Which food is the most antihistamine

Allergies can cause a variety of symptoms, including sneezing, runny nose, itchy eyes, and congestion. Antihistamines are medications that can help to relieve these symptoms by blocking the effects of histamine, a chemical that is released by the body during an allergic reaction. But did you know that certain foods can also act as natural antihistamines? In this article, we will explore which foods are the most effective at reducing allergy symptoms and how they can be incorporated into your diet.
Which Foods Naturally Counteract Histamine?
There isn't a single food that acts as a "most antihistamine" in the sense of directly blocking histamine release like a pharmaceutical antihistamine. However, many foods can help manage histamine levels in the body through various mechanisms. These mechanisms include providing enzymes that break down histamine, reducing inflammation, and supporting a healthy gut microbiome, all of which can alleviate allergy symptoms. The best approach involves a combination of dietary choices rather than relying on one "superfood."
1. Foods Rich in DAO (Diamine Oxidase)
Diamine oxidase (DAO) is an enzyme that breaks down histamine in the digestive tract. Foods naturally rich in DAO can help reduce the amount of histamine absorbed into the bloodstream. Fermented foods like sauerkraut, kimchi, and kefir are excellent sources of DAO. Consuming these regularly can assist in managing histamine intolerance. The effectiveness can vary from person to person, and not all fermented foods contain high levels of DAO.
2. Foods with Anti-inflammatory Properties
Inflammation plays a significant role in allergic reactions. Foods rich in antioxidants and omega-3 fatty acids can help reduce inflammation throughout the body. Examples include fatty fish (salmon, mackerel, tuna), leafy green vegetables (spinach, kale), and berries (blueberries, strawberries). By reducing overall inflammation, these foods can indirectly help alleviate histamine-related symptoms.
3. Probiotics for Gut Health
A healthy gut microbiome is crucial for immune function. Probiotics, found in yogurt, kefir, and other fermented foods, can help maintain a balanced gut flora. A balanced gut can contribute to a more efficient immune response and potentially reduce the severity of allergic reactions. It’s important to note that the effects of probiotics can be variable and depend on the specific strains and individual responses.
4. Foods Low in Histamine
While some foods actively counter histamine, others are naturally low in histamine content. Focusing on a diet low in histamine-rich foods (aged cheeses, cured meats, smoked fish, etc.) is essential for managing histamine intolerance. Combining these foods with DAO-rich foods can create a more comprehensive approach to symptom management.
5. The Importance of Individual Tolerance
Individual responses to foods vary greatly. What triggers a reaction in one person may be tolerated by another. Keeping a food diary to identify personal triggers and tolerances is critical for managing histamine-related issues. Consulting with a doctor or registered dietitian can provide personalized guidance on dietary choices.
| Food Category | Examples | Mechanism of Action |
|---|---|---|
| DAO-rich foods | Kefir, sauerkraut, kimchi | Increased histamine breakdown in the gut |
| Anti-inflammatory foods | Fatty fish, leafy greens, berries | Reduced overall inflammation |
| Probiotic-rich foods | Yogurt, kefir, fermented vegetables | Improved gut health and immune function |
| Low-histamine foods | Fresh fruits and vegetables, rice, potatoes | Reduced histamine intake |
Which Foods Naturally Counteract Histamine?
There isn't a single food that acts as a "most antihistamine" in the sense of directly blocking histamine release like a pharmaceutical antihistamine. However, many foods can help manage histamine levels in the body through various mechanisms. These mechanisms include providing enzymes that break down histamine, reducing inflammation, and supporting a healthy gut microbiome, all of which can alleviate allergy symptoms. The best approach involves a combination of dietary choices rather than relying on one "superfood."
1. Foods Rich in DAO (Diamine Oxidase)
Diamine oxidase (DAO) is an enzyme that breaks down histamine in the digestive tract. Foods naturally rich in DAO can help reduce the amount of histamine absorbed into the bloodstream. Fermented foods like sauerkraut, kimchi, and kefir are excellent sources of DAO. Consuming these regularly can assist in managing histamine intolerance. The effectiveness can vary from person to person, and not all fermented foods contain high levels of DAO.
2. Foods with Anti-inflammatory Properties
Inflammation plays a significant role in allergic reactions. Foods rich in antioxidants and omega-3 fatty acids can help reduce inflammation throughout the body. Examples include fatty fish (salmon, mackerel, tuna), leafy green vegetables (spinach, kale), and berries (blueberries, strawberries). By reducing overall inflammation, these foods can indirectly help alleviate histamine-related symptoms.
