What's the rarest allergy

In the vast tapestry of allergies, some stand out as more peculiar and uncommon than others. From the curious case of dihydrogen monoxide sensitivity to the enigmatic allergy to water, the world of allergies holds a myriad of mysteries. Among this enigmatic assembly, there lies a rare and extraordinary allergy that has intrigued scientists and puzzled sufferers alike - allergy to red meat.
What are Some of the Rarest Allergies?
Pinpointing the single "rarest" allergy is incredibly difficult. Allergy prevalence varies geographically and is constantly being researched. Furthermore, many rare allergies go undiagnosed or unreported due to their unusual nature and the challenges in identifying the allergen. However, we can discuss some allergies considered extremely uncommon and challenging to diagnose.
Allergy to Water (Aquagenic Urticaria)
Aquagenic urticaria is a truly rare condition where the skin reacts to contact with water, regardless of its source (tap water, rain, sweat). The reaction typically manifests as hives and itching within minutes of exposure. The exact cause isn't fully understood, but it's thought to be related to a substance that reacts with water on the skin's surface, perhaps a specific protein or chemical compound. Diagnosis is based on a careful history and the reproducible reaction to water challenges, excluding other potential triggers.
Allergy to Sunlight (Solar Urticaria)
Solar urticaria is an allergy triggered by exposure to ultraviolet (UV) radiation from sunlight. It causes hives, itching, and sometimes swelling at the site of sun exposure. Specific wavelengths of UV light trigger different reactions, and it's not always clear which are the culprits. Some cases are triggered by specific components of sunlight, while others are triggered by a complex interplay of factors within the skin's reaction to UV radiation. Diagnosis often involves phototesting, where the skin is exposed to controlled doses of UV light to determine sensitivity.
Allergy to Cold (Cold Urticaria)
Cold urticaria is characterized by hives, itching, and swelling in response to exposure to cold temperatures, which can affect everything from cold air to cold water to cold foods. The severity can range from mild discomfort to life-threatening anaphylaxis in severe cases. It's believed to be an abnormal immune response to cold temperatures, often involving the release of histamine and other inflammatory substances. Diagnosis is typically based on a history of cold-related symptoms and confirmed with cold stimulation tests.
Allergy to Exercise (Exercise-Induced Anaphylaxis)
Exercise-induced anaphylaxis (EIA) is a rare but potentially life-threatening condition where physical activity triggers a severe allergic reaction, including hives, swelling, difficulty breathing, and a drop in blood pressure. It's often associated with the consumption of certain foods (such as wheat or shellfish) before exercise or certain medications. However, some cases occur with no clear additional triggers. The exact mechanism isn't fully understood, but it involves a complex interaction between physical exertion and the immune system. Diagnosis is made through careful history taking and allergy testing, ideally including an exercise challenge under medical supervision.
Allergy to Pressure (Pressure Urticaria)
Pressure urticaria is a rare type of allergy characterized by the development of hives and swelling in areas subjected to prolonged or firm pressure. The reaction may occur several hours after the pressure is applied, and the affected areas are often intensely itchy. The cause is unknown, but it’s believed to involve a localized immune response triggered by the mechanical stress of pressure on the skin. Diagnosis is generally made based on history and clinical findings, especially if the hives appear specifically in areas that have been under pressure.
| Allergy Type | Key Characteristics | Diagnostic Approach |
|---|---|---|
| Aquagenic Urticaria | Hives and itching after contact with any water. | Careful history, water challenge test. |
| Solar Urticaria | Hives and itching after sun exposure. | Phototesting. |
| Cold Urticaria | Hives and itching after exposure to cold. | Cold stimulation tests. |
| Exercise-Induced Anaphylaxis | Severe allergic reaction triggered by exercise, often with food or medication involvement. | History, allergy testing, exercise challenge test. |
| Pressure Urticaria | Hives and swelling in areas subjected to pressure. | Clinical assessment based on history and physical examination. |
What are Some of the Rarest Allergies?
Pinpointing the single "rarest" allergy is incredibly difficult. Allergy prevalence varies geographically and is constantly being researched. Furthermore, many rare allergies go undiagnosed or unreported due to their unusual nature and the challenges in identifying the allergen. However, we can discuss some allergies considered extremely uncommon and challenging to diagnose.
