production and the potential for cross-contamination.
Milk Allergy and Cheese
The most common reason cheese might cause issues is due to a milk allergy. Cheese is made from milk, and even after processing, it can still contain milk proteins (casein and whey) that trigger allergic reactions in sensitive individuals. The intensity of the reaction varies depending on the type of cheese, the aging process, and the individual's sensitivity. Hard cheeses, due to their longer aging process, generally contain less of these proteins than soft cheeses. However, even small amounts can cause reactions ranging from mild digestive upset to severe anaphylaxis in individuals with severe milk allergies.
Lactose Intolerance and Cheese
Lactose intolerance is a different issue entirely, related to the inability to digest lactose, a sugar in milk. While not technically an allergy (which involves the immune system), lactose intolerance can cause significant digestive discomfort, including bloating, gas, and diarrhea. Hard, aged cheeses typically contain less lactose than soft, fresh cheeses, but some individuals may still experience symptoms even with small amounts.
Other Allergens in Cheese
Cheese can also contain other allergens depending on the type and production methods. Cross-contamination during manufacturing is a major concern. If the facility also processes nuts, soy, or other allergens, there's a risk of those allergens being present in the cheese, even if they aren't listed as ingredients. Additionally, some cheeses may contain additives like sulfites, which can trigger reactions in susceptible individuals. Always carefully check the ingredient list for any potential allergens.
Symptoms of Cheese-Related Reactions
Symptoms of a cheese-related reaction can range widely, depending on the cause and severity. Milk allergy symptoms can include hives, itching, swelling, breathing difficulties, and even anaphylaxis. Lactose intolerance symptoms are primarily digestive: bloating, gas, cramping, and diarrhea. Reactions to other allergens in cheese will manifest according to the specific allergen.
Diagnosing Cheese-Related Issues
If you suspect a problem with cheese, it's crucial to see a doctor or allergist for proper diagnosis. They can perform allergy testing to determine if you have a true milk allergy or an intolerance to lactose or other components. This testing is crucial for determining the cause and developing an appropriate management plan, which may involve dietary restrictions or medication.
| Allergen | Cheese Type | Potential Symptoms |
|---|---|---|
| Milk proteins (casein, whey) | All cheeses (less in aged cheeses) | Hives, itching, swelling, breathing difficulties, anaphylaxis |
| Lactose | Soft cheeses > Hard cheeses | Bloating, gas, diarrhea |
| Nuts, soy, etc. (cross-contamination) | Any cheese | Varies depending on the allergen |
| Sulfites | Some cheeses | Respiratory problems, skin reactions |
Is Cheese a Trigger for Allergies?
Cheese and allergies are a complex relationship. While cheese itself doesn't usually cause a direct allergic reaction in the way that, say, peanuts do, it can be a significant problem for individuals with certain allergies or intolerances. This is primarily due to the ingredients used in cheese production and the potential for cross-contamination.
Milk Allergy and Cheese
The most common reason cheese might cause issues is due to a milk allergy. Cheese is made from milk, and even after processing, it can still contain milk proteins (casein and whey) that trigger allergic reactions in sensitive individuals. The intensity of the reaction varies depending on the type of cheese, the aging process, and the individual's sensitivity. Hard cheeses, due to their longer aging process, generally contain less of these proteins than soft cheeses. However, even small amounts can cause reactions ranging from mild digestive upset to severe anaphylaxis in individuals with severe milk allergies.
Lactose Intolerance and Cheese
Lactose intolerance is a different issue entirely, related to the inability to digest lactose, a sugar in milk. While not technically an allergy (which involves the immune system), lactose intolerance can cause significant digestive discomfort, including bloating, gas, and diarrhea. Hard, aged cheeses typically contain less lactose than soft, fresh cheeses, but some individuals may still experience symptoms even with small amounts.
Other Allergens in Cheese
Cheese can also contain other allergens depending on the type and production methods. Cross-contamination during manufacturing is a major concern. If the facility also processes nuts, soy, or other allergens, there's a risk of those allergens being present in the cheese, even if they aren't listed as ingredients. Additionally, some cheeses may contain additives like sulfites, which can trigger reactions in susceptible individuals. Always carefully check the ingredient list for any potential allergens.
Symptoms of Cheese-Related Reactions
Symptoms of a cheese-related reaction can range widely, depending on the cause and severity. Milk allergy symptoms can include hives, itching, swelling, breathing difficulties, and even anaphylaxis. Lactose intolerance symptoms are primarily digestive: bloating, gas, cramping, and diarrhea. Reactions to other allergens in cheese will manifest according to the specific allergen.