3. Probiotics for Gut Health
A healthy gut microbiome is crucial for immune function. Probiotics, found in yogurt, kefir, and other fermented foods, can help maintain a balanced gut flora. A balanced gut can contribute to a more efficient immune response and potentially reduce the severity of allergic reactions. It’s important to note that the effects of probiotics can be variable and depend on the specific strains and individual responses.
4. Foods Low in Histamine
While some foods actively counter histamine, others are naturally low in histamine content. Focusing on a diet low in histamine-rich foods (aged cheeses, cured meats, smoked fish, etc.) is essential for managing histamine intolerance. Combining these foods with DAO-rich foods can create a more comprehensive approach to symptom management.
5. The Importance of Individual Tolerance
Individual responses to foods vary greatly. What triggers a reaction in one person may be tolerated by another. Keeping a food diary to identify personal triggers and tolerances is critical for managing histamine-related issues. Consulting with a doctor or registered dietitian can provide personalized guidance on dietary choices.
| Food Category | Examples | Mechanism of Action |
|---|---|---|
| DAO-rich foods | Kefir, sauerkraut, kimchi | Increased histamine breakdown in the gut |
| Anti-inflammatory foods | Fatty fish, leafy greens, berries | Reduced overall inflammation |
| Probiotic-rich foods | Yogurt, kefir, fermented vegetables | Improved gut health and immune function |
| Low-histamine foods | Fresh fruits and vegetables, rice, potatoes | Reduced histamine intake |
What foods flush out histamine?
What Foods Flush Out Histamine?
There's no single food that magically "flushes out" histamine. Histamine is a naturally occurring compound in the body, and its levels are regulated through various metabolic pathways. However, certain foods can help support the body's natural histamine-regulating mechanisms and reduce the symptoms associated with high histamine levels. This primarily involves consuming foods low in histamine and those that support the activity of diamine oxidase (DAO), an enzyme that breaks down histamine. It's crucial to understand that individual responses vary greatly, and what works for one person may not work for another. A proper diagnosis and dietary plan should be guided by a medical professional.
Foods Low in Histamine
Consuming foods naturally low in histamine is a cornerstone of managing histamine intolerance. These foods haven't undergone significant bacterial breakdown which can lead to increased histamine production. Incorporating them into your diet can help reduce the overall histamine load on your body. It's important to note that even low-histamine foods can be problematic in large quantities or if prepared incorrectly.
- Fresh fruits and vegetables: Many fruits and vegetables are naturally low in histamine, especially when fresh and consumed shortly after harvest. Examples include: apples (peeled), bananas, blueberries, carrots, cucumber, green beans, lettuce (some varieties), melon, and pineapple. Avoid overripe or fermented produce.
- Fresh, properly-prepared meats and poultry: Focus on fresh, lean cuts. Proper cooking methods are important; avoid aging or fermenting processes that can increase histamine.
- Fresh fish: Select fresh fish over canned or aged varieties. Ensure freshness is confirmed before consumption.
Foods That Support DAO Activity
Diamine oxidase (DAO) is a crucial enzyme that breaks down histamine. Supporting its activity can help your body process histamine more effectively. Certain foods are thought to boost DAO production or activity.
- Vitamin C-rich foods: Vitamin C plays a role in supporting the immune system and reducing inflammation, which can help modulate histamine response. Examples include citrus fruits (in moderation for those sensitive), bell peppers, and kale.
- Probiotics: A healthy gut microbiome is essential for overall health and may influence histamine metabolism. Foods rich in probiotics, like yogurt (fermented, but low in histamine when plain) and kefir, may offer benefits. The impact is still being researched and may be highly individual.
- Foods rich in antioxidants: Antioxidants help combat oxidative stress, which can indirectly influence histamine levels. Berries, turmeric, and green tea are examples of antioxidant-rich foods.
Foods to Avoid (High Histamine)
Minimizing or eliminating high-histamine foods is a key strategy. These foods contain high levels of pre-formed histamine or can trigger the release of histamine in the body, worsening symptoms. Identifying and eliminating trigger foods is often crucial for managing histamine intolerance.
- Fermented foods: Sauerkraut, kimchi, and aged cheeses are prime examples of foods high in histamine.
