What is the root cause of allergies

In the realm of human health, allergies have emerged as a prevalent and vexing ailment, affecting countless individuals worldwide. While the symptoms of allergies—from a stuffy nose to itchy eyes—are all too familiar, the underlying cause remains a complex enigma. This article delves into the depths of this enigmatic condition, exploring the root causes of allergies and shedding light on their intricate mechanisms.
What is the Root Cause of Allergies: A Complex Interaction
The root cause of allergies is a complex interplay of genetic predisposition and environmental factors. It's not a single cause, but rather a combination of events that lead to an overactive immune system. Essentially, the body mistakenly identifies a harmless substance (allergen) as a threat and mounts an immune response that leads to allergic symptoms. This response involves several key players, from the genetic code to specific immune cells and the environmental triggers themselves.
Genetic Predisposition: The Inherited Component
A significant factor in the development of allergies is a family history of allergies, asthma, or eczema. This suggests a genetic component. While specific genes haven't been definitively identified as "allergy genes," research points to variations in genes involved in immune system regulation. These variations can make individuals more susceptible to developing allergic reactions. For instance, some genes influence the production of IgE antibodies, which play a crucial role in allergic responses. It's important to note that having a family history doesn't guarantee an allergy, but it significantly increases the risk.
Immune System Dysregulation: The Overreaction
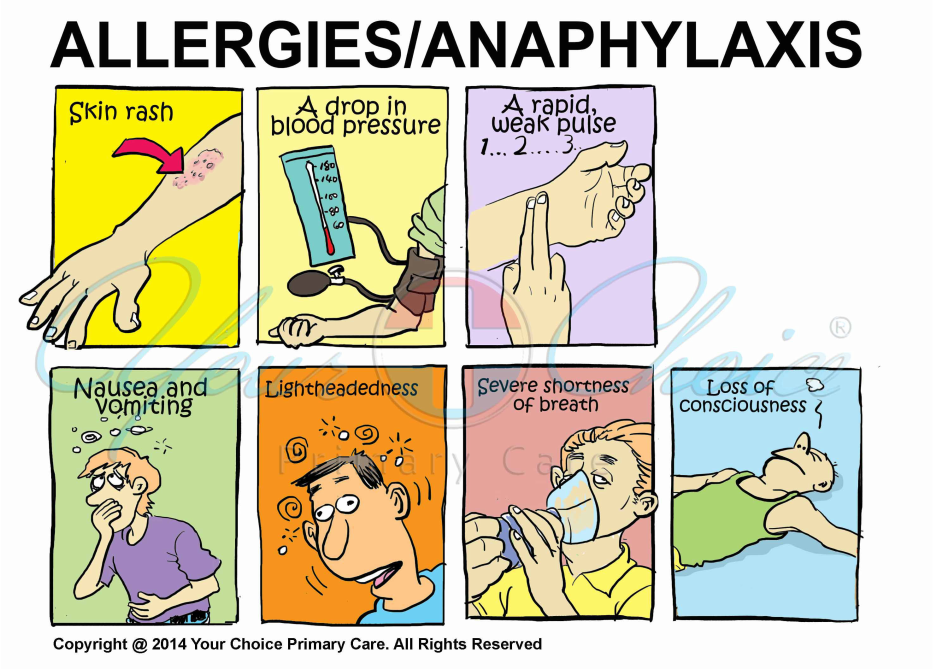
At the heart of allergies lies an immune system malfunction. When exposed to an allergen (like pollen, pet dander, or peanuts), the immune system of an allergic individual mistakenly identifies it as a threat. This triggers the production of immunoglobulin E (IgE) antibodies. These IgE antibodies bind to mast cells and basophils, which are immune cells residing in tissues throughout the body. Upon subsequent exposure to the same allergen, the IgE antibodies on these cells trigger the release of histamine and other inflammatory mediators. This release causes the characteristic symptoms of an allergic reaction, such as sneezing, itching, swelling, and difficulty breathing.