Diagnosing Cheese-Related Issues
If you suspect a problem with cheese, it's crucial to see a doctor or allergist for proper diagnosis. They can perform allergy testing to determine if you have a true milk allergy or an intolerance to lactose or other components. This testing is crucial for determining the cause and developing an appropriate management plan, which may involve dietary restrictions or medication.
| Allergen | Cheese Type | Potential Symptoms |
|---|---|---|
| Milk proteins (casein, whey) | All cheeses (less in aged cheeses) | Hives, itching, swelling, breathing difficulties, anaphylaxis |
| Lactose | Soft cheeses > Hard cheeses | Bloating, gas, diarrhea |
| Nuts, soy, etc. (cross-contamination) | Any cheese | Varies depending on the allergen |
| Sulfites | Some cheeses | Respiratory problems, skin reactions |
What foods make allergies worse?

What Foods Make Allergies Worse?
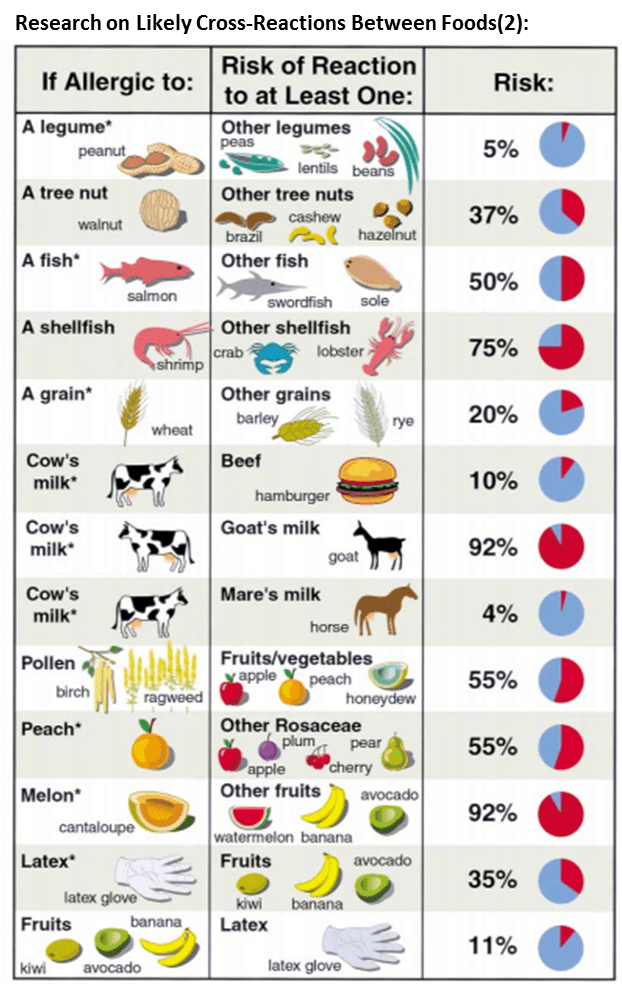
Many foods can exacerbate existing allergies or trigger allergic reactions, even if they don't directly contain the allergen. This is because some foods share similar protein structures or contain cross-reactive components that can cause the immune system to mistakenly attack them. The severity of the reaction depends on individual sensitivities and the amount consumed. It's crucial for individuals with allergies to carefully read food labels and be aware of potential cross-reactivity.
Cross-Reactive Foods
Cross-reactivity occurs when your immune system reacts to proteins in different foods that share similar structures. For example, someone allergic to pollen might experience symptoms when eating certain fruits or vegetables. This is because some plant proteins closely resemble the pollen proteins, triggering an immune response. It's not necessarily a direct allergy to the fruit itself, but a reaction to the similar protein structure.
- Birch pollen allergy: Often linked to cross-reactivity with apples, pears, carrots, hazelnuts, and celery.
- Grass pollen allergy: May trigger reactions to tomatoes, melons, and oranges.
- Ragweed allergy: Can cause reactions to melons, bananas, and cucumbers.
Foods High in Histamine
Histamine is a chemical compound naturally present in many foods. While not an allergen itself, it can worsen allergic reactions by increasing inflammation. Consuming foods high in histamine can trigger or worsen symptoms in individuals already predisposed to allergic reactions. The body normally breaks down histamine, but people with impaired histamine metabolism might experience more significant symptoms.