- Aged meats and fish: Aged meats like salami, pepperoni, and aged cheeses contain high levels of histamine.
- Processed foods: Many processed foods contain additives that can trigger histamine release.
Managing Histamine Intolerance Through Diet
Successfully managing histamine intolerance often requires a multifaceted approach. It's not merely about avoiding high-histamine foods; it involves actively supporting DAO activity and choosing foods that are less likely to contribute to histamine buildup. Careful meal planning and food preparation are crucial for reducing your exposure to histamine.
- Cook meals fresh: Avoid leftover meals where histamine levels may have increased.
- Use fresh ingredients: Using fresh ingredients is important to avoid high levels of histamine, as it is produced by microbial activity.
- Minimize food additives: Artificial food additives can trigger increased histamine release in sensitive individuals.
The Importance of Consulting a Healthcare Professional
It's critical to consult a doctor or registered dietitian before making significant dietary changes, especially if you suspect you have histamine intolerance. They can help you create a personalized plan, identify your specific triggers, and rule out other potential health conditions. Self-treating can be risky, and professional guidance is essential.
- Professional diagnosis: A healthcare provider can conduct tests to assess for histamine intolerance and rule out other potential issues.
- Personalized dietary plan: A registered dietitian can help develop a tailored dietary plan that fits your individual needs and preferences.
- Monitoring progress: Regular check-ups with your healthcare provider are essential to monitor your progress and adjust your plan as needed.
What is the strongest natural antihistamine?
:max_bytes(150000):strip_icc()/natural-antihistamine-5224433-1c75c98c11b143e5b74f8b1f5abc2a5a.png)
There isn't a single "strongest" natural antihistamine definitively proven by rigorous scientific studies to be superior to all others. The effectiveness of natural remedies varies significantly between individuals due to factors like the severity of allergies, individual sensitivities, and the specific allergen involved. What works well for one person might be ineffective for another. Furthermore, the research on many natural antihistamines is limited and often relies on smaller studies or anecdotal evidence. It's crucial to consult with a healthcare professional before using any natural remedy, particularly if you have pre-existing conditions or are taking other medications.
What are the commonly cited natural antihistamines?
Several natural substances are often touted for their antihistamine-like properties. These include quercetin, bromelain, stinging nettle, butterbur, and vitamin C. However, the scientific evidence supporting their efficacy as strong antihistamines compared to pharmaceutical options is generally lacking. It's important to remember that "natural" doesn't automatically equate to "safe" or "effective." Some natural remedies can have side effects or interact negatively with other medications.
- Quercetin: Found in many fruits and vegetables, it's thought to inhibit histamine release. More research is needed to establish its effectiveness as a potent antihistamine.
- Bromelain: An enzyme from pineapple, it's suggested to possess anti-inflammatory properties that might help manage allergy symptoms. Evidence of its antihistamine effect is limited.
- Stinging Nettle: This herb is often used in alternative medicine for allergies. Although some studies show it may reduce symptoms, more robust research is needed to confirm its strength as an antihistamine.
How do natural antihistamines work differently than pharmaceutical antihistamines?
Pharmaceutical antihistamines directly block histamine receptors, preventing histamine from binding and triggering an allergic reaction. Many natural substances, in contrast, may work through different mechanisms. For example, some may reduce inflammation, which can lessen allergy symptoms, or may inhibit the release of histamine, though the effect may be weaker than dedicated antihistamine drugs. The precise mechanisms of action for many natural remedies are still not fully understood.
- Pharmaceutical Antihistamines: These drugs directly compete with histamine for receptor sites.
- Natural Antihistamines: Their mechanisms are varied and often less direct, potentially including inflammation modulation and histamine release inhibition.
- Effectiveness Comparison: Direct comparisons are difficult due to varying study designs and limited research on natural options.
What are the potential side effects of natural antihistamines?
While generally considered safer than pharmaceutical drugs, natural antihistamines can still cause side effects. These can vary depending on the specific substance and the individual. Some possible side effects include digestive upset, such as nausea, diarrhea, or constipation. Allergic reactions are also possible, even to naturally derived substances. Because the purity and standardization of natural products can be inconsistent, it's crucial to source them from reputable suppliers.
- Gastrointestinal Issues: Nausea, diarrhea, and constipation are common.
- Allergic Reactions: These can range from mild skin irritation to more serious reactions.
