Why are my allergies so bad right now

Spring has sprung, and with it comes the dreaded arrival of allergy season. For many, this means a runny nose, itchy eyes, and a constant feeling of congestion. But why are allergies so bad right now, and what can you do to relieve your symptoms? Read on to find out.
Why Are My Allergies So Bad Right Now?
Experiencing a sudden worsening of your allergies can be incredibly frustrating and uncomfortable. Several factors can contribute to this increase in severity, making it challenging to pinpoint the exact cause. It's often a combination of environmental triggers, your body's changing sensitivity, and potentially even underlying health conditions. Let's explore some of the key possibilities.
Increased Pollen Counts
Pollen counts fluctuate significantly throughout the year, depending on factors like weather patterns, plant types in your area, and the time of year. High pollen counts, particularly from trees, grasses, or weeds, can dramatically worsen allergy symptoms. Warm, windy days often exacerbate pollen dispersal, leading to higher concentrations in the air you breathe. Monitoring local pollen forecasts is crucial for managing allergy symptoms effectively. If pollen counts are particularly high, consider staying indoors more, closing windows, and using an air purifier.
Mold Spores
Mold spores, microscopic fungal organisms, are another significant allergen. High humidity and damp environments promote mold growth, both indoors and outdoors. Following heavy rainfall or periods of high humidity, mold spore counts can surge, triggering allergic reactions in susceptible individuals. In addition to outdoor sources, mold can thrive in damp areas within your home, such as basements, bathrooms, and areas with water leaks. Addressing moisture problems and ensuring good ventilation is key to minimizing mold exposure.
Changes in Your Immune System
Your body's immune response to allergens isn't static. Factors like stress, illness, and even hormonal changes can affect your immune system's sensitivity. A weakened immune system might react more strongly to allergens, leading to more severe allergy symptoms. Similarly, hormonal fluctuations, particularly in women, can influence allergy susceptibility. Prioritizing stress management techniques and maintaining good overall health can contribute to a more robust immune response.
New or Emerging Allergens
You might develop allergies to substances you haven't previously reacted to. This could be due to exposure to new plants or pollens in your environment, a change in your living situation, or even exposure to new pet dander. Also, certain environmental factors can trigger the onset or worsening of pre-existing allergies. Identifying these new triggers can be challenging, but keeping a detailed allergy diary and observing symptom patterns can offer insights.
Medication Changes or Interactions
Certain medications can either worsen allergy symptoms or interact with allergy medications, potentially leading to unexpected side effects. For example, some medications can suppress the immune system, making you more susceptible to allergic reactions. Always inform your doctor or pharmacist about all medications you are taking, including over-the-counter drugs, to avoid potential interactions and ensure the safe and effective management of your allergies. It's crucial to have a discussion with a healthcare professional about any changes to your medication regime and their potential impact on your allergies.
| Factor | Impact on Allergy Severity | Mitigation Strategies |
|---|---|---|
| High Pollen Counts | Increased allergen exposure, leading to severe symptoms. | Monitor pollen forecasts, stay indoors during peak pollen times, use air purifiers. |
| Mold Spores | High humidity promotes mold growth, triggering reactions. | Address moisture problems in your home, improve ventilation, use dehumidifiers. |
| Immune System Changes | Weakened immune response can amplify allergic reactions. | Manage stress, maintain a healthy lifestyle, get sufficient sleep. |
| New Allergens | Exposure to previously unencountered allergens. | Keep an allergy diary, identify potential new triggers. |
| Medication Interactions | Certain drugs can exacerbate allergies or interact with allergy medication. | Consult your doctor or pharmacist about medication interactions. |
Why Are My Allergies So Bad Right Now?
Experiencing a sudden worsening of your allergies can be incredibly frustrating and uncomfortable. Several factors can contribute to this increase in severity, making it challenging to pinpoint the exact cause. It's often a combination of environmental triggers, your body's changing sensitivity, and potentially even underlying health conditions. Let's explore some of the key possibilities.
