What feels like allergies but isn't

Suffering from itchy eyes, runny nose, and congestion? You might assume it's allergies, but it may not be. There are a number of other conditions that can mimic allergy symptoms, making it difficult to pinpoint the exact cause of your discomfort.
What Feels Like Allergies, But Isn't: Identifying the Culprits
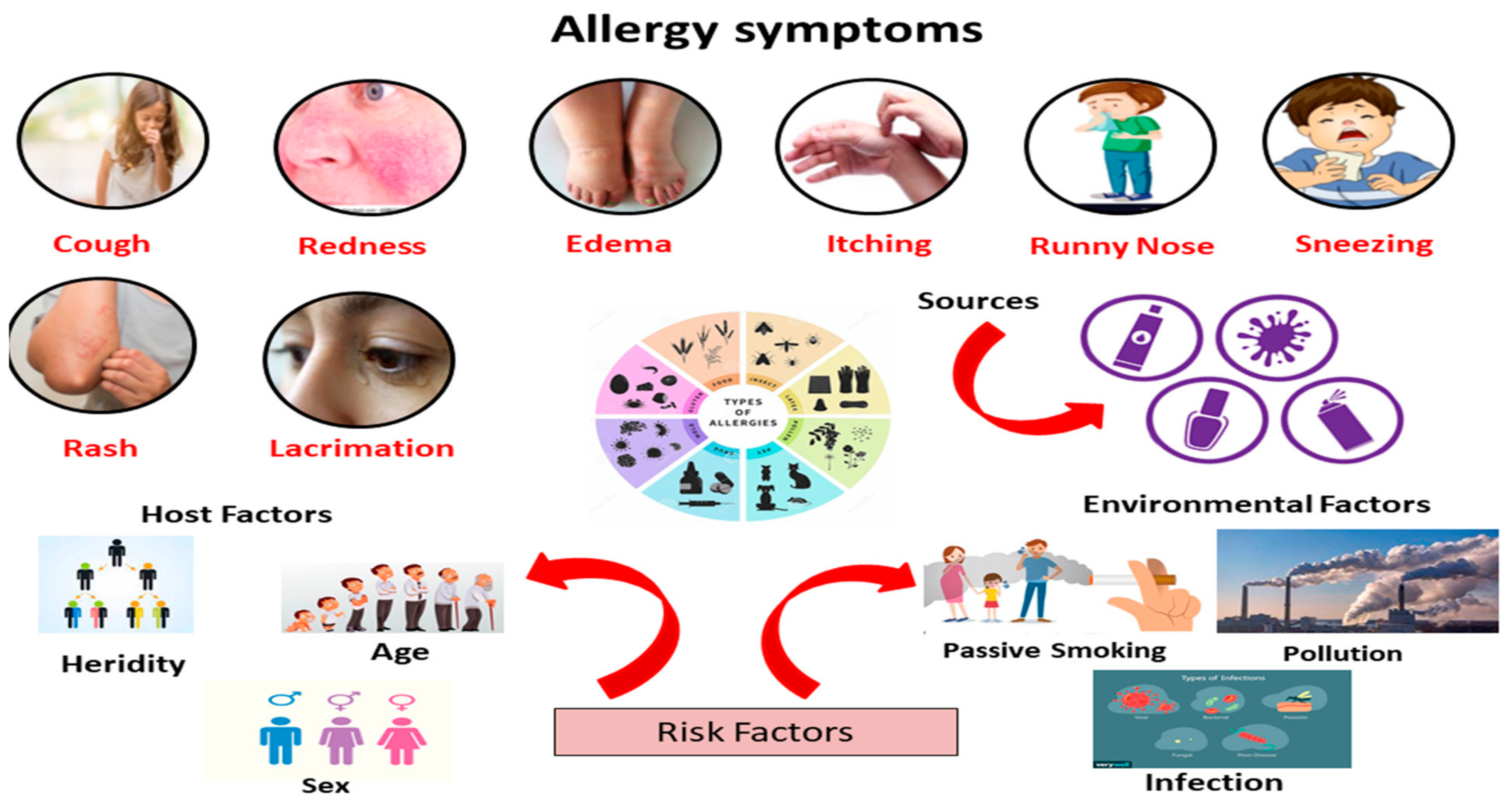
Many conditions mimic allergic reactions, making diagnosis challenging. Symptoms like sneezing, coughing, itchy eyes, and a runny nose are commonly associated with allergies, but they can also stem from various other sources. Understanding these differentials is crucial for effective treatment and management.