- Drug Interactions: Some natural antihistamines can interact with prescription medications.
What is the role of diet in managing allergies?
Diet plays a significant role in allergy management, although it doesn't replace the need for medical treatment if necessary. A balanced diet rich in fruits, vegetables, and whole grains can support overall immune function. Eliminating specific foods that trigger allergic reactions is critical for managing food allergies. However, self-diagnosing and eliminating foods without professional guidance is not recommended. A registered dietitian or allergist can provide personalized advice and help manage dietary restrictions.
- Anti-inflammatory Foods: Fruits, vegetables, and omega-3 fatty acids can reduce inflammation.
- Allergen Avoidance: Identifying and eliminating trigger foods is essential for managing food allergies.
- Personalized Dietary Plans: Registered dietitians or allergists can help create suitable dietary plans.
Are there any interactions with other medications?
Yes, some natural antihistamines can interact with other medications. This is particularly important for individuals taking prescription drugs for other conditions. It’s vital to inform your doctor or pharmacist about all supplements and herbal remedies you are taking, including natural antihistamines. Some natural substances can either enhance or weaken the effects of other medications, leading to unintended consequences.
- Always disclose supplements: Inform your doctor about all supplements before starting treatment.
- Potential interactions: Certain natural antihistamines may interact with blood thinners, immune suppressants, etc.
- Professional Guidance: Consult a healthcare professional to assess potential drug interactions.
Which food has high histamine?
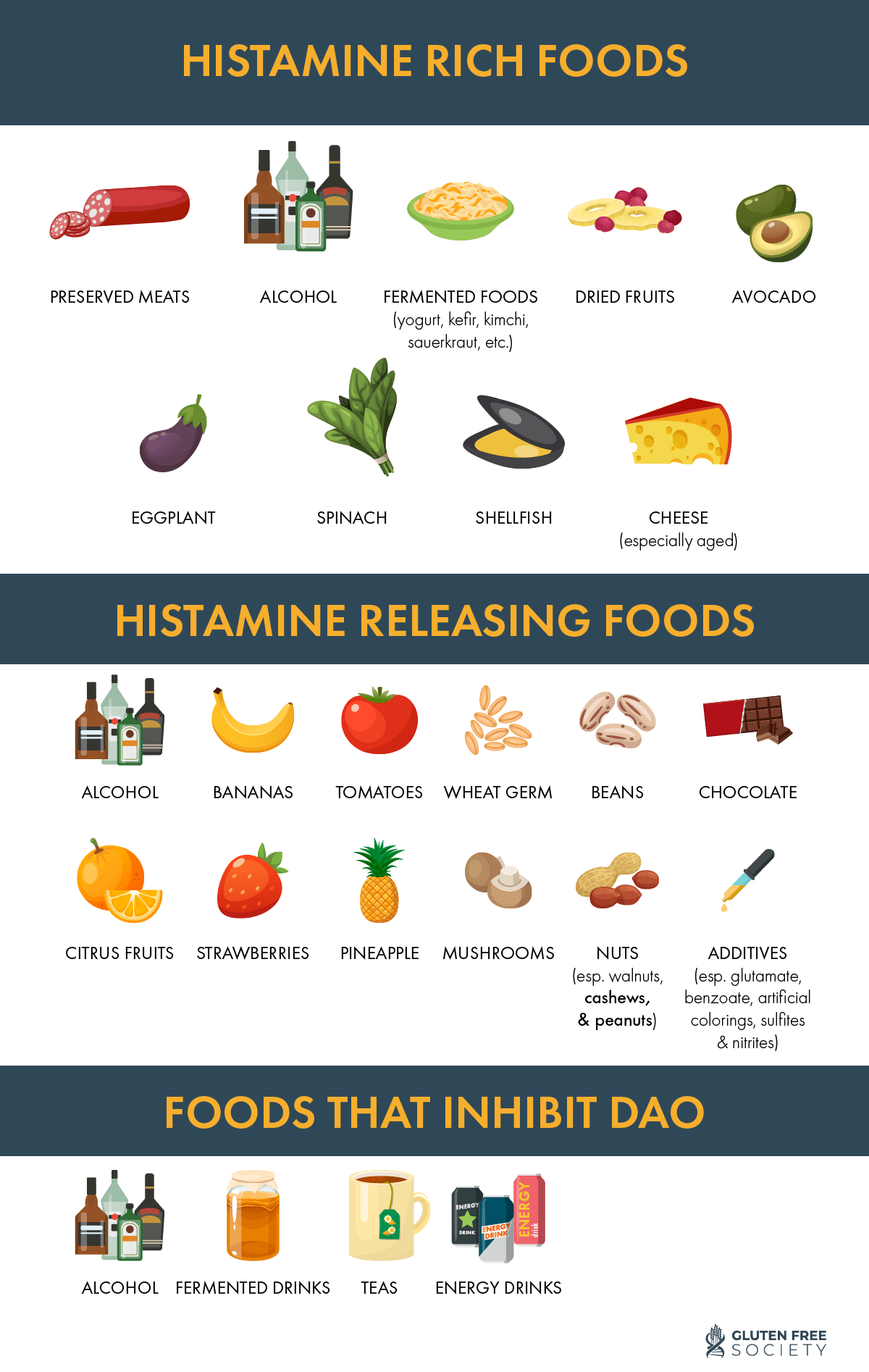
Many foods contain histamine, a compound naturally present in the body and also produced by bacteria during the fermentation and spoilage of food. Foods high in histamine can trigger reactions in individuals with histamine intolerance or mast cell activation syndrome. The amount of histamine in food is variable and affected by factors like freshness, processing, and storage. It's difficult to give exact numbers, as histamine levels fluctuate. However, certain foods are consistently associated with high histamine content.
Fermented Foods
Fermentation is a major contributor to high histamine levels in food. Bacteria involved in fermentation produce histamine as a byproduct. This makes fermented foods a common trigger for histamine intolerance. The longer the fermentation process, generally the higher the histamine levels.