Increased Pollen Counts
Pollen counts fluctuate significantly throughout the year, depending on factors like weather patterns, plant types in your area, and the time of year. High pollen counts, particularly from trees, grasses, or weeds, can dramatically worsen allergy symptoms. Warm, windy days often exacerbate pollen dispersal, leading to higher concentrations in the air you breathe. Monitoring local pollen forecasts is crucial for managing allergy symptoms effectively. If pollen counts are particularly high, consider staying indoors more, closing windows, and using an air purifier.
Mold Spores
Mold spores, microscopic fungal organisms, are another significant allergen. High humidity and damp environments promote mold growth, both indoors and outdoors. Following heavy rainfall or periods of high humidity, mold spore counts can surge, triggering allergic reactions in susceptible individuals. In addition to outdoor sources, mold can thrive in damp areas within your home, such as basements, bathrooms, and areas with water leaks. Addressing moisture problems and ensuring good ventilation is key to minimizing mold exposure.
Changes in Your Immune System
Your body's immune response to allergens isn't static. Factors like stress, illness, and even hormonal changes can affect your immune system's sensitivity. A weakened immune system might react more strongly to allergens, leading to more severe allergy symptoms. Similarly, hormonal fluctuations, particularly in women, can influence allergy susceptibility. Prioritizing stress management techniques and maintaining good overall health can contribute to a more robust immune response.
New or Emerging Allergens
You might develop allergies to substances you haven't previously reacted to. This could be due to exposure to new plants or pollens in your environment, a change in your living situation, or even exposure to new pet dander. Also, certain environmental factors can trigger the onset or worsening of pre-existing allergies. Identifying these new triggers can be challenging, but keeping a detailed allergy diary and observing symptom patterns can offer insights.
Medication Changes or Interactions
Certain medications can either worsen allergy symptoms or interact with allergy medications, potentially leading to unexpected side effects. For example, some medications can suppress the immune system, making you more susceptible to allergic reactions. Always inform your doctor or pharmacist about all medications you are taking, including over-the-counter drugs, to avoid potential interactions and ensure the safe and effective management of your allergies. It's crucial to have a discussion with a healthcare professional about any changes to your medication regime and their potential impact on your allergies.
| Factor | Impact on Allergy Severity | Mitigation Strategies |
|---|---|---|
| High Pollen Counts | Increased allergen exposure, leading to severe symptoms. | Monitor pollen forecasts, stay indoors during peak pollen times, use air purifiers. |
| Mold Spores | High humidity promotes mold growth, triggering reactions. | Address moisture problems in your home, improve ventilation, use dehumidifiers. |
| Immune System Changes | Weakened immune response can amplify allergic reactions. | Manage stress, maintain a healthy lifestyle, get sufficient sleep. |
| New Allergens | Exposure to previously unencountered allergens. | Keep an allergy diary, identify potential new triggers. |
| Medication Interactions | Certain drugs can exacerbate allergies or interact with allergy medication. | Consult your doctor or pharmacist about medication interactions. |
Why are my allergies so bad all of a sudden?
The sudden worsening of your allergies can be due to a variety of factors. It's not always a simple case of increased pollen counts. Several interacting elements could be at play, making it crucial to consider a range of possibilities rather than assuming a single cause. Your immune system's response to allergens is complex, and its sensitivity can fluctuate significantly over time. Therefore, a seemingly sudden onset of severe allergy symptoms may be the result of a gradual increase in sensitivity that has only recently become noticeable, or a combination of several factors reaching a critical threshold.
Increased Allergen Levels
Higher pollen counts are the most common culprit. Specific weather patterns, like increased wind or rain followed by warm, sunny days, can dramatically increase pollen dispersal. Similarly, changes in local landscaping, such as new construction or extensive planting of allergenic trees or flowers, can significantly impact exposure. Additionally, certain years see higher-than-average pollen production, irrespective of local factors. Consider these possibilities:
- Increased pollen from specific plants: Certain trees, grasses, or weeds may be producing significantly more pollen this year.