Allergy to Water (Aquagenic Urticaria)
Aquagenic urticaria is a truly rare condition where the skin reacts to contact with water, regardless of its source (tap water, rain, sweat). The reaction typically manifests as hives and itching within minutes of exposure. The exact cause isn't fully understood, but it's thought to be related to a substance that reacts with water on the skin's surface, perhaps a specific protein or chemical compound. Diagnosis is based on a careful history and the reproducible reaction to water challenges, excluding other potential triggers.
Allergy to Sunlight (Solar Urticaria)
Solar urticaria is an allergy triggered by exposure to ultraviolet (UV) radiation from sunlight. It causes hives, itching, and sometimes swelling at the site of sun exposure. Specific wavelengths of UV light trigger different reactions, and it's not always clear which are the culprits. Some cases are triggered by specific components of sunlight, while others are triggered by a complex interplay of factors within the skin's reaction to UV radiation. Diagnosis often involves phototesting, where the skin is exposed to controlled doses of UV light to determine sensitivity.
Allergy to Cold (Cold Urticaria)
Cold urticaria is characterized by hives, itching, and swelling in response to exposure to cold temperatures, which can affect everything from cold air to cold water to cold foods. The severity can range from mild discomfort to life-threatening anaphylaxis in severe cases. It's believed to be an abnormal immune response to cold temperatures, often involving the release of histamine and other inflammatory substances. Diagnosis is typically based on a history of cold-related symptoms and confirmed with cold stimulation tests.
Allergy to Exercise (Exercise-Induced Anaphylaxis)
Exercise-induced anaphylaxis (EIA) is a rare but potentially life-threatening condition where physical activity triggers a severe allergic reaction, including hives, swelling, difficulty breathing, and a drop in blood pressure. It's often associated with the consumption of certain foods (such as wheat or shellfish) before exercise or certain medications. However, some cases occur with no clear additional triggers. The exact mechanism isn't fully understood, but it involves a complex interaction between physical exertion and the immune system. Diagnosis is made through careful history taking and allergy testing, ideally including an exercise challenge under medical supervision.
Allergy to Pressure (Pressure Urticaria)
Pressure urticaria is a rare type of allergy characterized by the development of hives and swelling in areas subjected to prolonged or firm pressure. The reaction may occur several hours after the pressure is applied, and the affected areas are often intensely itchy. The cause is unknown, but it’s believed to involve a localized immune response triggered by the mechanical stress of pressure on the skin. Diagnosis is generally made based on history and clinical findings, especially if the hives appear specifically in areas that have been under pressure.
| Allergy Type | Key Characteristics | Diagnostic Approach |
|---|---|---|
| Aquagenic Urticaria | Hives and itching after contact with any water. | Careful history, water challenge test. |
| Solar Urticaria | Hives and itching after sun exposure. | Phototesting. |
| Cold Urticaria | Hives and itching after exposure to cold. | Cold stimulation tests. |
| Exercise-Induced Anaphylaxis | Severe allergic reaction triggered by exercise, often with food or medication involvement. | History, allergy testing, exercise challenge test. |
| Pressure Urticaria | Hives and swelling in areas subjected to pressure. | Clinical assessment based on history and physical examination. |
What is a very rare allergy?

Defining "very rare" in the context of allergies is challenging because prevalence data often varies depending on the study population and diagnostic methods. However, allergies affecting a minuscule percentage of the population, often with poorly understood mechanisms, can be considered very rare. These frequently involve reactions to specific proteins or compounds found in uncommon substances or even environmental exposures. Accurate diagnosis can be difficult, sometimes requiring extensive testing and specialist consultations. The severity of reactions can range widely, from mild skin irritation to life-threatening anaphylaxis.
Allergy to Alpha-Gal
Alpha-gal syndrome (AGS) is a rare allergy triggered by a carbohydrate molecule called alpha-gal, found in the meat of mammals like beef, pork, and lamb. It's usually discovered after a tick bite that transmits a specific type of tick saliva. The reaction can be delayed, manifesting hours after consuming meat, making diagnosis complex. It's estimated to affect a small but growing population.
- Symptoms can include hives, itching, swelling, vomiting, and diarrhea.
- Severe reactions can lead to anaphylaxis, requiring immediate medical attention.
- Diagnosis involves blood tests looking for IgE antibodies against alpha-gal.
Latex Allergy
While latex allergy itself isn't exceptionally rare, certain types of latex allergies, especially those manifesting as specific hypersensitivity reactions to particular proteins in natural rubber latex, are considered unusual. These can be far more severe and challenging to manage than common latex allergies.
- Type I reactions (immediate hypersensitivity) are more common but some individuals experience delayed reactions.