- Sauerkraut: A popular fermented cabbage dish.
- Kimchi: A spicy fermented Korean cabbage dish.
- Yogurt (some types): While some yogurts are low in histamine, those made with longer fermentation times can have higher levels.
Aged Foods
The aging process, particularly in meats and cheeses, also leads to increased histamine production. The longer the aging process, the more likely a food is to contain high histamine levels. Bacteria are responsible for this increase in histamine, which is responsible for the unique flavors of aged products.
- Aged cheeses (Cheddar, Parmesan, etc.): These cheeses often have high histamine content.
- Cured meats (salami, pepperoni, etc.): These meats undergo a curing process which can result in significant histamine accumulation.
- Aged fish (tuna, mackerel, etc.): The aging process affects histamine levels considerably. Improper storage can exacerbate this effect.
Certain Fish and Seafood
Certain types of fish and seafood are known for having naturally higher levels of histamine, even when fresh. This is partly due to the fish's own metabolic processes and the presence of histamine-producing bacteria. Improper handling and storage can significantly increase histamine levels in these foods.
- Tuna: Particularly when canned or improperly stored.
- Mackerel: High histamine levels are often found.
- Anchovies: Known for higher histamine content.
Processed Meats
Many processed meats contain high levels of histamine. This is partly due to the processing methods, which can encourage bacterial growth and histamine production. Additives and preservatives sometimes used in processed meats may also impact histamine levels. The longer the shelf life of the meat, the more likely it is to have elevated histamine.
- Bacon: The curing process can lead to high histamine.
- Sausages: Depending on the type and preparation, they often contain significant histamine.
- Lunch Meats: Many lunch meats are known to have higher than average levels of histamine.
Other High-Histamine Foods
Beyond the categories above, several other foods are frequently implicated in histamine intolerance. It's crucial to pay attention to individual reactions, as sensitivity varies. Keeping a food diary can be helpful in pinpointing specific triggers.
- Spinach: Can contain considerable levels of histamine.
- Tomatoes: Often cited as a potential trigger.
- Avocados: Although a healthy food, it can be high in histamine for some individuals.
What is a very strong antihistamine?