- Favorable weather conditions for pollen dispersal: Windy and dry conditions spread pollen more effectively.
- Changes in your environment: New construction or landscaping near your home could introduce new allergens.
Changes in Your Immune System
Your body's response to allergens isn't static. Several factors can influence its sensitivity. Stress, lack of sleep, and illnesses, even mild ones like colds or the flu, can weaken your immune system, making you more susceptible to allergic reactions. Hormonal changes, particularly in women, can also impact allergy severity. It's important to note that these factors don't directly cause allergies, but they can exacerbate existing sensitivities. Consider:
- Recent illness: Even a mild respiratory infection can temporarily lower your immune defenses.
- Stress levels: High stress can weaken the immune system, increasing allergy symptoms.
- Sleep deprivation: Insufficient sleep can negatively impact your immune response.
- Hormonal fluctuations: Women may experience worsening allergies during menstruation or pregnancy.
New Allergens
You may have developed a new allergy altogether. This is particularly relevant if you've recently moved to a new location, started a new job, or adopted a new pet. Exposure to new allergens, such as dust mites in a new home, pet dander from a newly acquired animal, or mold spores in a damp environment, can trigger a reaction. It is also possible to develop allergies later in life. Take into account:
- New living environment: Exposure to new allergens in your home or workplace.
- New pets: Introducing a pet can lead to allergy development or worsening of existing ones.
- Dietary changes: Although less common, certain foods can trigger allergic reactions.
Medication Interactions or Changes
Certain medications can either increase or decrease your susceptibility to allergies. Changes in your medication regimen, whether prescription or over-the-counter, might be playing a role. Some medications can interact with allergy medications, reducing their effectiveness or triggering unforeseen reactions. If you've recently started or stopped a medication, or changed the dosage, consider this possibility. Keep in mind:
- New medications: Some medications can impact the immune system or interact with allergy medications.
- Changes in medication dosage: Adjustments to existing medication can affect allergy symptoms.
- Interaction between medications: Some medications may interact negatively, worsening allergy symptoms.
Environmental Factors
Beyond pollen, other environmental factors can dramatically affect allergy severity. Air pollution, from industrial emissions or wildfires, can irritate respiratory passages, worsening allergy symptoms. Climate change is also playing a significant role, leading to longer pollen seasons and increased allergen concentrations in many regions. Mold growth in damp areas of your home can also contribute significantly. Pay attention to these points:
- Air quality: Poor air quality due to pollution can exacerbate allergy symptoms.
- Mold exposure: Increased humidity or water damage can lead to mold growth and allergic reactions.
- Climate change effects: Longer pollen seasons and higher pollen concentrations due to climate change.
What are the worst months for allergies?

The worst months for allergies vary depending on the specific allergen and geographic location. However, generally speaking, spring and fall are the peak seasons for allergy sufferers. This is because of the abundance of pollen released by trees, grasses, and weeds during these times of year. While some people may experience symptoms year-round, the intensity and prevalence of symptoms are significantly higher during these particular months.
Tree Pollen Season
For many, the worst allergy months begin in early spring, typically March through May, corresponding with the peak pollen production of trees like oak, birch, maple, and elm. This is when trees are releasing their pollen into the air to fertilize other trees. The severity of tree pollen allergies can vary widely depending on factors such as weather conditions (warmer, drier conditions often worsen symptoms) and the specific tree species prevalent in the region.
- High pollen counts: Expect significantly elevated pollen counts during this period.
- Symptom severity: Symptoms like sneezing, runny nose, itchy eyes, and congestion are common and can be intense.
- Regional variations: The exact timing and severity will vary based on local climate and tree species.
Grass Pollen Season
Following the tree pollen season, the grass pollen season typically peaks in late spring and early summer, usually between May and July. Grasses like Bermuda, rye, and Timothy release large amounts of pollen during this period, causing significant problems for those with grass allergies. Wind plays a large role in spreading grass pollen, often carrying it long distances.
- Prevalence: Grass pollen is a particularly common allergen, affecting a large portion of the population.