- Fermented foods like sauerkraut, kimchi, and yogurt.
- Aged cheeses like cheddar and parmesan.
- Smoked and cured meats.
Foods with Sulfites
Sulfites are preservatives commonly added to processed foods and drinks to maintain freshness and prevent microbial growth. Many individuals with asthma or other respiratory allergies are sensitive to sulfites, experiencing symptoms such as breathing difficulties, wheezing, or hives. It's important to note that even small amounts of sulfites can trigger a reaction in some people.
- Dried fruits
- Wine
- Processed meats
Foods Containing Additives
Certain food additives can also trigger or exacerbate allergic reactions. These aren't necessarily allergens themselves, but their presence can act as irritants and trigger inflammatory responses in sensitive individuals. Artificial colors, flavorings, and preservatives are common culprits.
- Artificial food coloring (like Yellow 5 or Red 40).
- MSG (monosodium glutamate).
- Certain preservatives like benzoates and nitrates.
The Role of Gut Health
Gut health plays a significant role in immune function. An imbalance of gut bacteria (dysbiosis) can increase intestinal permeability ("leaky gut"), allowing partially digested food proteins to enter the bloodstream. This can trigger inflammatory responses and worsen allergic symptoms. Maintaining a healthy gut microbiome through diet and lifestyle choices may help to reduce the severity of allergic reactions.
- Focusing on a diet rich in prebiotics and probiotics.
- Reducing intake of processed foods and sugar.
- Managing stress levels.
Can dairy make your allergies worse?

Dairy's potential to worsen allergies is a complex issue. While dairy itself isn't a common allergen for most people, its consumption can exacerbate existing allergies in several ways. It's not a direct causal relationship; instead, the impact is often indirect and dependent on several factors, including the type of allergy, the individual's sensitivity, and the presence of other substances in dairy products.
Dairy and Inflammation
Dairy products, particularly those with high fat content, can contribute to inflammation in the body. Inflammation is a key player in allergic reactions, and increased inflammation can worsen symptoms. This effect isn't specific to dairy; many foods can increase inflammation. For those already experiencing allergic inflammation, adding dairy might further exacerbate this response.
- Increased histamine release: Dairy can trigger histamine release in some individuals, leading to worsening allergy symptoms.
- Cross-reactivity with other allergens: Some individuals with allergies to certain proteins might also experience cross-reactivity with components found in dairy products.
- Impaired gut health: Poor gut health, often linked to dairy consumption in certain individuals, can further influence the body's immune response and contribute to heightened allergy symptoms.
Dairy and the Gut Microbiome
The gut microbiome plays a crucial role in immune regulation. Dairy consumption can alter the composition of the gut microbiome, potentially leading to an imbalance that may increase susceptibility to or worsen allergic reactions. This effect is highly variable and depends on factors such as the individual's existing gut microbiota, the type of dairy consumed, and other dietary factors.
- Changes in gut bacteria: Dairy intake can influence the abundance of certain bacteria species which influence immune responses.
- Increased gut permeability: In some individuals, dairy consumption may increase intestinal permeability ("leaky gut"), allowing allergens to enter the bloodstream more easily.
- Altered immune cell activity: Imbalances in the gut microbiome may modify the activity of immune cells, contributing to an increased allergic response.
Dairy and Food Additives
Many processed dairy products contain additives such as preservatives, artificial colors, and flavorings. These additives can be potent allergens or irritants for many people, regardless of any direct dairy-related effect. The presence of such additives in dairy products can significantly complicate the identification of the source of allergic reactions.
- Artificial coloring: Many dairy products contain artificial colors that are known allergens.
- Preservatives: Preservatives are common in many processed dairy products and can irritate sensitive individuals.
- Flavorings: Artificial flavorings may trigger allergy symptoms in individuals.
Dairy and Existing Respiratory Allergies
Individuals with existing respiratory allergies, such as asthma or rhinitis, might find that their symptoms worsen after consuming dairy. Dairy consumption can increase mucus production in some people, potentially exacerbating respiratory issues. This correlation may be indirect; increased inflammation from dairy could contribute to airway constriction and heightened sensitivity to other allergens.
- Increased mucus production: Dairy can trigger an increase in mucus production, exacerbating respiratory conditions.
- Airway inflammation: Dairy-induced inflammation can contribute to airway constriction and breathing difficulties.