- Symptoms vary from mild skin irritation and itching to severe respiratory distress and anaphylaxis.
- Avoiding contact with latex products is crucial, but trace amounts can be difficult to avoid in many consumer goods.
Allergy to Insect Venom
While allergies to common stinging insects like bees and wasps are relatively well-known, allergies to the venom of less common insects, such as certain species of ants, hornets, or spiders, are much rarer. These can present with serious and potentially life-threatening consequences due to the less readily available specific immunotherapy options.
- Reactions can range from localized swelling and pain to systemic anaphylaxis.
- Desensitization therapy (immunotherapy) may be an option, but it's often challenging to obtain due to the rarity of the venom.
- Accurate identification of the insect species responsible is crucial for diagnosis and management.
Jellyfish Sting Allergy
Although jellyfish stings are relatively common, severe allergic reactions to specific jellyfish venom components are considered unusual. The diverse array of venomous compounds in various jellyfish species results in a complex spectrum of allergic reactions.
- Symptoms may vary from mild irritation and pain to potentially life-threatening anaphylaxis.
- The severity of the reaction often depends on the type of jellyfish, the amount of venom injected, and the individual's immune response.
- Treatment focuses on managing symptoms, and in severe cases, may involve antivenom if available.
Allergy to Specific Food Proteins
While common food allergies (e.g., peanuts, milk, eggs) are well-documented, allergies to very specific proteins within certain foods are rare and may not be readily identifiable through standard allergy testing. These uncommon allergies often involve reactions to minor components rather than the major allergenic proteins typically analyzed.
- These allergies can be challenging to diagnose and require specialized testing.
- Symptoms can mimic other conditions, leading to misdiagnosis.
- Strict avoidance of the offending food is the primary treatment.
What is the deadliest allergy?
There isn't a single "deadliest" allergy, as the severity of an allergic reaction depends on several factors including the individual's sensitivity, the amount of allergen encountered, and the speed and effectiveness of treatment. Allergies to things that cause a rapid and severe systemic reaction, like anaphylaxis, are potentially life-threatening. These can be triggered by a wide range of substances, including foods, insect stings, medications, and latex. The speed of the reaction is crucial; some allergens cause immediate and severe reactions, while others might cause delayed reactions that are still life-threatening. The most dangerous allergies are those that most frequently trigger anaphylaxis.
Food Allergies and Anaphylaxis
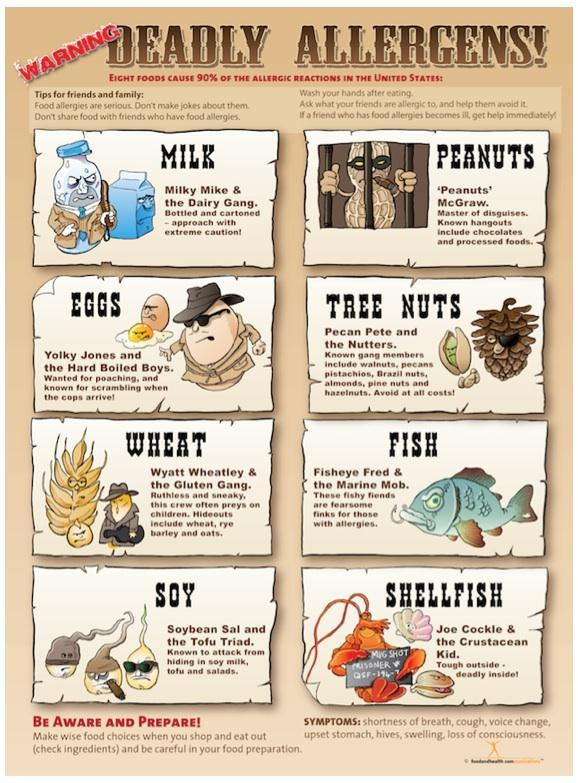
Food allergies are a common cause of severe allergic reactions, with peanuts, tree nuts, milk, eggs, soy, wheat, fish, and shellfish being the most frequent culprits. Anaphylaxis, a severe, life-threatening allergic reaction, can occur within minutes of exposure. Symptoms include difficulty breathing, swelling of the throat and tongue, hives, dizziness, and a drop in blood pressure. Early recognition and treatment with epinephrine are critical for survival.
- Peanuts: A leading cause of fatal anaphylaxis, often requiring lifelong avoidance.
- Tree Nuts: Including walnuts, almonds, cashews, etc., these cause similar severe reactions to peanuts.