- Outdoor activities: Symptoms can be particularly troublesome during outdoor activities.
- Geographical impact: The timing and intensity of the grass pollen season will depend on geographical location and weather patterns.
Weed Pollen Season
The third major allergy season often occurs in the late summer and early fall, generally spanning from August to November. This is when weeds like ragweed, pigweed, and Russian thistle release their pollen. Ragweed is notorious for causing intense allergic reactions, and its pollen can travel long distances on the wind. This can be a particularly challenging season for allergy sufferers as it often coincides with back-to-school activities and colder weather.
- Ragweed prominence: Ragweed is a major culprit during this season.
- Extended duration: This allergy season often lasts longer than the tree or grass pollen seasons.
- Overlap with other allergens: There can be overlap with other allergens, making symptoms even more severe.
Mold Spore Season
While pollen is a prominent allergen during specific seasons, mold spores can be a problem year-round, but they're particularly prevalent during warmer, wetter periods. Spring and fall often bring increased humidity and rainfall, creating ideal conditions for mold growth. Mold spores are microscopic particles that can trigger allergic reactions in sensitive individuals. Areas with high humidity and standing water are especially high-risk.
- Year-round potential: Mold spores are a concern throughout the year, but especially during humid seasons.
- Indoor and outdoor sources: Mold can be found both indoors and outdoors.
- Impact of weather: Rainfall and high humidity are crucial factors impacting mold growth.
Indoor Allergens
While outdoor allergens are often the focus of allergy discussions, indoor allergens can also be significant contributors to year-round allergy symptoms. Dust mites, pet dander, and cockroach droppings are common culprits. While these allergens don't have specific peak seasons like pollen, they can be a consistent problem throughout the year, particularly during the winter months when people spend more time indoors. Proper home maintenance, including regular cleaning and use of air purifiers, can help mitigate these issues.
- Dust mites: A common indoor allergen found in bedding and carpets.
- Pet dander: Allergens shed from animals such as cats and dogs.
- Cockroach allergens: Droppings from cockroaches can trigger allergic reactions.
Are allergies worse this year, 2024?
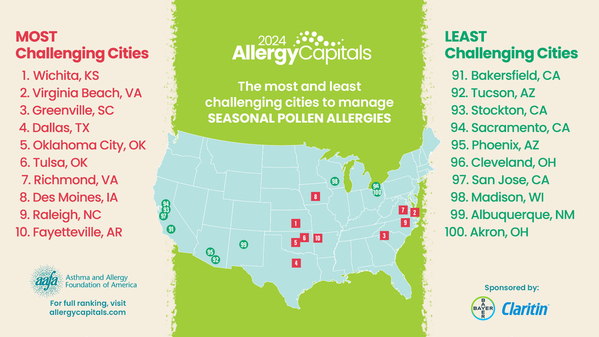
It's difficult to definitively say whether allergies are "worse" in 2024 compared to previous years on a global scale. Allergy severity is highly individual and depends on numerous interacting factors, making broad generalizations challenging. While some regions may be experiencing more intense allergy seasons, others might not. The perceived increase in allergy symptoms could be attributed to several contributing factors rather than a simple worsening of allergies themselves. More research and data are needed for definitive conclusions.
Increased Pollen Counts in Certain Regions
Reports from various pollen monitoring networks suggest significantly higher pollen counts in specific geographical areas during 2024. This increase can be attributed to several factors, including: warmer temperatures leading to earlier and more prolonged pollen seasons, changes in weather patterns causing more intense pollen release, and increased urbanization leading to higher concentrations of allergens in certain areas. These higher counts directly translate to more severe allergy symptoms for susceptible individuals in those affected regions.
- Higher temperatures: Earlier blooming and longer pollen seasons.
- Increased rainfall: Can lead to increased pollen production in some species.
- Climate change effects: Altered weather patterns contribute to variations in pollen production and release.
