How do you pee after bladder removal
After undergoing a bladder removal surgery, also known as cystectomy, many individuals are left wondering about the significant changes that have occurred in their urinary systems. One of the primary concerns is understanding how to urinate effectively without a bladder. This article will provide a comprehensive guide on the various methods and techniques available for post-cystectomy urination, empowering patients with the knowledge and understanding necessary to navigate this aspect of their recovery journey.
Life After Bladder Removal: Understanding Urinary Diversion
After a cystectomy (bladder removal), you will no longer be able to urinate in the usual way. This is because the bladder, the organ responsible for storing and releasing urine, has been removed. Therefore, a surgical procedure called urinary diversion is necessary to create a new way for urine to exit the body. This involves rerouting the ureters (tubes that carry urine from the kidneys) to a different location, creating a new pathway for urine elimination. The specific type of diversion used depends on various factors, including your overall health, the surgeon's preference, and your individual circumstances. The adjustment to a new urinary system requires careful planning, preparation, and ongoing medical management. It's crucial to understand the process and potential challenges beforehand to facilitate a smoother transition and improve your quality of life.
Types of Urinary Diversion
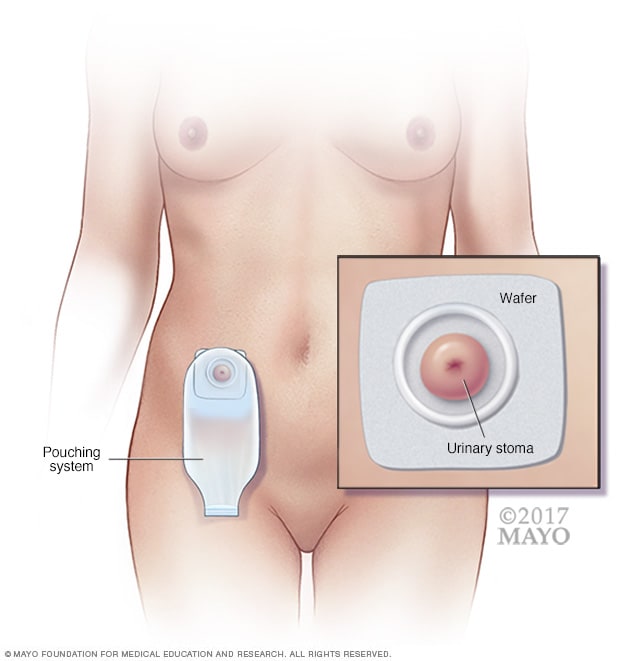
There are several types of urinary diversion procedures, each with its own advantages and disadvantages. These include: ileal conduit (or urostomy), where a section of the ileum (small intestine) is used to create a pouch that collects urine, which then exits the body through a stoma (opening in the abdomen); neobladder (orthotopic neobladder), where a new bladder is constructed from a section of bowel, allowing you to urinate through the urethra as before, although with some differences; and cutaneous ureterostomy, where the ureters are directly connected to the skin, creating a stoma for urine drainage. The choice of diversion is a critical decision made in consultation with your urologist and based on your individual needs and medical history. Careful consideration of the pros and cons of each option is essential before surgery.
Stoma Care and Management
If your urinary diversion involves a stoma (as in an ileal conduit or cutaneous ureterostomy), you'll need to learn how to care for it properly. This involves regularly changing the ostomy appliance (a pouch that collects urine), monitoring the stoma for any signs of infection or irritation, and maintaining good skin hygiene around the stoma site. Your healthcare team will provide detailed instructions and training on stoma care before you leave the hospital and will continue to support you afterward. Regular follow-up appointments are crucial for monitoring your progress and addressing any issues that may arise.
Potential Complications
Like any major surgery, urinary diversion carries the risk of complications. These can include infection, bleeding, leakage from the stoma or surgical site, blockages in the urinary system, and kidney stones. It's essential to be aware of the potential complications and know what to look for. Promptly reporting any concerning symptoms to your healthcare provider is crucial for early intervention and preventing more serious issues. Regular check-ups and blood tests will help monitor kidney function and detect any potential problems early.