Non-Allergic Rhinitis
Non-allergic rhinitis is a common condition that causes similar symptoms to allergies, such as runny nose, stuffy nose, sneezing, and itchy eyes. However, unlike allergies, it's not triggered by an immune response to an allergen. Instead, it can be caused by various factors, including irritants (like dust or smoke), hormonal changes, certain medications, or environmental factors like changes in temperature or humidity. The key difference is the absence of IgE antibodies, which are typically elevated in allergic rhinitis. Treatment focuses on managing symptoms through medications like nasal sprays and antihistamines, tailored to the underlying cause.
Sinusitis
Sinusitis, or a sinus infection, involves inflammation of the sinuses. Symptoms can overlap significantly with allergies, including facial pain or pressure, congestion, cough, and fever. However, sinusitis is often caused by a viral, bacterial, or fungal infection, rather than an allergic reaction. Diagnosis typically involves a physical exam and sometimes imaging studies. Treatment may include antibiotics (for bacterial infections), decongestants, and pain relievers.
Common Cold
The common cold is another frequent culprit mistaken for allergies. While allergies can cause a runny nose and sneezing, the common cold often presents with additional symptoms such as a sore throat, cough, body aches, and fever. The common cold is caused by viruses, and unlike allergies, doesn't typically involve a prolonged, seasonal pattern of symptoms. Treatment is primarily supportive, focusing on rest and symptom relief.
Environmental Irritants
Exposure to environmental irritants like dust mites (although not technically an allergen for everyone), pet dander, mold, smoke, and strong perfumes can cause symptoms very similar to allergies. Unlike true allergies, the body's immune system isn't directly involved. These irritants directly trigger inflammation in the nasal passages and airways, leading to symptoms such as itching, sneezing, and watery eyes. Management focuses on avoiding exposure to the irritants.
Certain Medications
Some medications can produce side effects that mimic allergic symptoms. For example, certain blood pressure medications, ACE inhibitors, can cause a dry cough. Aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) can trigger nasal congestion and other symptoms in some individuals. If you suspect a medication is causing allergy-like symptoms, consult your doctor to discuss alternative options.
| Condition | Key Symptoms | Cause | Treatment |
|---|---|---|---|
| Non-Allergic Rhinitis | Runny nose, stuffy nose, sneezing, itchy eyes | Irritants, hormonal changes, medications | Nasal sprays, antihistamines |
| Sinusitis | Facial pain/pressure, congestion, cough, fever | Viral, bacterial, or fungal infection | Antibiotics (if bacterial), decongestants, pain relievers |
| Common Cold | Runny nose, sneezing, sore throat, cough, body aches, fever | Viruses | Rest, symptom relief |
| Environmental Irritants | Itching, sneezing, watery eyes | Dust, pet dander, mold, smoke, perfumes | Avoidance |
| Medication Side Effects | Vary depending on medication | Specific medications | Change medication or manage symptoms |
What Feels Like Allergies, But Isn't: Identifying the Culprits
Many conditions mimic allergic reactions, making diagnosis challenging. Symptoms like sneezing, coughing, itchy eyes, and a runny nose are commonly associated with allergies, but they can also stem from various other sources. Understanding these differentials is crucial for effective treatment and management.