Impact of Climate Change on Allergy Seasons
Climate change is increasingly recognized as a significant factor influencing allergy seasons. Rising global temperatures, altered precipitation patterns, and increased carbon dioxide levels are all implicated in changes to plant growth and pollen production. These changes can lead to longer and more intense allergy seasons, affecting both the timing and intensity of allergen exposure.
- Longer pollen seasons: Warmer temperatures extend the time plants release pollen.
- Increased pollen production: Some plants produce more pollen under elevated CO2 levels.
- Changes in plant distribution: Shifting ranges of allergen-producing plants.
Improved Allergy Diagnostics and Reporting
It's possible that the perceptionof worse allergies stems from improved diagnostic tools and more widespread reporting of allergy-related illnesses. With increased access to healthcare and more sophisticated allergy testing, more cases are being identified and documented, leading to a potential statistical increase in reported cases without necessarily reflecting an actual increase in allergy prevalence.
- Greater awareness: Increased public awareness of allergies leads to more people seeking diagnosis.
- Advanced testing methods: Better identification of specific allergens leading to more accurate diagnoses.
- Improved data collection: More comprehensive data on allergy prevalence and severity.
Individual Variation in Allergy Symptoms
It is crucial to remember that allergy symptoms vary greatly among individuals. Factors like age, genetic predisposition, overall health, and exposure levels significantly influence the severity of allergic reactions. Even within the same geographical area, the experience of allergy sufferers can differ dramatically. Therefore, generalizations about the overall worsening of allergies need to be made with caution.
- Genetic factors: Inherent susceptibility to specific allergens.
- Environmental factors: Exposure levels to different allergens.
- Comorbidities: Existing health conditions that exacerbate allergies.
Influence of Air Pollution on Allergy Severity
Air pollution interacts significantly with allergens, potentially worsening allergy symptoms. Pollutants can irritate the respiratory system, making individuals more susceptible to allergens. Increased exposure to air pollutants, particularly in urban areas, could be contributing to the severity of allergy symptoms reported in some regions during 2024. The combination of high pollen counts and poor air quality creates a particularly challenging environment for allergy sufferers.
- Irritant effect of pollutants: Increased inflammation and sensitivity in airways.
- Enhanced allergen deposition: Pollutants can carry and deposit allergens more effectively.
- Synergistic effects: Combined effect of pollen and pollutants leading to increased severity.
How to stop allergies immediately?
:max_bytes(150000):strip_icc()/VWH_Illustration_Preventing-and-Treating-Seasonal-Allergies_Danie-Drankwalter_Final-884166d09ac94425ad7e7a3b68a14249.jpg)
How to Stop Allergies Immediately?
There's no single magic bullet to stop allergy symptoms instantly. However, depending on the allergen and the severity of your reaction, several strategies can offer rapid relief. It's crucial to remember that these are temporary measures, and long-term allergy management requires a different approach, often involving medication prescribed by a doctor or allergist. Immediate relief often focuses on managing symptoms rather than eliminating the underlying cause.
Over-the-Counter Medications
Over-the-counter (OTC) antihistamines are your first line of defense against many allergy symptoms. These medications work by blocking histamine, a chemical your body releases during an allergic reaction. They are most effective when taken beforesymptoms start or at the very first sign of an allergic reaction. However, they won't work instantly; it takes time for the medication to reach the affected areas. Different antihistamines have varying onset times. Some provide faster relief than others.
- Diphenhydramine (Benadryl): This is a first-generation antihistamine known for its sedating effects; it can cause drowsiness. It usually starts working within 30-60 minutes.
- Cetirizine (Zyrtec), Fexofenadine (Allegra), Loratadine (Claritin): These are second-generation antihistamines which are generally less sedating than diphenhydramine. They may take longer to provide relief (30-60 minutes) but are longer lasting.
- Decongestants (Pseudoephedrine, Phenylephrine): These can help relieve stuffy noses associated with allergies, often used in conjunction with antihistamines. They typically start working within 30-60 minutes.
Nasal Corticosteroids
Nasal sprays containing corticosteroids, such as fluticasone (Flonase) or mometasone (Nasonex), are very effective for reducing nasal inflammation and relieving symptoms like congestion and sneezing. While they don't provide instant relief, their effects build up over several days. They are best used preventativelyrather than as an immediate solution to a sudden allergy attack.