- Increased sensitivity to airborne allergens: The inflammatory response triggered by dairy could increase sensitivity to airborne allergens and increase symptom severity.
Dairy and Other Allergies
The relationship between dairy consumption and other allergies is not always straightforward. While dairy itself is rarely the direct cause of an allergy, it can potentially interact with other allergens to worsen symptoms. For example, an individual with a nut allergy might experience a more severe reaction if they consume dairy along with the nut allergen. This effect is linked to interactions within the immune system and can be highly variable.
- Increased IgE levels: In certain individuals, dairy consumption can increase the production of IgE antibodies, contributing to a more severe allergic response.
- Enhanced inflammatory response: Dairy can enhance the inflammatory response to other allergens, leading to more severe symptoms.
- Delayed reaction: Some individuals may experience a delayed allergic reaction when dairy is consumed in conjunction with another allergen.
Is cheese bad for histamine?
Cheese and histamine intolerance have a complex relationship. While cheese itself contains histamine, the amount varies significantly depending on several factors. Aged cheeses generally contain higher levels of histamine than fresh cheeses due to the fermentation process. This process involves bacterial action that produces histamine as a byproduct. However, the presence of histamine in cheese isn't the sole determining factor in whether it will trigger a reaction. Individual sensitivity to histamine plays a crucial role. Some people with histamine intolerance might tolerate small amounts of even aged cheeses, while others may experience symptoms even from low-histamine varieties. Additionally, the cheese's tyramine content also contributes to potential symptoms. Tyramine, another biogenic amine, can exacerbate symptoms in individuals sensitive to both histamine and tyramine. Therefore, a simple "yes" or "no" answer is insufficient. A more accurate assessment necessitates considering individual tolerance levels, the type of cheese, and the interaction of various biogenic amines within the cheese.
Histamine Content in Different Cheeses
The histamine concentration varies dramatically across different types of cheese. Hard, aged cheeses tend to be higher in histamine than soft, fresh cheeses. This is because aging involves longer periods of bacterial activity and fermentation. The longer the aging process, the higher the potential for histamine production. Conversely, fresh cheeses, produced with less time for bacterial fermentation, typically contain lower levels of histamine. However, even within these categories, there can be substantial variation.
- Hard Cheeses (High Histamine): Cheddar, Parmesan, Swiss
- Semi-Hard Cheeses (Moderate Histamine): Gouda, Monterey Jack
- Soft Cheeses (Lower Histamine): Fresh Mozzarella, Feta (variations exist)
Individual Sensitivity and Histamine Intolerance
The impact of cheese on individuals with histamine intolerance is highly personalized. One person's tolerance level is different from another's. Some individuals might experience adverse reactions even from low-histamine cheeses, while others can tolerate moderate levels of histamine-containing cheeses without issue. Factors such as gut health, DAO enzyme activity (the enzyme responsible for breaking down histamine), and the overall health of the individual all influence how the body reacts to histamine-containing foods like cheese. It's essential to track your own reactions to determine your personal tolerance level.
- DAO Enzyme Activity: Lower activity can lead to increased histamine sensitivity.
- Gut Microbiome: A healthy gut microbiome can better manage histamine.
- Individual Thresholds: Histamine tolerance varies widely among individuals.
Tyramine's Role in Cheese and Histamine Intolerance
Cheese contains not only histamine but also tyramine, another biogenic amine. Tyramine can act synergistically with histamine, potentially worsening symptoms in individuals sensitive to both substances. Tyramine contributes to the vasoconstrictive effects associated with histamine, leading to potential symptoms such as headaches, increased blood pressure, and heart palpitations. The combination of high histamine and high tyramine content in some aged cheeses can create a considerable challenge for individuals with histamine intolerance.
- Synergistic Effects: Histamine and tyramine can work together to increase symptoms.
- Vasoconstriction: Both amines can constrict blood vessels, leading to headaches.
- Increased Blood Pressure: Tyramine, in particular, can elevate blood pressure.
Other Factors Affecting Histamine Levels in Cheese
Beyond aging and cheese type, other factors influence the histamine content of cheese. The production method, storage conditions, and even the breed of animal used to produce the milk can all play a role. For example, cheeses made with raw milk might contain higher levels of histamine than those made with pasteurized milk due to the presence of naturally occurring bacteria. Similarly, improper storage can lead to increased bacterial growth and, consequently, higher histamine levels. This underlines the complexity of assessing the histamine content of cheese and its impact on individuals with histamine intolerance.