Non-Allergic Rhinitis
Non-allergic rhinitis is a common condition that causes similar symptoms to allergies, such as runny nose, stuffy nose, sneezing, and itchy eyes. However, unlike allergies, it's not triggered by an immune response to an allergen. Instead, it can be caused by various factors, including irritants (like dust or smoke), hormonal changes, certain medications, or environmental factors like changes in temperature or humidity. The key difference is the absence of IgE antibodies, which are typically elevated in allergic rhinitis. Treatment focuses on managing symptoms through medications like nasal sprays and antihistamines, tailored to the underlying cause.
Sinusitis
Sinusitis, or a sinus infection, involves inflammation of the sinuses. Symptoms can overlap significantly with allergies, including facial pain or pressure, congestion, cough, and fever. However, sinusitis is often caused by a viral, bacterial, or fungal infection, rather than an allergic reaction. Diagnosis typically involves a physical exam and sometimes imaging studies. Treatment may include antibiotics (for bacterial infections), decongestants, and pain relievers.
Common Cold
The common cold is another frequent culprit mistaken for allergies. While allergies can cause a runny nose and sneezing, the common cold often presents with additional symptoms such as a sore throat, cough, body aches, and fever. The common cold is caused by viruses, and unlike allergies, doesn't typically involve a prolonged, seasonal pattern of symptoms. Treatment is primarily supportive, focusing on rest and symptom relief.
Environmental Irritants
Exposure to environmental irritants like dust mites (although not technically an allergen for everyone), pet dander, mold, smoke, and strong perfumes can cause symptoms very similar to allergies. Unlike true allergies, the body's immune system isn't directly involved. These irritants directly trigger inflammation in the nasal passages and airways, leading to symptoms such as itching, sneezing, and watery eyes. Management focuses on avoiding exposure to the irritants.
Certain Medications
Some medications can produce side effects that mimic allergic symptoms. For example, certain blood pressure medications, ACE inhibitors, can cause a dry cough. Aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) can trigger nasal congestion and other symptoms in some individuals. If you suspect a medication is causing allergy-like symptoms, consult your doctor to discuss alternative options.
| Condition | Key Symptoms | Cause | Treatment |
|---|---|---|---|
| Non-Allergic Rhinitis | Runny nose, stuffy nose, sneezing, itchy eyes | Irritants, hormonal changes, medications | Nasal sprays, antihistamines |
| Sinusitis | Facial pain/pressure, congestion, cough, fever | Viral, bacterial, or fungal infection | Antibiotics (if bacterial), decongestants, pain relievers |
| Common Cold | Runny nose, sneezing, sore throat, cough, body aches, fever | Viruses | Rest, symptom relief |
| Environmental Irritants | Itching, sneezing, watery eyes | Dust, pet dander, mold, smoke, perfumes | Avoidance |
| Medication Side Effects | Vary depending on medication | Specific medications | Change medication or manage symptoms |
What can allergies be mistaken for?
What Can Allergies Be Mistaken For?
Allergies can mimic a wide range of conditions, making diagnosis challenging. Symptoms often overlap, leading to misdiagnosis or delayed treatment. The severity and specific symptoms can vary greatly depending on the allergen, the individual's sensitivity, and the affected system (respiratory, skin, digestive, etc.). Accurate diagnosis often requires a careful history, physical examination, and potentially allergy testing.
1. Common Illnesses
Allergic reactions can easily be confused with common illnesses like the common cold, the flu, or even a sinus infection. The symptoms, such as sneezing, coughing, runny nose, and congestion, are very similar. However, allergies typically lack fever (although a low-grade fever is possible in some cases) and body aches, which are hallmarks of viral infections like the flu. Furthermore, allergic symptoms are often triggered by specific exposures and tend to be chronic or recurring when exposed to the allergen.
- Runny nose and sneezing: Common in both allergies and colds.
- Congestion: Can occur in allergies, colds, and sinus infections.
- Cough: Present in both allergies and respiratory infections.
2. Chronic Conditions
Several chronic conditions can share symptoms with allergies, making it difficult to distinguish between them. For example, asthma, a chronic respiratory condition, frequently coexists with allergies. Similarly, eczema, a chronic skin condition, is often linked to allergies. Chronic fatigue, commonly associated with allergies due to poor sleep from nighttime symptoms, can be mistaken for other systemic illnesses. A comprehensive evaluation is needed to differentiate these conditions.
