What is life expectancy after bladder removal
Bladder removal is a major surgical procedure that can significantly impact a person's life expectancy. This article explores the factors that influence life expectancy after bladder removal, including the type of surgery performed, the patient's overall health, and the availability of post-operative care.
Life Expectancy Following Cystectomy: A Comprehensive Overview
Life expectancy after bladder removal (cystectomy) is a complex issue, and it's impossible to give a single definitive answer. Several factors significantly influence a patient's prognosis following this major surgery. While the surgery itself carries risks, the impact on life expectancy is primarily determined by the underlying reason for the cystectomy – typically bladder cancer – and the patient's overall health.
Factors Affecting Life Expectancy Post-Cystectomy
Several factors influence life expectancy after a cystectomy. The most crucial is the stage and grade of the bladder cancer at the time of surgery. Early-stage cancers have a much better prognosis than advanced cancers that have spread to other organs (metastasis). Other significant factors include the patient's age, overall health, presence of other medical conditions (such as heart disease or diabetes), and their response to treatment, including chemotherapy and radiation therapy.
Impact of Cancer Stage on Survival Rates
The stage of the bladder cancer at the time of diagnosis is the most powerful predictor of survival. Stage 0 cancers, which are non-invasive, have an excellent prognosis. Conversely, Stage IV cancers, which have metastasized, have a much lower survival rate. Survival statistics vary widely depending on the staging system used and the specific characteristics of the cancer, so it is crucial to discuss prognosis with the medical team.
Surgical Techniques and Outcomes
The type of cystectomy performed also plays a role. A radical cystectomy, which involves removing the bladder and surrounding lymph nodes, is the most common procedure for bladder cancer. Partial cystectomies, where only part of the bladder is removed, are done for less advanced cancers. The surgical approach (open surgery versus minimally invasive techniques like robotic-assisted surgery) can impact recovery time and potential complications, but it's not typically the primary determinant of long-term survival.
Post-Operative Complications and their Effect
Post-operative complications can significantly affect life expectancy. These complications may include infection, bleeding, blood clots, urinary tract complications (such as urinary leakage or strictures), and bowel dysfunction. The severity and management of these complications impact the patient's recovery and overall health, which in turn affect their long-term survival prospects. Effective post-operative care is essential to minimize these risks.
Treatment Following Cystectomy and its Influence
Adjuvant therapies such as chemotherapy and radiation are often used after cystectomy, especially in patients with more advanced cancers or a high risk of recurrence. These treatments can improve survival rates and reduce the chances of the cancer returning. The effectiveness of these therapies depends on several factors, including the patient's individual characteristics and the type of cancer. Close monitoring following surgery is essential to detect and treat any recurrence as early as possible.
| Factor | Impact on Life Expectancy |
|---|---|
| Cancer Stage | Significantly impacts survival rates; early stages have much better prognoses. |
| Patient Age and Overall Health | Older age and pre-existing conditions can influence recovery and survival. |
| Surgical Technique | Minimally invasive techniques may improve recovery time but don't drastically alter long-term survival. |
| Adjuvant Therapy (Chemotherapy/Radiation) | Can significantly improve survival rates in certain cases. |
| Post-Operative Complications | Can negatively affect recovery and long-term survival. |
Life Expectancy Following Cystectomy: A Comprehensive Overview
Life expectancy after bladder removal (cystectomy) is a complex issue, and it's impossible to give a single definitive answer. Several factors significantly influence a patient's prognosis following this major surgery. While the surgery itself carries risks, the impact on life expectancy is primarily determined by the underlying reason for the cystectomy – typically bladder cancer – and the patient's overall health.
Factors Affecting Life Expectancy Post-Cystectomy
Several factors influence life expectancy after a cystectomy. The most crucial is the stage and grade of the bladder cancer at the time of surgery. Early-stage cancers have a much better prognosis than advanced cancers that have spread to other organs (metastasis). Other significant factors include the patient's age, overall health, presence of other medical conditions (such as heart disease or diabetes), and their response to treatment, including chemotherapy and radiation therapy.
Impact of Cancer Stage on Survival Rates
The stage of the bladder cancer at the time of diagnosis is the most powerful predictor of survival. Stage 0 cancers, which are non-invasive, have an excellent prognosis. Conversely, Stage IV cancers, which have metastasized, have a much lower survival rate. Survival statistics vary widely depending on the staging system used and the specific characteristics of the cancer, so it is crucial to discuss prognosis with the medical team.
Surgical Techniques and Outcomes
The type of cystectomy performed also plays a role. A radical cystectomy, which involves removing the bladder and surrounding lymph nodes, is the most common procedure for bladder cancer. Partial cystectomies, where only part of the bladder is removed, are done for less advanced cancers. The surgical approach (open surgery versus minimally invasive techniques like robotic-assisted surgery) can impact recovery time and potential complications, but it's not typically the primary determinant of long-term survival.