Environmental Triggers: The Allergens
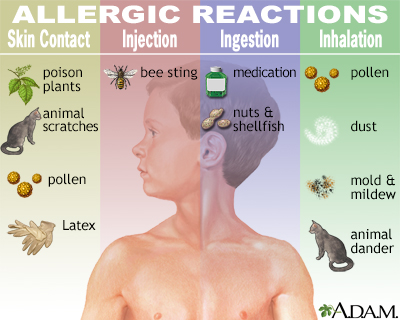
Environmental allergens are the substances that trigger an allergic reaction in susceptible individuals. These can be diverse, ranging from pollens and molds in the air to foods like peanuts, milk, and eggs, as well as pet dander, dust mites, and insect stings. The prevalence and concentration of these allergens can influence the severity and frequency of allergic reactions. Geographic location, climate, and lifestyle factors contribute to the exposure levels of various allergens.
The Hygiene Hypothesis: A Proposed Explanation
The hygiene hypothesis proposes that a lack of early exposure to infectious agents and parasites can disrupt the development of a balanced immune system, leading to an increased risk of allergies. This theory suggests that early exposure to diverse microbes helps train the immune system to differentiate between harmless substances and genuine threats. In environments with high sanitation and reduced microbial exposure, the immune system might be more prone to misidentifying harmless substances as dangerous, thus triggering allergic reactions.
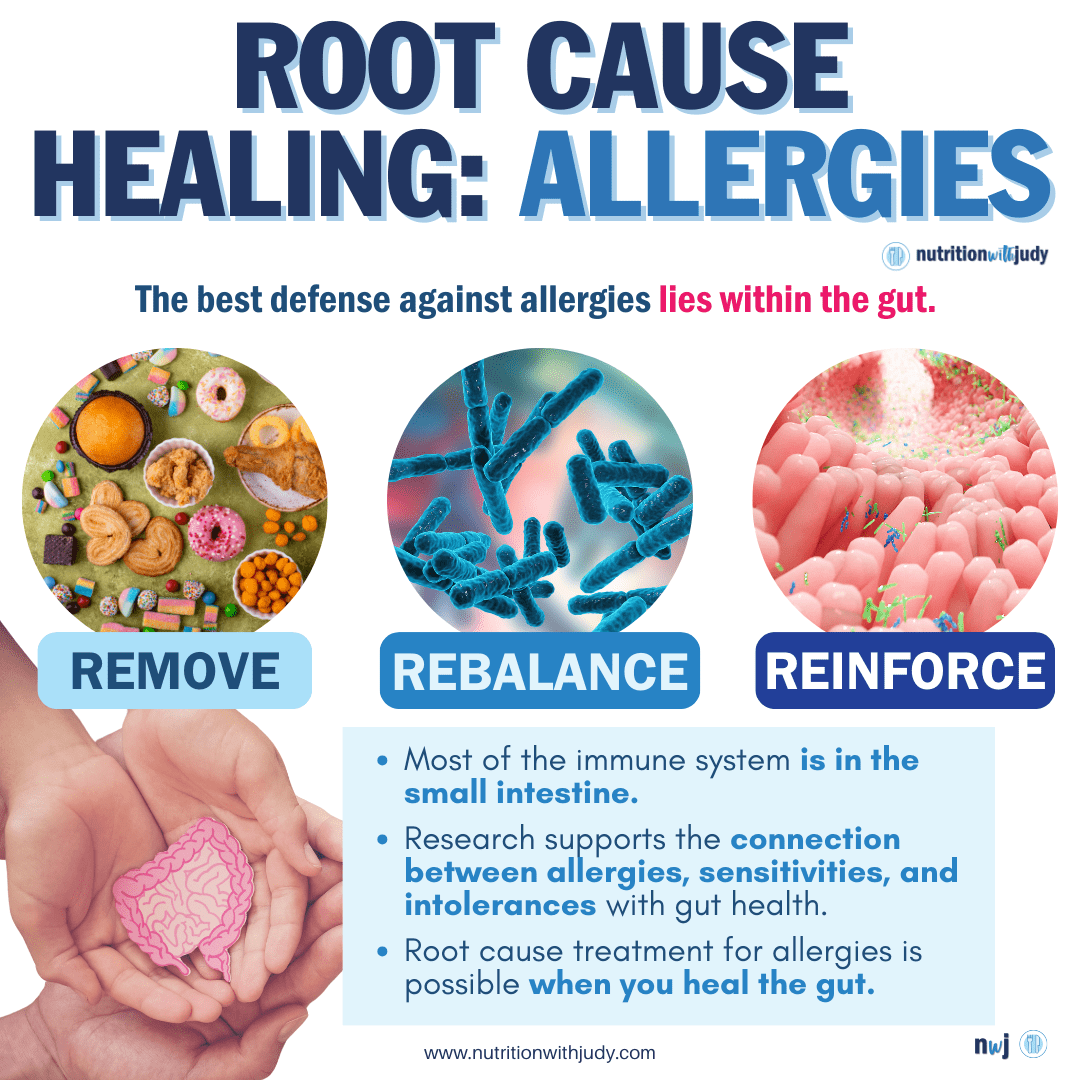
The Role of the Gut Microbiome: Emerging Research
Research is increasingly focusing on the role of the gut microbiome in allergy development. The gut microbiome encompasses the trillions of bacteria and other microbes residing in the digestive tract. The composition and function of the gut microbiome can significantly impact immune system development and regulation. Studies suggest that imbalances in the gut microbiome, known as dysbiosis, might contribute to the development of allergies. Further research is necessary to fully understand the complex interactions between the gut microbiome and allergic responses.
| Factor | Role in Allergy Development |
|---|---|
| Genetics | Increased susceptibility through inherited immune system variations. |
| Immune System Dysregulation | IgE antibody production and release of inflammatory mediators. |
| Environmental Allergens | Triggers for the allergic immune response; examples include pollen, foods, and pet dander. |
| Hygiene Hypothesis | Lack of early exposure to microbes may lead to immune system imbalances. |
| Gut Microbiome | Dysbiosis (imbalance) may contribute to allergy development. |
What is the Root Cause of Allergies: A Complex Interaction