- Milk: A common childhood allergy that can persist into adulthood, triggering severe reactions in sensitive individuals.
Insect Sting Allergies
Insect stings, particularly from bees, wasps, hornets, and yellow jackets, can cause life-threatening allergic reactions. The venom injected contains proteins that can trigger anaphylaxis in susceptible individuals. Symptoms can develop rapidly, even in people with no prior history of reactions. The amount of venom injected and the individual’s sensitivity play a crucial role in determining the severity of the reaction. Immediate treatment with epinephrine is essential.
- Bee stings: A common cause of anaphylaxis, often requiring emergency treatment.
- Wasp stings: Similar to bee stings in their potential for severe reactions.
- Hymenoptera venom: This refers to the venom from bees, wasps, hornets, and ants, all of which can cause severe allergic reactions.
Medication Allergies
Certain medications, such as penicillin and other antibiotics, can trigger severe allergic reactions including anaphylaxis. These reactions can be life-threatening and require immediate medical attention. It is vital to inform healthcare providers of any known allergies before receiving medication. Some medications might trigger a reaction even if the patient has tolerated them previously. Always consult a doctor or pharmacist to ensure safety.
- Penicillin: A well-known cause of severe allergic reactions, including anaphylaxis.
- NSAIDs: Nonsteroidal anti-inflammatory drugs like ibuprofen and naproxen can cause anaphylaxis in rare instances.
- Contrast dyes: Used in medical imaging, these can trigger allergic reactions in some individuals.
Latex Allergy
Latex allergy is a significant concern for healthcare workers and individuals with frequent exposure to latex products. Contact with latex can cause a range of reactions, from mild skin irritation to life-threatening anaphylaxis. The proteins in natural rubber latex are responsible for causing allergic reactions. The severity can vary depending on the concentration of latex proteins and individual sensitivity. Avoiding latex exposure is crucial for those with known allergies.
- Type I hypersensitivity: This is the most severe form of latex allergy, involving immunoglobulin E (IgE) antibodies and potential for anaphylaxis.
- Contact dermatitis: A less severe reaction that manifests as skin irritation and inflammation.
- Occupational exposure: Healthcare workers are at higher risk of developing latex allergy due to frequent contact with latex products.
Diagnosis and Management of Severe Allergies
Accurate diagnosis of allergies is crucial for effective management and preventing life-threatening reactions. Allergy testing, including skin prick tests and blood tests, helps identify specific allergens. For individuals at risk of anaphylaxis, carrying an epinephrine auto-injector (like an EpiPen) and knowing how to use it is vital. Regular follow-up with an allergist is also recommended to monitor the allergy and adjust treatment as needed. Emergency medical care should be sought immediately if anaphylaxis is suspected.
- Skin prick tests: A common method for allergy testing.
- Blood tests: Measure IgE antibody levels against specific allergens.
- Epinephrine auto-injectors: Essential for treating anaphylaxis in emergency situations.
What are the top 7 allergies?
What are the Top 7 Allergies?
Determining the exact "top" 7 allergies is challenging because prevalence varies based on geographic location, age, and other factors. However, based on widespread data and studies, the following represent some of the most common allergies globally:
- Milk
- Eggs
- Peanuts
- Tree nuts (e.g., walnuts, pecans, cashews)
- Soy
- Wheat
- Fish (and shellfish)
1. Prevalence and Age of Onset for Top Food Allergies
Food allergies, particularly those listed above, affect a significant portion of the population, with children exhibiting a higher prevalence than adults. Many food allergies manifest early in life, sometimes in infancy, while others can develop later. Early diagnosis and management are crucial to prevent serious reactions.
- Early detection through allergy testing is vital.
- Careful dietary management is necessary to avoid exposure to allergens.
- Emergency epinephrine auto-injectors (like EpiPens) are essential for severe reactions.
2. Symptoms of Allergic Reactions
Allergic reactions can vary widely in severity, ranging from mild to life-threatening. Symptoms can include skin rashes (hives, eczema), itching, swelling (angioedema), digestive issues (nausea, vomiting, diarrhea), respiratory problems (wheezing, coughing, shortness of breath), and in severe cases, anaphylaxis (a medical emergency characterized by a sudden drop in blood pressure and difficulty breathing).
- Mild reactions might involve itching or a rash.
- Moderate reactions can include vomiting, swelling, and difficulty breathing.
- Severe reactions (anaphylaxis) require immediate medical attention.