- Start using them well in advance of known allergy triggers (e.g., pollen season).
- They are not appropriate for immediate relief, but for long-term management.
- Always follow the instructions provided on the packaging or by your doctor.
Eye Drops
For itchy, watery eyes, over-the-counter eye drops containing antihistamines or mast cell stabilizers can provide some relief. These work directly on the eyes, providing faster relief than oral antihistamines. However, the effect might not be instantaneous, and they will only address the eye-related symptoms.
- Look for eye drops containing antihistamines (e.g., ketotifen) or mast cell stabilizers (e.g., cromolyn sodium).
- Always follow the instructions on the packaging, as overuse can cause irritation.
- Consider using cool compresses to soothe irritated eyes in conjunction with eye drops.
Home Remedies
Some home remedies may offer temporary relief from allergy symptoms. These are not substitutes for medical treatments but can supplement them. The effectiveness varies greatly depending on the individual and the severity of the allergy.
- Saline nasal rinse: This can help clear nasal passages of allergens and irritants, providing some relief from congestion.
- Cool compress: Applying a cool compress to itchy eyes or skin can provide soothing relief.
- Showering: Washing your hair and body after spending time outdoors can remove allergens from your skin.
Emergency Treatments
For severe allergic reactions (anaphylaxis), which can be life-threatening, immediate medical attention is crucial. This requires using an epinephrine auto-injector (EpiPen or similar) followed by immediate transport to a hospital. Delaying treatment in such cases can be extremely dangerous.
- Call emergency services immediately if you experience symptoms such as difficulty breathing, swelling of the face or throat, dizziness, or a rapid heartbeat.
- Administer epinephrine as prescribed by your doctor.
- Seek immediate medical care; do not rely solely on home remedies.
Why are my allergies so bad this year?
Allergy severity can fluctuate significantly from year to year due to a variety of factors. One major contributor is pollen count. Higher pollen counts, driven by factors like warmer temperatures, increased rainfall (in some cases), or even changes in land use leading to more pollen-producing plants, directly translate to more allergen exposure and consequently, worse allergy symptoms. Weather patterns play a huge role; a particularly wet spring followed by a warm, dry period can create a perfect storm for pollen production and dispersal. Additionally, the type of pollen prevalent in your area can influence your symptoms. Some people are more sensitive to certain types of pollen (grass, tree, weed) than others, and the dominant pollen in your region during a given season will dictate how severe your allergies are. Finally, your individual immune system and its response to allergens changes over time, making some years worse than others, even under similar environmental conditions. Underlying health conditions, stress levels, and even medication changes can all contribute to variations in your allergy response.
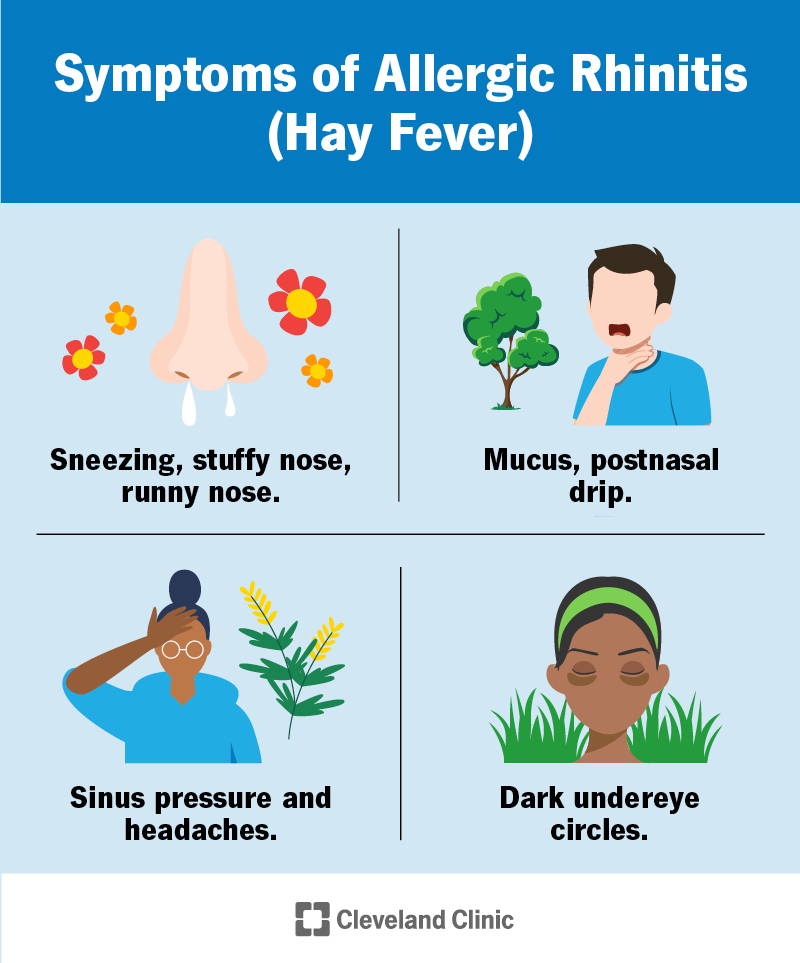
Why are my allergies so bad this time of year?