The root cause of allergies is a complex interplay of genetic predisposition and environmental factors. It's not a single cause, but rather a combination of events that lead to an overactive immune system. Essentially, the body mistakenly identifies a harmless substance (allergen) as a threat and mounts an immune response that leads to allergic symptoms. This response involves several key players, from the genetic code to specific immune cells and the environmental triggers themselves.
Genetic Predisposition: The Inherited Component
A significant factor in the development of allergies is a family history of allergies, asthma, or eczema. This suggests a genetic component. While specific genes haven't been definitively identified as "allergy genes," research points to variations in genes involved in immune system regulation. These variations can make individuals more susceptible to developing allergic reactions. For instance, some genes influence the production of IgE antibodies, which play a crucial role in allergic responses. It's important to note that having a family history doesn't guarantee an allergy, but it significantly increases the risk.
Immune System Dysregulation: The Overreaction
At the heart of allergies lies an immune system malfunction. When exposed to an allergen (like pollen, pet dander, or peanuts), the immune system of an allergic individual mistakenly identifies it as a threat. This triggers the production of immunoglobulin E (IgE) antibodies. These IgE antibodies bind to mast cells and basophils, which are immune cells residing in tissues throughout the body. Upon subsequent exposure to the same allergen, the IgE antibodies on these cells trigger the release of histamine and other inflammatory mediators. This release causes the characteristic symptoms of an allergic reaction, such as sneezing, itching, swelling, and difficulty breathing.
Environmental Triggers: The Allergens
Environmental allergens are the substances that trigger an allergic reaction in susceptible individuals. These can be diverse, ranging from pollens and molds in the air to foods like peanuts, milk, and eggs, as well as pet dander, dust mites, and insect stings. The prevalence and concentration of these allergens can influence the severity and frequency of allergic reactions. Geographic location, climate, and lifestyle factors contribute to the exposure levels of various allergens.