3. Diagnosis and Testing for Allergies
Diagnosing allergies often involves a combination of methods. A doctor will review your medical history and symptoms, and may conduct skin prick tests or blood tests to identify specific allergens. Accurate diagnosis is essential to guide appropriate management and avoid future exposures.
- Skin prick tests involve pricking the skin with a small amount of allergen.
- Blood tests measure allergen-specific IgE antibodies in the blood.
- Oral food challenges, under medical supervision, might be used in some cases.
4. Management and Treatment of Allergies
The primary management strategy for allergies is allergen avoidance. This involves carefully reading food labels, being cautious in social situations where food is served, and communicating allergy information to others. Medication, such as antihistamines and corticosteroids, can help manage symptoms, while epinephrine is crucial for treating severe anaphylaxis.
- Strict avoidance of the allergen is the cornerstone of management.
- Antihistamines can relieve mild symptoms such as itching and sneezing.
- Corticosteroids may be used for more severe symptoms or inflammation.
5. Research and Future Directions in Allergy Treatment
Ongoing research is exploring various approaches to allergy treatment, including immunotherapy (allergy shots or sublingual tablets). Immunotherapy aims to desensitize the immune system to specific allergens over time, reducing the severity of allergic reactions. Future research may also focus on identifying new treatments and preventative strategies.
- Immunotherapy is a promising approach for long-term management of allergies.
- Research is ongoing to develop new, more effective treatments.
- Understanding the genetic and environmental factors involved in allergy development is crucial for prevention.
What is the most allergic thing in the world?

There is no single "most allergic thing in the world." Allergic reactions are highly individual and depend on a person's immune system response. What causes a severe reaction in one person might cause a mild reaction or no reaction at all in another. The severity of an allergic reaction also depends on factors like the amount of allergen encountered, the route of exposure (inhalation, ingestion, skin contact), and individual factors like age and overall health. Therefore, ranking allergens by their allergenicity is impossible and misleading. Different allergens affect different populations differently, and prevalence varies geographically.
Prevalence of Allergens
The prevalence of allergens varies significantly based on geographical location, environmental factors, and lifestyle. For example, pollen allergies are more common in areas with abundant plant life, while food allergies can be influenced by dietary habits. Certain allergens, like pollen from certain plants and specific food proteins, are more widely recognized as prevalent causes of allergic reactions. However, this prevalence doesn't equate to inherent allergenicity.
- Pollen: Grass pollen, tree pollen, and weed pollen are common culprits, with seasonal variations impacting the severity of allergic responses.
- Food allergens: Peanuts, tree nuts, milk, eggs, soy, wheat, fish, and shellfish are among the most common food allergens, but reactions vary greatly between individuals.
- Insect stings: Bee, wasp, and hornet stings can trigger severe allergic reactions, including anaphylaxis, in susceptible individuals.
Severity of Allergic Reactions
Allergic reactions range widely in severity, from mild symptoms like itchy skin or sneezing to life-threatening anaphylaxis. Anaphylaxis is a severe, potentially fatal allergic reaction that requires immediate medical attention. The severity of a reaction isn't solely determined by the allergen itself; individual factors and the amount of allergen exposure play crucial roles.
- Mild reactions may include: runny nose, itchy eyes, hives.
- Moderate reactions can manifest as: swelling, difficulty breathing, gastrointestinal issues.
- Severe reactions (anaphylaxis) involve: life-threatening symptoms like difficulty breathing, drop in blood pressure, and loss of consciousness.
Individual Sensitivity
Individual sensitivity to allergens is unique and can change over time. What causes a mild reaction in one person may trigger a severe reaction in another. Genetic predisposition, age, and environmental factors all play a role in shaping a person's allergic profile. Even the same individual may experience varying reactions to the same allergen depending on various circumstances.
- Genetic factors influence susceptibility to allergies.
- Exposure to allergens at a young age can influence future reactivity.
- Environmental factors, such as air pollution, can exacerbate allergic responses.
Types of Allergic Reactions
Allergic reactions can manifest in diverse ways, affecting different parts of the body. The symptoms experienced depend on the allergen, the route of exposure, and the individual's immune response. Understanding the different types of allergic reactions helps in diagnosing and managing allergic conditions effectively.
- Type I hypersensitivity: Involves IgE antibodies, often causing immediate reactions like hives, asthma, or anaphylaxis.
- Type IV hypersensitivity: A delayed reaction involving T cells, often seen in contact dermatitis (e.g., poison ivy).