- Asthma: Often triggered or worsened by allergens.
- Eczema: Frequently linked to allergic reactions.
- Chronic fatigue: May result from prolonged allergic reactions.
3. Gastrointestinal Issues
Food allergies can manifest as various gastrointestinal problems. Symptoms like nausea, vomiting, diarrhea, and abdominal cramps can easily be mistaken for food poisoning, irritable bowel syndrome (IBS), or other digestive disorders. The timing of symptoms (immediately after consuming a specific food) is often a key indicator of a food allergy. A detailed dietary history and allergy testing are crucial for proper diagnosis.
- Nausea and vomiting: Can be symptoms of both food allergies and food poisoning.
- Diarrhea: Common in both food allergies and various digestive disorders.
- Abdominal cramps: Can be present in food allergies and IBS.
4. Skin Conditions
Allergic reactions often involve the skin, leading to symptoms that could be mistaken for other dermatological conditions. Hives (urticaria), a common allergic reaction, might be confused with other rashes or skin irritations. Contact dermatitis, caused by skin contact with irritants, can mimic an allergic contact dermatitis reaction. Careful examination of the rash, its distribution, and associated symptoms are essential for differentiation.
- Hives (urticaria): Characteristic of allergic reactions but can be confused with other rashes.
- Eczema: A chronic inflammatory skin condition often linked to allergies.
- Contact dermatitis: Can mimic allergic contact dermatitis.
5. Neurological Symptoms
While less common, severe allergic reactions (anaphylaxis) can cause symptoms that affect the nervous system, such as dizziness, lightheadedness, and even loss of consciousness. These symptoms could be mistakenly attributed to other neurological conditions, making prompt diagnosis and treatment essential. The rapid onset and systemic nature of anaphylaxis help distinguish it from most neurological conditions.
- Dizziness and lightheadedness: Can be symptoms of anaphylaxis, but also other conditions.
- Loss of consciousness: A serious symptom of anaphylaxis.
- Difficulty breathing: Often present in severe allergic reactions.
Why do I feel like I have allergies but I don't?
Feeling like you have allergies when you don't actually have a diagnosed allergy is a common experience. There are several reasons why you might experience allergy-like symptoms without a true allergy. It's crucial to understand these possibilities to determine the underlying cause and find appropriate relief.
Non-Allergic Rhinitis
Non-allergic rhinitis is a condition that causes similar symptoms to allergies, such as a runny nose, sneezing, and congestion, but it's not triggered by an allergen. Instead, it's often caused by irritants or other factors. This can be triggered by things such as hormonal changes, certain medications, or even changes in weather. It's essential to distinguish between this and a true allergy, as the treatments will differ significantly.
- Hormonal fluctuations: These can significantly impact nasal passages.
- Irritants: Strong smells, smoke, and pollution can mimic allergy symptoms.
- Medications: Some drugs can have nasal congestion as a side effect.
Environmental Irritants
Exposure to various environmental factors can trigger symptoms mimicking allergies. These irritants aren't allergens in the traditional sense; your body isn't producing an immune response, but they can still cause significant discomfort. Dust, fumes, strong perfumes, and changes in humidity or temperature can all contribute to this. Identifying and minimizing exposure to these irritants is key to reducing symptoms.
- Dust mites: These microscopic creatures live in bedding and carpets, causing irritation.
- Mold spores: Present in damp areas, these can trigger respiratory symptoms.
- Air pollution: Exposure to pollutants in the air can lead to nasal irritation.
Vasomotor Rhinitis
Vasomotor rhinitis is another form of non-allergic rhinitis. It involves the dilation and constriction of blood vessels in the nasal passages, leading to nasal congestion and other symptoms. This can be triggered by temperature changes, stress, or even spicy food. Understanding the triggers can help in managing symptoms.
- Temperature changes: Moving from a cold environment to a warm one can trigger symptoms.