Seasonal allergies, also known as hay fever, are typically triggered by specific plants releasing pollen during their flowering season. The severity of your symptoms at a particular time of year depends heavily on the dominant pollen in your area during that period. For instance, tree pollen is usually most prevalent in the spring, grass pollen in the summer, and weed pollen in the late summer and fall. If you’re experiencing particularly bad allergies right now, it's likely due to a high concentration of the pollen type currently dominating your local environment. Environmental factors such as wind patterns, temperature, and rainfall also influence pollen dispersal. Strong winds can spread pollen over larger distances, increasing your exposure. The length of the pollen season itself can impact symptom severity; a longer pollen season leads to more extended exposure and potentially more severe symptoms. Furthermore, your individual sensitivity to specific pollen types and overall pollen load determine your personal experience. If you are particularly sensitive to a pollen prevalent in your area at this time, you’ll likely experience a significant worsening of allergy symptoms.
Why are my allergies suddenly so much worse?
A sudden worsening of allergy symptoms can be concerning and often points to specific triggers beyond the usual seasonal variations. One possibility is a new allergen exposure. Perhaps you've moved to a new area with a different pollen profile, started a new hobby that exposes you to allergens (like gardening), or brought a new pet into your home that carries allergens (such as pet dander). Changes in your environment also play a key role. Construction nearby, increased mold growth due to humidity, or the presence of new flowering plants near your home can all lead to a sudden increase in allergen exposure. Underlying health conditions, such as a viral infection weakening your immune system, can also trigger a dramatic increase in allergy symptoms. Furthermore, changes in medication, stress levels, or even hormonal fluctuations can impact your immune response and exacerbate existing allergies. It's crucial to identify the potential trigger to manage your symptoms effectively.
Why are my allergies worse indoors than outdoors?
While you might associate allergies primarily with outdoor pollen, many allergens thrive indoors, making indoor spaces potentially more problematic for some allergy sufferers. Indoor allergens such as dust mites, pet dander, mold, and cockroach droppings are common culprits. Dust mites, microscopic creatures that feed on dead skin cells, are prevalent in carpets, bedding, and upholstered furniture. Pet dander, consisting of tiny skin flakes, can accumulate on surfaces throughout the home. Mold spores thrive in damp environments, such as bathrooms, basements, and areas with leaks. Cockroach droppings contain allergens that can trigger significant reactions. The concentration of these allergens indoors is often higher than outdoors, leading to more intense allergy symptoms for those sensitive to them. Poor ventilation traps these allergens indoors, worsening the problem. Regular cleaning, air filtration, and addressing dampness are crucial steps in reducing indoor allergen levels.
Deja una respuesta