- Other types of hypersensitivity reactions exist, but are less common in relation to simple allergen exposure.
Diagnosis and Management of Allergies
Diagnosing allergies usually involves a combination of medical history, physical examination, and allergy testing (skin prick tests, blood tests). Effective management of allergies involves allergen avoidance, medication (antihistamines, corticosteroids, epinephrine), and immunotherapy (allergy shots). Early diagnosis and appropriate management are crucial in preventing severe reactions and improving the quality of life for people with allergies.
- Allergy testing helps identify specific allergens.
- Medication can alleviate symptoms and prevent severe reactions.
- Immunotherapy may desensitize individuals to specific allergens over time.
What is considered the rarest allergy?
Pinpointing the single rarest allergy is difficult due to underreporting and varying diagnostic criteria across different regions. Many allergies are uncommon, and their rarity often depends on factors like geographic location and exposure. However, allergies to specific components of certain foods, insects, or even environmental elements are often cited as incredibly rare. For example, allergies to certain types of tree pollen that are geographically restricted, like specific species found only in remote areas, might qualify. Similarly, allergies to certain exotic fruits or seafood varieties might be incredibly rare due to limited exposure in the general population. The diagnosis itself is crucial; a seemingly rare reaction might be misdiagnosed or simply go unreported. Research on allergies is constantly evolving, and as new allergens are identified and diagnostic techniques improve, the understanding of true rarity shifts. Furthermore, allergic reactions themselves can be varied in their presentation, complicating the identification of a rare allergy. A seemingly unique reaction might be a variation of a more common allergy, further blurring the lines when determining true rarity.
Are there allergies so rare they're virtually unknown?
While it's unlikely an allergy exists that is completely unknown to medical science, the possibility of undiagnosed or unreported allergies is certainly a factor. The complexity of the immune system and the vast number of potential allergens mean there could be allergic reactions to substances yet to be identified or linked to a specific allergen. Many individuals might experience unusual reactions that they or their doctors attribute to other causes, leaving the underlying allergy undiagnosed. Furthermore, in regions with limited access to advanced medical care, rare allergic reactions might go unreported, skewing the data on allergy prevalence. The rarity of certain allergies also stems from limited exposure. Someone may only be exposed to a specific allergen once or twice in their lifetime, never experiencing a reaction strong enough to trigger a diagnosis. Therefore, the answer is a nuanced one. While it's highly probable that allergies exist that are exceptionally uncommon and perhaps unknown to wider scientific communities, the actual existence of an entirely unknown allergy is difficult to prove or disprove.
How are rare allergies diagnosed?
Diagnosing rare allergies presents unique challenges. Standard allergy tests, such as skin prick tests or blood tests (like IgE antibody testing), might not be effective for identifying uncommon allergens if the necessary testing components aren't readily available. Often, a thorough medical history is crucial, involving detailed questioning about potential exposures and symptoms. Elimination diets might be employed, where suspected allergens are removed from a patient's diet to see if symptoms improve. However, this approach is time-consuming and can be difficult to manage. Challenge tests, involving controlled exposure to potential allergens under medical supervision, are sometimes used but carry inherent risks. Advanced testing methods, such as molecular allergy testing, offer the potential for greater specificity, but these methods are often not widely accessible. Ultimately, accurate diagnosis often relies on a combination of careful clinical observation, patient history, and sophisticated testing techniques, with close collaboration between the patient and specialized allergists who are experienced in dealing with unusual presentations.
What are the treatments for rare allergies?
Treatment for rare allergies often follows similar principles to those for more common allergies, albeit with increased challenges. Avoiding the allergen is the cornerstone of management. However, this can be incredibly difficult with rare allergens that are not easily identifiable or avoidable. Antihistamines, such as cetirizine or loratadine, and corticosteroids can help manage symptoms, but their effectiveness might vary depending on the severity and type of reaction. Epinephrine (adrenaline) auto-injectors are crucial for managing severe allergic reactions (anaphylaxis), even for rare allergens. In some instances, allergy immunotherapy (desensitization) might be considered, although its effectiveness and feasibility for rare allergies are case-dependent and require careful consideration of the risks and benefits. For very uncommon allergies, research and development of targeted therapies may be limited, making the treatment primarily focused on managing the symptoms and mitigating the risk of severe reactions. The collaborative approach between patient, allergist, and potentially other specialists is paramount in developing effective and safe management strategies for rare and unusual allergic conditions.

Deja una respuesta