- Spicy foods: Certain foods can cause nasal congestion in some individuals.
- Stress: Emotional stress can affect blood vessel dilation.
Food Intolerance
While not a true allergy (which involves the immune system), food intolerance can manifest with symptoms that resemble allergies. This is often characterized by digestive distress, such as bloating, gas, or diarrhea. While not directly causing respiratory symptoms like a runny nose or sneezing, these digestive issues can be uncomfortable and lead to a feeling of general unwellness, possibly mistaken for allergies.
- Lactose intolerance: Difficulty digesting lactose in dairy products.
- Gluten intolerance: Sensitivity to gluten found in wheat, barley, and rye.
- Fructose malabsorption: Difficulty digesting fructose, a type of sugar.
Underlying Medical Conditions
Certain underlying medical conditions can mimic the symptoms of allergies. For example, chronic sinusitis or a deviated septum can cause nasal congestion and other symptoms resembling allergies. These conditions require specific medical diagnoses and treatments distinct from allergy management. It is important to consult a healthcare professional for a proper diagnosis.
- Chronic sinusitis: Inflammation of the sinuses.
- Deviated septum: Misalignment of the nasal septum.
- Other respiratory infections: These infections can cause similar symptoms.
What else feels like allergies?
Many conditions can mimic the symptoms of allergies, making diagnosis challenging. The overlapping symptoms can lead to misdiagnosis and inappropriate treatment. It's crucial to consult a healthcare professional for accurate assessment and proper management. The following are some conditions that share similar symptoms with allergies:
Viral Infections
Viral infections, such as the common cold or influenza, frequently present with symptoms easily confused with allergies. These include a runny nose, sneezing, cough, and congestion. However, unlike allergies, viral infections often involve fever, body aches, and general malaise. Differentiating between the two can be tricky, particularly in the early stages.
- Runny nose: Often clear and watery in both allergies and viral infections.
- Congestion: Can be present in both, but often more severe in viral infections.
- Cough: More prevalent and persistent in viral infections.
Sinusitis
Sinusitis, or inflammation of the sinuses, produces symptoms similar to allergies, including facial pain and pressure, nasal congestion, and headache. The key difference often lies in the duration and severity. Sinusitis usually lasts longer than allergic reactions and involves more intense facial pain. The nasal discharge might be thicker and colored (yellow or green) in sinusitis, whereas allergic rhinitis typically produces clear mucus.
- Facial pain: A prominent symptom of sinusitis, often absent in allergies.
- Thick, discolored nasal discharge: Suggestive of sinusitis rather than allergies.
- Headache: Can be severe and persistent in sinusitis.
Environmental Irritants
Exposure to environmental irritants, such as dust, smoke, or chemical fumes, can trigger symptoms resembling allergies. These include coughing, sneezing, and eye irritation. However, these symptoms typically resolve upon removal from the irritant, unlike true allergic reactions which persist even after the allergen is no longer present. Furthermore, environmental irritants do not usually involve the same systemic symptoms, like skin rashes or gastrointestinal problems.
- Immediate symptom resolution: A key indicator of irritant-induced symptoms.
- Absence of systemic symptoms: Unlike allergies that may involve skin, gut, or other systems.
- Specific trigger identification: Possible in irritant-induced reactions.
Hormonal Changes
Fluctuations in hormone levels, particularly in women, can cause nasal congestion, sneezing, and other allergy-like symptoms. These symptoms are often linked to menstrual cycles or pregnancy. The symptoms are typically milder than true allergic reactions, and there's no identifiable allergen. Hormonal changes do not usually trigger the same degree of skin irritation or other systemic symptoms seen in allergies.
- Timing related to menstrual cycle or pregnancy: A key indicator of hormonal influence.
- Milder symptoms: Compared to the severity often seen in allergies.
- Absence of a specific allergen: A distinguishing feature from allergic reactions.