- Raw vs. Pasteurized Milk: Raw milk can lead to higher histamine levels.
- Storage Conditions: Improper storage encourages bacterial growth and histamine production.
- Manufacturing Processes: Variations in cheese-making can affect histamine content.
Testing and Management of Histamine Intolerance
Managing histamine intolerance involves a multifaceted approach. This can begin with identifying trigger foods through a process of elimination and careful food journaling. Many people with histamine intolerance find that limiting their intake of aged cheeses is beneficial. However, relying solely on eliminating specific foods might not be enough. Supplementing with DAO enzyme and addressing underlying gut health issues might also prove necessary for effective management. Consulting a doctor or registered dietitian knowledgeable about histamine intolerance is highly recommended.
- Food Journaling: Tracking food intake and symptoms can help identify triggers.
- Dietary Elimination: Restricting high-histamine foods, including certain cheeses.
- DAO Enzyme Supplements: Increasing DAO enzyme activity to break down histamine.
What not to eat in an allergy?
What Not to Eat in an Allergy
What you should avoid eating depends entirely on the specific allergen you are allergic to. There's no single blanket answer. An allergy to peanuts is vastly different from a dairy allergy, for example. Knowing your specific allergens is paramount. This information should come from a doctor or allergist via allergy testing. Improperly identifying or managing food allergies can lead to serious health consequences, including anaphylaxis, a life-threatening reaction. Always read food labels carefully, as ingredients can vary between brands and even batches of the same product. If you are unsure about an ingredient, err on the side of caution and avoid it.
Foods to Avoid Based on Specific Allergens
This section will delve into specific allergens and provide examples of what to avoid. Careful reading of labels is crucial, as even trace amounts of allergens can trigger reactions in susceptible individuals. Always check the ingredient list and be aware of potential cross-contamination during processing and preparation. Always carry your epinephrine auto-injector (like an EpiPen) if your doctor has recommended it, especially if eating outside your home.
- Dairy: Avoid milk, cheese, yogurt, butter, cream, whey, casein, and lactose. This includes hidden dairy in processed foods like bread, sauces, and desserts.
- Peanuts: Avoid all peanut products, including peanut butter, peanut oil, and any foods that may have been processed in facilities that also process peanuts (due to cross-contamination).
- Tree Nuts: This includes almonds, walnuts, cashews, pecans, hazelnuts, pistachios, and macadamia nuts. Like peanuts, cross-contamination is a major concern.
- Soy: Soybeans, soy milk, soy sauce, tofu, tempeh, and edamame should all be avoided. Look out for soy lecithin as an ingredient.
- Eggs: Avoid eggs in any form, including whole eggs, egg whites, and egg yolks. This also includes foods containing egg powder or other egg products.
Hidden Allergens in Processed Foods
Many processed foods contain hidden allergens. Manufacturers are required to list allergens on labels, but it's crucial to read them carefully. Additives and processing aids can contain allergens, even if the main ingredient doesn't. Always be aware of terms like "may contain," as this indicates a potential for cross-contamination.
- Check for "May Contain" Statements: These statements indicate a potential for cross-contamination during processing.
- Examine Ingredient Lists Thoroughly: Pay close attention to all ingredients, not just the main ones. Many allergens can hide in unexpected places.
- Understand Cross-Contamination: Be aware that even trace amounts of allergens can be dangerous.
Reading Food Labels Effectively
Food labels are your best defense against accidental allergen exposure. Learn to decipher them effectively. Understanding ingredient lists and allergen labeling is key to safe eating.
- Identify the Allergen Declaration: This statement usually lists the top eight most common allergens (milk, eggs, peanuts, tree nuts, soy, wheat, fish, and shellfish).
- Look for "May Contain" Statements: These are crucial to avoid potential cross-contamination.
- Compare Labels: Different brands might have different ingredients, even for the same product.
Managing Allergens When Eating Out
Dining out poses extra challenges for those with allergies. Always inform the server about your allergies. This allows them to take appropriate precautions and help to avoid accidental exposure.
- Inform the Server: Clearly and explicitly state your allergies to the server.
- Ask About Preparation Methods: Inquire about how the food is prepared to avoid cross-contamination.
- Double-Check the Order: Before eating, confirm the order to ensure it meets your dietary restrictions.
Emergency Preparedness
Having an action plan in case of an allergic reaction is essential. This includes knowing how to identify symptoms, having access to epinephrine (if prescribed), and understanding when to seek immediate medical attention.