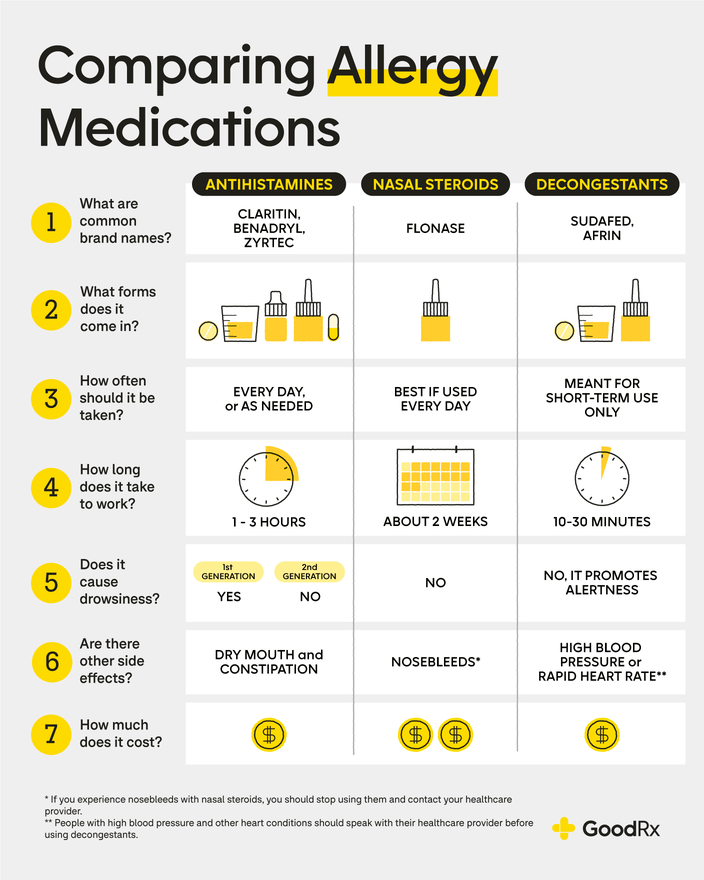
The concept of a "very strong" antihistamine is relative and depends on individual needs and the specific symptoms being treated. There isn't one single antihistamine universally considered the "strongest." The strength is determined by factors like how effectively it blocks histamine receptors and its duration of action. However, some antihistamines are generally considered more potent or longer-lasting than others. Second-generation antihistamines, like cetirizine (Zyrtec), fexofenadine (Allegra), and loratadine (Claritin), are often preferred over first-generation antihistamines due to their lower incidence of sedative side effects. These are generally considered to be more effective for relieving allergy symptoms than older first-generation options. However, even within the second-generation class, potency can vary slightly depending on individual responses. The best antihistamine for any particular person will depend on factors such as their specific allergy symptoms, other medications they are taking, and potential side effects.
What are the different types of antihistamines?
Antihistamines are broadly classified into two generations: first-generation and second-generation. First-generation antihistamines, such as diphenhydramine (Benadryl) and chlorpheniramine, are older medications that are readily available over the counter. They are often more likely to cause drowsiness but can be effective for relieving allergy symptoms. Second-generation antihistamines, such as cetirizine, fexofenadine, and loratadine, are generally less sedating and are often preferred for daily use.
- First-generation antihistamines: Often cause drowsiness, but can be effective for short-term relief.
- Second-generation antihistamines: Generally less sedating, suitable for long-term use.
- Third-generation antihistamines: A newer class with even fewer side effects but not as widely available.
How do antihistamines work?
Histamine is a chemical released by the body in response to allergens like pollen or pet dander. It triggers allergic symptoms like sneezing, itching, and runny nose. Antihistamines work by blocking histamine receptors, preventing histamine from binding and causing these symptoms. Different antihistamines have varying affinities for different histamine receptors, leading to differences in their efficacy and side-effect profiles.
- Bind to histamine receptors: Prevents histamine from triggering allergic responses.
- Reduce inflammation: Some antihistamines also have anti-inflammatory properties.
- Relieve symptoms: Alleviate allergy symptoms like sneezing, itching, and runny nose.
What are the potential side effects of strong antihistamines?
While second-generation antihistamines are generally well-tolerated, side effects can still occur. The most common side effects include drowsiness (though less frequent with second-generation drugs), headache, dry mouth, and nausea. First-generation antihistamines are significantly more likely to cause drowsiness and other side effects. Always consult a doctor or pharmacist before using any antihistamine, especially if you have other health conditions or are taking other medications.
- Drowsiness: Particularly common with first-generation antihistamines.
- Dry mouth: A common side effect of many antihistamines.
- Headache: Can occur with some antihistamines.
When should I see a doctor about my allergies?