Lifestyle Adjustments
Adapting to life after bladder removal and urinary diversion requires significant lifestyle adjustments. This might involve learning new techniques for managing your urinary output, understanding the proper use of ostomy supplies, and making adjustments to your diet and fluid intake. You'll need to pay close attention to your fluid intake to avoid dehydration or overhydration, both of which can lead to complications. Support groups and counseling can be invaluable in navigating these changes and coping with the emotional challenges that may arise.
Long-Term Follow-Up Care
Long-term follow-up care is essential after urinary diversion. This involves regular check-ups with your urologist to monitor your kidney function, assess the health of your stoma (if applicable), and address any complications that may develop. You will likely need regular blood tests and imaging studies to ensure everything is functioning as it should. Maintaining open communication with your healthcare team is key to managing your condition effectively and maintaining a good quality of life. Learning how to self-manage your condition, such as recognizing and addressing potential problems, is an important part of long-term success.
| Type of Diversion | Description | Advantages | Disadvantages |
|---|---|---|---|
| Ileal Conduit | Urine drains into a pouch created from the ileum, exiting through a stoma. | Relatively simple procedure, low risk of incontinence. | Requires ostomy care, risk of infection and stoma complications. |
| Neobladder | A new bladder is created from bowel, allowing urination through the urethra. | More natural way of urination. | Higher risk of incontinence, potential for complications during surgery and recovery. |
| Cutaneous Ureterostomy | Ureters are connected directly to the skin, creating a stoma. | Simple procedure. | Higher risk of kidney damage, requires ostomy care. |
Life After Bladder Removal: Understanding Urinary Diversion
After a cystectomy (bladder removal), you will no longer be able to urinate in the usual way. This is because the bladder, the organ responsible for storing and releasing urine, has been removed. Therefore, a surgical procedure called urinary diversion is necessary to create a new way for urine to exit the body. This involves rerouting the ureters (tubes that carry urine from the kidneys) to a different location, creating a new pathway for urine elimination. The specific type of diversion used depends on various factors, including your overall health, the surgeon's preference, and your individual circumstances. The adjustment to a new urinary system requires careful planning, preparation, and ongoing medical management. It's crucial to understand the process and potential challenges beforehand to facilitate a smoother transition and improve your quality of life.
Types of Urinary Diversion
There are several types of urinary diversion procedures, each with its own advantages and disadvantages. These include: ileal conduit (or urostomy), where a section of the ileum (small intestine) is used to create a pouch that collects urine, which then exits the body through a stoma (opening in the abdomen); neobladder (orthotopic neobladder), where a new bladder is constructed from a section of bowel, allowing you to urinate through the urethra as before, although with some differences; and cutaneous ureterostomy, where the ureters are directly connected to the skin, creating a stoma for urine drainage. The choice of diversion is a critical decision made in consultation with your urologist and based on your individual needs and medical history. Careful consideration of the pros and cons of each option is essential before surgery.
Stoma Care and Management
If your urinary diversion involves a stoma (as in an ileal conduit or cutaneous ureterostomy), you'll need to learn how to care for it properly. This involves regularly changing the ostomy appliance (a pouch that collects urine), monitoring the stoma for any signs of infection or irritation, and maintaining good skin hygiene around the stoma site. Your healthcare team will provide detailed instructions and training on stoma care before you leave the hospital and will continue to support you afterward. Regular follow-up appointments are crucial for monitoring your progress and addressing any issues that may arise.
Potential Complications
Like any major surgery, urinary diversion carries the risk of complications. These can include infection, bleeding, leakage from the stoma or surgical site, blockages in the urinary system, and kidney stones. It's essential to be aware of the potential complications and know what to look for. Promptly reporting any concerning symptoms to your healthcare provider is crucial for early intervention and preventing more serious issues. Regular check-ups and blood tests will help monitor kidney function and detect any potential problems early.