The Hygiene Hypothesis: A Proposed Explanation
The hygiene hypothesis proposes that a lack of early exposure to infectious agents and parasites can disrupt the development of a balanced immune system, leading to an increased risk of allergies. This theory suggests that early exposure to diverse microbes helps train the immune system to differentiate between harmless substances and genuine threats. In environments with high sanitation and reduced microbial exposure, the immune system might be more prone to misidentifying harmless substances as dangerous, thus triggering allergic reactions.
The Role of the Gut Microbiome: Emerging Research
Research is increasingly focusing on the role of the gut microbiome in allergy development. The gut microbiome encompasses the trillions of bacteria and other microbes residing in the digestive tract. The composition and function of the gut microbiome can significantly impact immune system development and regulation. Studies suggest that imbalances in the gut microbiome, known as dysbiosis, might contribute to the development of allergies. Further research is necessary to fully understand the complex interactions between the gut microbiome and allergic responses.
| Factor | Role in Allergy Development |
|---|---|
| Genetics | Increased susceptibility through inherited immune system variations. |
| Immune System Dysregulation | IgE antibody production and release of inflammatory mediators. |
| Environmental Allergens | Triggers for the allergic immune response; examples include pollen, foods, and pet dander. |
| Hygiene Hypothesis | Lack of early exposure to microbes may lead to immune system imbalances. |
| Gut Microbiome | Dysbiosis (imbalance) may contribute to allergy development. |
How to get to the root cause of allergies?
Getting to the root cause of allergies requires a multi-faceted approach involving detailed medical history, thorough testing, and often, a process of elimination. There's no single, universally applicable test, as allergy triggers vary widely between individuals. The journey focuses on identifying the specific allergen(s) causing the reaction, understanding the underlying mechanisms, and potentially addressing contributing factors.
1. Comprehensive Medical History and Physical Exam
A detailed discussion with your allergist is the crucial first step. They will inquire about your symptoms, their onset, frequency, severity, and any associated factors. Be prepared to discuss your family history of allergies, any past illnesses, medications you take, your lifestyle (diet, exercise, exposure to potential allergens), and your environment (pets, home environment, work environment). A thorough physical examination is also important to rule out other conditions that might mimic allergic symptoms.
- Discuss the timing and circumstances of your allergy symptoms.
- Provide a detailed list of potential allergy triggers you've encountered.
- Describe the nature and severity of your symptoms.
2. Skin Prick Testing
Skin prick testing is a common method used to identify allergies. Small amounts of potential allergens are pricked onto your skin. A raised wheal (a hive) at the prick site indicates a positive reaction and suggests an allergy. This test is relatively quick, inexpensive, and provides results immediately, but it doesn't detect all types of allergies, particularly those involving food. False positives and negatives are possible.
- This test is usually quick and painless.
- It can identify multiple allergens simultaneously.
- Results are available almost immediately.
3. Blood Tests
Blood tests, such as radioallergosorbent tests (RAST) or enzyme-linked immunosorbent assays (ELISA), measure the levels of IgE antibodies in your blood that are specific to certain allergens. Blood tests are useful for detecting allergies to foods and inhalants that are difficult to test with skin prick tests and for people who cannot undergo skin prick testing due to medications or skin conditions. However, they're generally more expensive than skin prick testing.
- Blood tests can detect a wider range of allergens compared to skin prick testing.
- They are useful for individuals with skin conditions or those on medications affecting skin prick tests.
- Results may take longer than skin prick tests.
4. Food Challenges and Elimination Diets
For suspected food allergies, a controlled food challenge under medical supervision might be necessary. This involves gradually introducing the suspected food allergen to your diet while closely monitoring for any allergic reactions. Elimination diets, where suspected allergens are removed from the diet for a period, can also be used to identify potential food triggers, but they require careful planning and monitoring to ensure nutritional adequacy.