Gastroesophageal Reflux Disease (GERD)
GERD, characterized by stomach acid refluxing into the esophagus, can cause postnasal drip, cough, and throat irritation. These symptoms can easily be mistaken for allergies, especially if accompanied by nasal congestion. However, GERD symptoms are often worse after eating, especially lying down, and may include heartburn or indigestion. The cough is frequently dry and irritating.
- Heartburn or indigestion: Suggestive of GERD.
- Cough worse after eating: A hallmark of GERD-related symptoms.
- Postnasal drip: Often a prominent feature of GERD.
What diseases mimic allergies?
What Diseases Mimic Allergies?
Several diseases can present with symptoms remarkably similar to allergic reactions, making diagnosis challenging. These conditions often involve inflammation and immune system dysfunction, leading to overlapping symptoms like sneezing, coughing, itchy eyes, rash, and shortness of breath. The key difference lies in the underlying cause: allergies are triggered by an immune response to a harmless substance (allergen), whereas these mimicking diseases stem from internal processes or infections.
1. Vasculitis
Vasculitis encompasses various inflammatory conditions affecting blood vessels. Depending on the affected vessels and severity, symptoms can mimic allergies, including skin rashes (purpura), nasal congestion, and even respiratory problems. Differentiating vasculitis from allergies requires careful examination and often specialized tests, such as biopsies.
- Skin manifestations: Purpura, ulcers, livedo reticularis.
- Respiratory involvement: Cough, shortness of breath, lung inflammation.
- Systemic effects: Fever, fatigue, joint pain, kidney problems (depending on the type of vasculitis).
2. Autoimmune Diseases
Many autoimmune diseases can produce allergy-like symptoms. Conditions like lupus, rheumatoid arthritis, and even certain thyroid disorders can manifest with skin rashes, itching, nasal congestion, or breathing difficulties. Autoantibodies, instead of allergens, drive the inflammation and symptoms in these cases. Diagnosis hinges on identifying the specific autoimmune markers through blood tests and other diagnostic tools.
- Lupus: Butterfly rash, joint pain, fatigue.
- Rheumatoid arthritis: Joint swelling, pain, stiffness, fatigue.
- Thyroid disorders: Fatigue, weight changes, changes in heart rate.
3. Chronic Sinusitis
Persistent inflammation and infection in the sinuses can result in symptoms that mimic seasonal allergies, including nasal congestion, runny nose, sneezing, and postnasal drip. However, chronic sinusitis is often accompanied by facial pain or pressure, a hallmark not typically seen in allergies. Diagnosis frequently relies on imaging studies, such as CT scans, and cultures to identify any bacteria or fungi.
- Facial pain and pressure: Localized pain in the forehead, cheeks, or around the eyes.
- Thick, discolored nasal discharge: Yellow or green mucus indicating infection.
- Reduced sense of smell (anosmia): Due to sinus blockage.
4. Mast Cell Activation Syndrome (MCAS)
MCAS is a condition where mast cells, key players in allergic reactions, release excessive amounts of inflammatory mediators. This leads to a wide range of symptoms mirroring allergies, but often more severe and persistent. Unlike typical allergies, MCAS symptoms aren't triggered by specific allergens but can be precipitated by various factors, including stress, infections, or medications. Diagnosis involves identifying elevated levels of mast cell mediators in the blood or urine.
- Widespread symptoms: Affecting multiple organ systems, such as skin, gut, and respiratory tract.
- Intolerance to various substances: Not necessarily linked to a specific allergen.
- Symptoms may fluctuate in severity: Periods of remission and exacerbation.
5. Certain Infections
Various viral and bacterial infections, particularly respiratory ones, can mimic allergic reactions. Common colds, influenza, and even some bacterial pneumonias can present with symptoms like coughing, sneezing, runny nose, and itchy eyes. The key here is the presence of other infectious signs, such as fever, body aches, or a general feeling of illness, distinguishing them from allergies. Diagnosis relies on identifying the specific pathogen through testing.
- Fever and chills: Indicative of an infection.
- Body aches and fatigue: Common in many infectious illnesses.