Lifestyle Adjustments
Adapting to life after bladder removal and urinary diversion requires significant lifestyle adjustments. This might involve learning new techniques for managing your urinary output, understanding the proper use of ostomy supplies, and making adjustments to your diet and fluid intake. You'll need to pay close attention to your fluid intake to avoid dehydration or overhydration, both of which can lead to complications. Support groups and counseling can be invaluable in navigating these changes and coping with the emotional challenges that may arise.
Long-Term Follow-Up Care
Long-term follow-up care is essential after urinary diversion. This involves regular check-ups with your urologist to monitor your kidney function, assess the health of your stoma (if applicable), and address any complications that may develop. You will likely need regular blood tests and imaging studies to ensure everything is functioning as it should. Maintaining open communication with your healthcare team is key to managing your condition effectively and maintaining a good quality of life. Learning how to self-manage your condition, such as recognizing and addressing potential problems, is an important part of long-term success.
| Type of Diversion | Description | Advantages | Disadvantages |
|---|---|---|---|
| Ileal Conduit | Urine drains into a pouch created from the ileum, exiting through a stoma. | Relatively simple procedure, low risk of incontinence. | Requires ostomy care, risk of infection and stoma complications. |
| Neobladder | A new bladder is created from bowel, allowing urination through the urethra. | More natural way of urination. | Higher risk of incontinence, potential for complications during surgery and recovery. |
| Cutaneous Ureterostomy | Ureters are connected directly to the skin, creating a stoma. | Simple procedure. | Higher risk of kidney damage, requires ostomy care. |
What happens to my bladder when it's removed?
When your bladder is removed, a surgical procedure called a cystectomy, it's completely taken out of your body. This is typically done to treat bladder cancer, but may also be necessary for other conditions. The surgery itself can vary depending on the extent of the cancer and the surgeon's approach. Sometimes, only part of the bladder is removed (partial cystectomy), while other times, the entire bladder is removed (radical cystectomy). Following a radical cystectomy, surgeons will need to create a new way for urine to leave your body. This is where urinary diversion comes in.
What is urinary diversion, and what are my options?
Urinary diversion is a surgical procedure that creates a new way for urine to leave your body after bladder removal. There are several different types of urinary diversions, each with its own advantages and disadvantages. Ileal conduit is a common option where a portion of the small intestine is used to create a channel (stoma) that brings urine to a bag worn on the outside of the body. This bag needs to be emptied regularly. Another option is a neobladder, where a section of the intestine is surgically fashioned into a new bladder. This allows you to urinate in a more natural way, although you may experience some incontinence. A third option is a continent cutaneous diversion, where a pouch is created from the intestine and connected to the skin. This allows you to catheterize yourself regularly to empty the pouch. The best option for you will depend on several factors, including your overall health, the extent of the surgery, and your personal preferences. Your surgeon will discuss these options with you in detail before surgery.
How will I empty my bladder after surgery, regardless of the diversion method?
The method of emptying your bladder after a cystectomy depends entirely on the type of urinary diversion performed. With an ileal conduit, you will wear a drainage bag attached to the stoma on your abdomen. This bag needs to be emptied regularly, typically several times a day. You'll also need to change the bag regularly to maintain hygiene and prevent infections. If you have a neobladder, you will urinate through your urethra as you did before, although you may need to catheterize yourself periodically to fully empty your neobladder. With a continent cutaneous diversion, you will need to regularly catheterize yourself to empty the internal pouch through a stoma. Your healthcare team will thoroughly train you on the proper techniques for emptying your urinary diversion, caring for your stoma, and managing any potential complications.
What are the potential complications after bladder removal?
As with any major surgery, there are potential complications associated with bladder removal and urinary diversion. These can include infection at the surgical site or in the urinary tract, bleeding, blood clots, leakage from the diversion, obstruction of the urinary tract, and kidney problems. Additionally, you may experience skin irritation around the stoma (if applicable), incontinence (depending on the type of diversion), or psychological adjustment to the changes in your body and lifestyle. Regular follow-up appointments with your surgeon and healthcare team are crucial for monitoring your progress, addressing any complications, and ensuring optimal management of your urinary diversion. Open communication with your healthcare provider about any concerns or symptoms is essential for maintaining your health and well-being.
Deja una respuesta