- Food challenges must be conducted under medical supervision.
- Elimination diets require careful planning to avoid nutritional deficiencies.
- These methods are essential in confirming or ruling out specific food allergies.
5. Investigating Underlying Factors and Comorbidities
Allergies can sometimes be linked to other underlying health issues, such as eczema (atopic dermatitis), asthma, or autoimmune disorders. Your allergist may investigate these possibilities to obtain a complete picture. Addressing underlying health problems can sometimes reduce the severity or frequency of allergy symptoms. Environmental factors, stress levels, and even gut microbiome imbalances can also play a role and warrant investigation.
- Assess for related conditions such as eczema or asthma.
- Consider the influence of environmental factors (pollutants, mold).
- Evaluate the potential role of gut health and stress.
What is the root cause of allergic reactions?
The root cause of allergic reactions is an overreaction by the immune system to a normally harmless substance, known as an allergen. This overreaction occurs because the immune system mistakenly identifies the allergen as a threat, triggering a cascade of events that leads to the characteristic symptoms of an allergic reaction. Instead of ignoring the allergen, the body mounts a defense against it, releasing various chemicals that cause inflammation and other reactions. This misidentification is a key feature of allergies, distinguishing them from other forms of immune responses.
Immune System Misidentification
At the heart of allergic reactions lies the immune system's failure to recognize harmless substances as such. This misidentification leads to the production of IgE antibodies, which bind to mast cells and basophils. When the allergen is encountered again, it binds to these IgE antibodies, triggering their degranulation and the release of inflammatory mediators like histamine. This process sets off a chain reaction, causing the various symptoms of allergic reactions.
- IgE antibody production is a hallmark of allergic responses.
- Mast cell and basophil degranulation releases histamine and other inflammatory mediators.
- Inflammatory mediators trigger the characteristic symptoms of allergic reactions (e.g., swelling, itching, rash).
The Role of IgE Antibodies
IgE antibodies play a central role in allergic reactions. They are a type of antibody produced by the immune system in response to allergens. Unlike other antibodies, IgE antibodies bind to mast cells and basophils, immune cells that are located in tissues throughout the body. When the allergen is encountered again, it binds to the IgE antibodies, causing the mast cells and basophils to release histamine and other chemicals that contribute to the symptoms of an allergic reaction. The levels of IgE antibodies in the blood are often used to diagnose allergies.
- IgE antibodies are specifically involved in allergic responses.
- Binding of allergens to IgE triggers mast cell and basophil activation.
- Histamine release causes the hallmark symptoms of an allergy, such as hives and itching.
Genetic Predisposition and Family History
A significant factor contributing to the development of allergies is genetic predisposition. Individuals with a family history of allergies are more likely to develop them themselves. While the exact genes involved are still being researched, it's evident that inherited traits influence immune system development and reactivity. This genetic susceptibility doesn't guarantee the development of allergies, but it significantly increases the risk. Environmental factors also play a crucial role in triggering allergic responses in genetically susceptible individuals.
- Family history of allergies is a strong predictor of allergy development.
- Genetic variations influence immune system response to allergens.
- Gene-environment interactions determine the likelihood of developing allergies.
Environmental Factors and Exposure
Exposure to allergens is a critical factor in triggering allergic reactions. The environment plays a crucial role, exposing individuals to a wide range of potential allergens like pollen, dust mites, pet dander, and food proteins. The frequency and intensity of exposure significantly impact the severity of allergic responses. Regular exposure can sensitize the immune system, making individuals more likely to react strongly upon subsequent encounters with the same allergen. Preventing or reducing exposure is a key strategy in managing allergies.
- Exposure to allergens is essential for triggering allergic reactions.
- Frequency and intensity of exposure influence allergic response severity.
- Environmental control measures can help reduce allergic symptoms.