- Carry an EpiPen (if prescribed): This is a life-saving medication for severe allergic reactions.
- Know the Symptoms of Anaphylaxis: This includes hives, swelling, difficulty breathing, and dizziness.
- Have a Plan for Emergency Care: Know how to contact emergency services and what steps to take in case of a reaction.
Can cheese trigger allergic reactions?
Yes, cheese can absolutely trigger allergic reactions in susceptible individuals, although it's less common than allergies to other foods like nuts or shellfish. The proteins found in cheese are the primary culprits. Different types of cheese will contain varying amounts and types of proteins depending on the milk source (cow, goat, sheep) and the cheesemaking process. For example, someone allergic to cow's milk might experience an allergic reaction to cheddar cheese, while someone with a goat milk allergy might react to chèvre. The reaction can manifest in various ways, ranging from mild symptoms like itching or hives to more severe reactions involving swelling (angioedema), difficulty breathing, or even anaphylaxis, a life-threatening condition. It's important to note that the severity of the reaction can vary depending on the individual, the amount of cheese consumed, and the specific proteins present. A person might be able to tolerate small amounts of certain cheeses, while larger quantities or different types could lead to a significant reaction. Careful attention to ingredient labels is crucial, as some cheeses may contain additives or other allergens that can exacerbate symptoms. If you suspect a cheese allergy, it's vital to consult with an allergist for proper diagnosis and management.
What are the common symptoms of a cheese allergy?
Symptoms of a cheese allergy can range widely in severity and presentation. Mild reactions often involve skin irritation, such as itching, hives (urticaria), redness, or eczema. The affected area may feel warm or swollen. Some individuals may experience gastrointestinal distress, including nausea, vomiting, diarrhea, or stomach cramps. More severe symptoms can include respiratory issues, such as shortness of breath, wheezing, coughing, or tightness in the chest. In rare but serious cases, a cheese allergy can trigger anaphylaxis, a life-threatening condition characterized by a rapid drop in blood pressure, swelling of the throat and tongue (making breathing difficult), dizziness, and loss of consciousness. It's vital to understand that the timing of symptoms can vary. Reactions can occur within minutes of consuming cheese or might be delayed for several hours. The onset and severity of symptoms can also vary significantly based on factors like the amount of cheese ingested, the individual's sensitivity, and the specific type of cheese consumed. Any suspected allergic reaction to cheese, regardless of severity, warrants immediate medical attention.
Is it possible to have a cheese intolerance instead of an allergy?
Yes, it's definitely possible to have a cheese intolerance rather than a true allergy. While a cheese allergy involves an immune system response to cheese proteins, an intolerance is often related to the digestive system's inability to properly break down certain components of cheese, such as lactose. Lactose intolerance is a very common issue, affecting a significant portion of the adult population. Lactose is a sugar found in milk, and cheese, being a dairy product, contains varying amounts of lactose depending on the type and aging process. Symptoms of lactose intolerance often involve digestive discomfort, including bloating, gas, abdominal pain, and diarrhea. These symptoms are generally less severe than those associated with a true allergy and usually don't involve respiratory or cardiovascular symptoms. It's also possible to have an intolerance to other components of cheese such as casein, a milk protein. In some cases, both an allergy and an intolerance can coexist, making it challenging to pinpoint the exact cause of the reaction. Consulting a doctor or allergist can help differentiate between a cheese allergy and an intolerance.
How can I avoid cheese if I have an allergy?
Avoiding cheese if you have an allergy requires careful attention to detail and proactive measures. Thoroughly reading food labels is crucial, as cheese can be a hidden ingredient in many processed foods, such as sauces, soups, baked goods, and even some salad dressings. Be especially aware of terms like "dairy," "whey," "casein," and "milk solids" which could indicate the presence of cheese or other dairy products. When eating out, clearly communicate your allergy to the server and chef to ensure your food is prepared safely. Ask about ingredients and preparation methods to avoid cross-contamination. It is also advisable to always carry an epinephrine auto-injector (EpiPen) if you've experienced severe allergic reactions to cheese. Furthermore, learning about alternative foods can help you enjoy a diverse diet while avoiding cheese. There are many delicious cheese substitutes available, including plant-based cheeses made from nuts, soy, or other ingredients. Remember, even a small amount of cheese can cause a reaction in some individuals, so vigilance and careful planning are essential for managing a cheese allergy.

Deja una respuesta