- Presence of other infectious signs: Like a sore throat or cough with sputum.
What are some common conditions that mimic allergies?
Many conditions can present symptoms strikingly similar to allergies, making diagnosis tricky. One common culprit is a viral infection, such as the common cold or the flu. These infections often cause nasal congestion, runny nose, sneezing, and even itchy eyes – all classic allergy symptoms. However, unlike allergies, viral infections usually involve other symptoms like fever, body aches, and cough. Non-allergic rhinitis is another frequent imposter. This condition involves inflammation of the nasal lining, causing similar symptoms to allergies but without the involvement of an allergen-specific immune response. Sinusitis, or inflammation of the sinuses, can also produce similar symptoms, particularly nasal congestion, facial pain, and pressure. Certain medications, including some blood pressure medications and aspirin, can trigger similar symptoms as allergies in some individuals. Finally, environmental irritants, such as smoke, dust, and strong chemicals, can irritate the mucous membranes and trigger symptoms resembling an allergic reaction without a true allergic response. Differentiating between these conditions requires careful consideration of the symptom presentation and a thorough medical history.
How can I tell if my symptoms are truly allergies or something else?
Distinguishing between allergies and other conditions requires a careful evaluation of your symptoms and their pattern. Allergies usually exhibit a predictable pattern, triggered by exposure to a specific allergen, such as pollen, pet dander, or dust mites. Symptoms typically start shortly after exposure and improve once exposure ceases. In contrast, symptoms of other conditions, like viral infections, may develop gradually and persist for several days or weeks, regardless of environmental factors. The presence of additional symptoms can also be indicative of something other than allergies. Fever, body aches, and cough strongly suggest a viral infection, while facial pain and pressure point towards sinusitis. Keeping a detailed symptom diary, noting the timing, intensity, and associated symptoms, can be incredibly helpful for both you and your doctor in reaching an accurate diagnosis. A consultation with a healthcare professional is crucial for proper diagnosis and treatment planning, as they can assess your symptoms, medical history, and conduct necessary tests, such as allergy testing, to determine the underlying cause.
What tests might my doctor use to rule out allergies?
Your doctor may employ several tests to determine if your symptoms are caused by allergies or another condition. Allergy skin testing is a common method, involving the application of small amounts of potential allergens to your skin. A positive reaction, indicated by a wheal and flare response, suggests an allergy to that specific allergen. Blood tests can also measure the levels of specific antibodies (IgE) associated with allergic reactions. However, these tests can be less specific than skin tests and may not always be conclusive. Nasal endoscopy might be used to visualize the nasal passages and rule out conditions like sinusitis or structural abnormalities that could be contributing to your symptoms. Chest X-rays might be considered if a cough or lung involvement is suspected, helping to rule out other respiratory illnesses. In some cases, a trial of allergy medications might be employed to see if symptoms improve, helping to assess the likelihood of allergies. The choice of tests will depend on your individual symptoms, medical history, and the doctor's clinical judgment. The results of these tests will help to confirm or rule out allergies, leading to an accurate diagnosis and appropriate treatment plan.
When should I seek medical attention for symptoms that seem like allergies?
While many allergy-like symptoms can be managed at home, it's crucial to seek medical attention under certain circumstances. If your symptoms are severe, such as difficulty breathing, swelling of the face or throat (angioedema), or persistent dizziness, you should seek immediate medical attention as these could indicate a serious allergic reaction. If your symptoms are unresponsive to over-the-counter medications or worsen despite treatment, a doctor's consultation is warranted. Similarly, if you experience new or unusual symptoms in conjunction with allergy-like symptoms, a medical evaluation is essential to rule out more serious conditions. Persistent symptoms, lasting for several weeks or months without improvement, necessitate a professional assessment to identify the underlying cause and receive appropriate treatment. If you suspect you might have an allergy but are unsure, or if you are experiencing symptoms that significantly impact your quality of life, it's advisable to schedule an appointment with your doctor or an allergist for a thorough evaluation and diagnosis.


Deja una respuesta