If your allergy symptoms are severe, persistent, or unresponsive to over-the-counter antihistamines, it's crucial to consult a doctor. A doctor can diagnose the specific allergen(s) causing your symptoms and recommend the most appropriate treatment, including prescription-strength antihistamines or other allergy management strategies. Don't hesitate to seek professional medical advice if your allergies significantly impact your quality of life.
- Severe allergy symptoms: Difficulty breathing, swelling, hives.
- Unresponsive symptoms: Over-the-counter treatments are ineffective.
- Persistent symptoms: Allergies persist despite treatment.
What foods are naturally antihistamine?
There isn't one single food that acts as a powerful, universally effective antihistamine. The concept of a food being "antihistamine" is a bit of a simplification. Histamine is a chemical compound involved in allergic reactions, and certain foods can either reduce histamine levels in the body or inhibit histamine release. However, the effectiveness varies significantly from person to person due to individual sensitivities and the complexity of allergic reactions. Foods often cited for their potential antihistamine properties include those rich in quercetin, a flavonoid antioxidant found in onions, apples, berries, and leafy green vegetables. These foods may help to stabilize mast cells, preventing the release of histamine. Foods fermented with probiotics, such as yogurt and kefir, may also contribute to gut health, which can indirectly affect the immune system and potentially reduce the severity of allergic responses. It's crucial to remember that these foods are not a replacement for medication prescribed by a doctor for allergies. They are best considered as part of a holistic approach to managing allergy symptoms, potentially reducing their severity when incorporated into a balanced diet. The impact on individual histamine levels can be subtle and dependent on many factors including overall diet, gut microbiome, and the specific allergen involved. More research is needed to fully understand the complex interactions between diet and histamine release.
Are there foods that actually block histamine?
While no food perfectly "blocks" histamine in the same way an antihistamine medication does, some foods can help reduce the body's production of histamine or prevent its release from mast cells. The mechanism is not a direct blockade, but rather a modulation of the immune response. Foods rich in vitamin C, for example, are thought to have an anti-inflammatory effect and may indirectly help reduce histamine production. Similarly, foods containing bromelain, an enzyme found in pineapple, possess anti-inflammatory properties and may help to reduce swelling and inflammation often associated with histamine release. Furthermore, some studies suggest that foods high in omega-3 fatty acids, such as fatty fish, can contribute to a less inflammatory environment in the body. However, it's critical to understand that the impact of these foods is typically mild compared to pharmaceutical antihistamines. Their effectiveness varies greatly between individuals, and they should be viewed as supplementary, not replacement, strategies for managing allergies. A balanced diet rich in these beneficial components is always advisable, but should not be seen as a cure for allergies.
Which foods should I avoid if I have high histamine levels?
Managing high histamine levels often involves avoiding certain histamine-rich foods. These are foods that contain naturally high levels of histamine or that promote the release of histamine in the body. These can vary depending on individual sensitivities, but common culprits include fermented foods (unless specifically fermented with probiotic strains considered beneficial), aged cheeses, cured meats, smoked fish, spinach, tomatoes, and alcohol. Additionally, foods containing tyramine, a compound that can increase histamine levels, should also be limited. This includes many aged cheeses and fermented products. It’s essential to note that the impact of these foods can vary significantly, and an elimination diet guided by a doctor or registered dietitian is usually recommended to identify personal triggers. A careful food journal documenting symptoms after consuming different foods can be immensely helpful in this process. The goal is not necessarily to eliminate all of these foods entirely, but rather to understand personal tolerance levels and manage consumption accordingly. It's a process of trial and error to determine what works best for each individual. Remember, this should be done in consultation with a healthcare professional.
Can diet completely replace antihistamine medication?
No, diet alone cannot completely replace antihistamine medication for most individuals with allergies. While dietary changes can play a supportive role in managing allergy symptoms and potentially reducing their severity, they do not provide the same level of immediate and targeted relief as pharmaceutical antihistamines. Pharmaceutical antihistamines work directly to block histamine receptors, providing a quick and often powerful effect in alleviating allergy symptoms like sneezing, itching, and runny nose. Dietary modifications might help reduce the underlying inflammation and frequency of allergic responses over time, but they are not a substitute for medication when immediate relief is needed or when allergic reactions are severe. It is always crucial to consult with a doctor or allergist for diagnosis and treatment of allergies. They can help determine the appropriate course of action, which may include medication alongside dietary adjustments. Relying solely on diet to manage significant allergic reactions can be risky and potentially dangerous.

Deja una respuesta