The Role of Inflammatory Mediators
Once an allergen binds to IgE antibodies on mast cells and basophils, these cells release a variety of inflammatory mediators. These mediators, including histamine, leukotrienes, and prostaglandins, are responsible for the diverse symptoms of allergic reactions. Histamine, for instance, causes vasodilation, increased vascular permeability, and bronchoconstriction, leading to symptoms like swelling, itching, and difficulty breathing. Understanding the role of these mediators is crucial for developing effective treatments that target specific pathways involved in the inflammatory response.
- Histamine causes vasodilation, increased permeability, and bronchoconstriction.
- Leukotrienes contribute to prolonged bronchoconstriction and inflammation.
- Prostaglandins contribute to inflammation and pain.
What is the root cause of skin allergies?

Skin allergies, also known as allergic dermatitis or eczema, arise from a malfunction in the body's immune system. The root cause lies in an overreaction by the immune system to otherwise harmless substances, called allergens. When the skin comes into contact with an allergen, the immune system mistakenly identifies it as a threat. This triggers a cascade of events, involving the release of inflammatory chemicals like histamine, leading to the characteristic symptoms of itching, redness, swelling, and rash. The precise mechanism varies depending on the type of allergy (e.g., contact dermatitis, atopic dermatitis), but the underlying principle remains the same: an inappropriate immune response to a non-threatening substance.
Genetic Predisposition
A family history of allergies, asthma, or eczema significantly increases the risk of developing skin allergies. This suggests a strong genetic component plays a role. While specific genes haven't been definitively identified for all skin allergies, inherited variations in immune system function likely influence how susceptible an individual is to developing these conditions. This predisposition doesn't guarantee the development of an allergy, but it raises the likelihood.
- Family history of atopic conditions significantly increases risk.
- Genetic variations affect immune system development and responsiveness.
- Predisposition doesn't guarantee allergy development, but increases probability.
Environmental Factors
Exposure to various environmental triggers can significantly influence the development and severity of skin allergies. These environmental factors are often interacting with an individual's genetic predisposition. Common triggers include irritants like harsh soaps and detergents, allergens such as pollen, pet dander, and dust mites, and even certain fabrics or metals. Pollution and climate changes may also play a role, especially in exacerbating existing allergies.
- Irritants like harsh soaps and detergents can trigger allergic reactions.
- Allergens like pollen, pet dander, and dust mites are common culprits.
- Environmental pollution and climate change may worsen allergies.
Immature Skin Barrier
The skin acts as a barrier against external substances. In individuals with skin allergies, this barrier may be compromised, making it more permeable to allergens and irritants. This weakened barrier function can be due to genetic factors or be further compromised by environmental factors like dry air, frequent washing with harsh soaps, and other skin injuries. A compromised barrier allows more allergens to penetrate, stimulating an exaggerated immune response.
- Weakened skin barrier allows easier penetration of allergens and irritants.
- Genetic factors and environmental exposures can damage the skin barrier.
- Increased permeability leads to greater immune system stimulation.
Immune System Dysregulation
Skin allergies involve a dysregulation of the immune system. The immune system's T helper cells, particularly Th2 cells, play a central role. In allergic reactions, there's an overproduction of Th2 cytokines, which promote inflammation. This imbalance contributes to the characteristic symptoms of skin allergies. Additionally, dysregulation of other immune cells, such as mast cells, also plays a part.
- Th2 cell overactivity leads to increased inflammation.
- Cytokine imbalance drives the allergic response.
- Mast cell dysregulation contributes to the inflammatory cascade.
Infections
While not a direct cause, certain infections can trigger or exacerbate skin allergies. Viral or bacterial infections can disrupt the skin barrier function, making it more susceptible to allergens and irritants. In some cases, infections can directly activate immune cells, leading to a more intense inflammatory response. The weakened skin barrier from infection can make the skin more sensitive, amplifying allergic reactions.
- Viral or bacterial infections can compromise the skin barrier.
- Infections can directly activate immune cells increasing inflammation.
- Weakened skin barrier from infection increases susceptibility to allergens.
Does having allergies mean your immune system is weak?
No, having allergies does not necessarily mean you have a weak immune system. In fact, it's quite the opposite. Allergies are a result of an overactive, rather than a weak, immune system. A healthy immune system is capable of identifying and neutralizing threats, such as viruses and bacteria. In people with allergies, the immune system mistakenly identifies harmless substances, like pollen or pet dander, as dangerous invaders. This triggers an immune response that produces excessive amounts of antibodies called immunoglobulin E (IgE), leading to allergy symptoms. While the immune system is responding aggressively, it's misdirected, not weak.
What is the Role of IgE Antibodies in Allergies?
IgE antibodies play a central role in allergic reactions. When a person with an allergy is exposed to an allergen (the substance that triggers the allergy), their immune system produces IgE antibodies specifically targeted to that allergen. These IgE antibodies bind to mast cells and basophils, which are types of white blood cells. Upon subsequent exposure to the same allergen, the IgE antibodies on these cells trigger their release of histamine and other inflammatory mediators. This release causes the characteristic symptoms of an allergic reaction, such as sneezing, itching, and inflammation.
- IgE antibodies are specifically produced by plasma cells in response to allergens.
- They bind to mast cells and basophils, sensitizing these cells to the allergen.
- Upon subsequent exposure to the allergen, the IgE antibodies trigger the release of histamine and other inflammatory mediators, leading to allergy symptoms.
How Does the Immune System Normally Respond to Threats?
A healthy immune system operates through a complex interplay of cells and molecules. When it encounters a genuine threat, like a virus or bacteria, it initiates a response involving various components. This typically includes the innate immune system’s immediate, non-specific defense, followed by the adaptive immune system's more targeted and long-lasting response. The adaptive immune system creates memory cells, providing quicker and more effective responses to future encounters with the same threat. Allergies, however, bypass this efficient, targeted process by triggering an inappropriate and overzealous response to harmless substances.
- The innate immune system provides an immediate, non-specific response to pathogens.
- The adaptive immune system mounts a targeted response, producing specific antibodies and memory cells for long-term protection.
- This coordinated response efficiently neutralizes the threat, preventing illness or infection.
What are the Differences Between Allergies and a Compromised Immune System?
A person with a compromised immune system is more susceptible to infections because their body struggles to effectively fight off pathogens. This can be due to various factors, including illness, malnutrition, or certain medications. Allergies, on the other hand, indicate an overactive immune system, not an ineffective one. The immune system is actively responding, but its response is misdirected towards harmless substances. A compromised immune system has difficulty responding adequately even to genuine threats; an allergic individual's immune system is overly responsive to harmless triggers.
- A compromised immune system is characterized by increased susceptibility to infections.
- Allergies represent an overreaction of the immune system to harmless substances.
- The consequences of a compromised immune system are entirely different from those of allergies.
Can Allergies Indicate Underlying Immune Dysregulation?
While allergies themselves don't indicate a weak immune system, they can sometimes be a sign of broader immune dysregulation. This means the immune system isn't functioning perfectly, even if its overall strength is not reduced. Certain immune disorders can increase the likelihood of allergies. Understanding the specific interplay of genetic predispositions and environmental factors is still an area of ongoing research, and the exact cause-and-effect relationships are not fully elucidated. However, it's crucial to distinguish between an overactive immune response (allergies) and an insufficient immune response (immunodeficiency).
- Allergies can be associated with other immune disorders, reflecting a broader pattern of immune system dysregulation.
- Genetic factors and environmental influences play a role in the development of allergies.
- Further research is needed to fully understand the complex interplay between allergies and immune dysregulation.
Are There any Treatments for Allergies?
Various treatments are available to manage allergy symptoms and reduce their impact on daily life. These treatments aim to either reduce the immune response to allergens or alleviate the symptoms caused by the inflammatory response. Antihistamines are commonly used to block the effects of histamine, a key mediator of allergic reactions. Immunotherapy, also known as allergy shots, involves gradually exposing the body to increasing amounts of the allergen over time to desensitize the immune system. Other treatments include nasal corticosteroids and medications to control asthma symptoms, which are often associated with allergies.
- Antihistamines block the action of histamine, reducing allergy symptoms.
- Immunotherapy aims to desensitize the immune system to the allergen.
- Other treatments target specific allergy symptoms, such as nasal congestion or asthma.
What is an allergy, and what causes them?
An allergy is a hypersensitive reaction by your immune system to a normally harmless substance. This substance, called an allergen, can be anything from pollen and pet dander to food and medications. When you're exposed to an allergen, your body mistakenly identifies it as a threat. This triggers your immune system to release histamine and other chemicals, leading to a range of symptoms. The root cause lies in the misidentification of the allergen by your immune system. While genetics play a significant role, influencing an individual's predisposition to develop allergies, the exact mechanism isn't fully understood. Research suggests that environmental factors, such as exposure to certain substances during critical periods of development, might also contribute. In essence, the root cause is a complex interplay between genetic predisposition and environmental triggers that result in your immune system overreacting to a harmless substance. This overreaction manifests as an allergic response. Understanding this interplay is crucial for both preventing and treating allergic reactions effectively.
Why do some people develop allergies and others don't?
The development of allergies is a complex process influenced by several interconnected factors. One of the most significant contributors is genetics. A family history of allergies significantly increases your risk. However, genetics doesn't dictate whether or not you'll develop an allergy; it merely increases your susceptibility. This means that even with a family history, you might not develop allergies, and conversely, someone without a family history could still develop them. Environmental factors also play a crucial role. Exposure to certain allergens during early childhood, especially in the first few years of life, can influence allergy development. This concept is known as the "hygiene hypothesis," which posits that limited exposure to pathogens and allergens during childhood might lead to an overactive immune system. Another key factor is the individual's immune system itself. Variations in the immune response and the way the body interacts with allergens are unique to each individual, influencing their likelihood of developing an allergic reaction. In summary, the reason why some people develop allergies while others don't is a combination of inherited genetic traits, environmental exposures, and individual variations in immune system function.
Can allergies be cured?
Unfortunately, there's currently no known cure for allergies. While there is no way to completely eliminate the predisposition to an allergic reaction, various methods can effectively manage and control the symptoms. Immunotherapy, also known as allergy shots, is one approach that aims to desensitize the immune system to specific allergens over time. This treatment involves gradually increasing exposure to the allergen, training the immune system to tolerate it. Another approach involves medications such as antihistamines, corticosteroids, and decongestants to relieve symptoms. These medications manage the symptoms but don't eliminate the underlying allergy. Lifestyle changes, such as avoiding allergens, can also play a significant role in managing allergies. This might include using air purifiers, avoiding specific foods, and taking other precautionary measures to minimize exposure to triggers. In conclusion, while a complete cure remains elusive, a combination of immunotherapy, medications, and lifestyle modifications provides effective management strategies for allergy sufferers, significantly improving quality of life.
What role does the environment play in the development of allergies?
The environment plays a significant role in the development of allergies. Several environmental factors can either trigger or exacerbate allergic reactions. Air pollution, for example, can irritate the respiratory system, making individuals more susceptible to allergic symptoms. Exposure to certain allergens at critical periods of development, especially during infancy and early childhood, can influence the likelihood of developing allergies later in life. This is supported by the "hygiene hypothesis," suggesting that limited exposure to pathogens and allergens in early childhood might lead to an overly reactive immune system. Furthermore, the level of allergen exposure significantly impacts allergy development and severity. Individuals living in areas with high pollen counts or significant pet dander might experience more severe allergic reactions. Changes in the environment, such as climate change, can also influence allergen levels and seasons, potentially leading to increased allergy prevalence and severity. In summary, the environment's impact on allergy development is complex and multifaceted, encompassing both direct triggers and indirect factors that modulate the immune response and susceptibility to allergies. Understanding these environmental influences is crucial for both preventing and managing allergic conditions.
Deja una respuesta