Post-Operative Complications and their Effect
Post-operative complications can significantly affect life expectancy. These complications may include infection, bleeding, blood clots, urinary tract complications (such as urinary leakage or strictures), and bowel dysfunction. The severity and management of these complications impact the patient's recovery and overall health, which in turn affect their long-term survival prospects. Effective post-operative care is essential to minimize these risks.
Treatment Following Cystectomy and its Influence
Adjuvant therapies such as chemotherapy and radiation are often used after cystectomy, especially in patients with more advanced cancers or a high risk of recurrence. These treatments can improve survival rates and reduce the chances of the cancer returning. The effectiveness of these therapies depends on several factors, including the patient's individual characteristics and the type of cancer. Close monitoring following surgery is essential to detect and treat any recurrence as early as possible.
| Factor | Impact on Life Expectancy |
|---|---|
| Cancer Stage | Significantly impacts survival rates; early stages have much better prognoses. |
| Patient Age and Overall Health | Older age and pre-existing conditions can influence recovery and survival. |
| Surgical Technique | Minimally invasive techniques may improve recovery time but don't drastically alter long-term survival. |
| Adjuvant Therapy (Chemotherapy/Radiation) | Can significantly improve survival rates in certain cases. |
| Post-Operative Complications | Can negatively affect recovery and long-term survival. |
What is the average life expectancy after a cystectomy?
Life expectancy after a cystectomy, or bladder removal surgery, is highly variable and depends on several crucial factors. While the surgery itself doesn't inherently shorten lifespan, the underlying reason for the cystectomy—typically bladder cancer—is the primary determinant of long-term prognosis. The stage of the cancer at the time of diagnosis is paramount; early-stage bladder cancer treated with a cystectomy offers significantly better survival rates compared to advanced-stage disease. Other factors impacting life expectancy include the patient's overall health, the presence of other comorbidities (like heart disease or diabetes), the effectiveness of the surgery in removing all cancerous tissue, and the subsequent need for adjuvant therapies such as chemotherapy or radiation. Studies show that patients undergoing cystectomy for muscle-invasive bladder cancer have a significantly lower 5-year survival rate than the general population. However, advancements in surgical techniques, chemotherapy regimens, and immunotherapy have improved outcomes in recent years. Furthermore, post-operative complications, such as infections or issues related to urinary diversion, can also affect long-term survival. Therefore, it's impossible to give a single definitive answer to the question of life expectancy after a cystectomy. Each patient's case is unique, and their prognosis should be discussed with their oncology team who can provide a personalized assessment based on their individual circumstances.
How does the type of urinary diversion affect life expectancy?
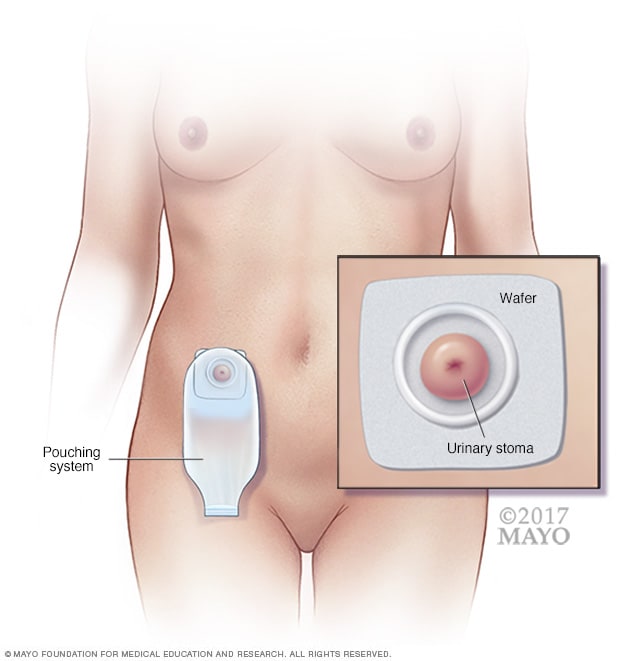
The type of urinary diversion used following a cystectomy can indirectly influence a patient's quality of life and, consequently, might have a subtle impact on their overall lifespan. While the diversion itself doesn't directly shorten lifespan, complications associated with the diversion can affect overall health. Ileal conduit, for instance, carries a risk of infections, stones, and other complications that, if severe or recurrent, could potentially impact longevity. Similarly, other diversions, such as neobladder or continent diversions, carry their own set of potential complications, although they often offer better quality of life. Complications from any diversion can lead to hospitalizations, infections, and decreased functionality, potentially impacting overall well-being. However, the impact on life expectancy is often indirect and overshadowed by the underlying cancer and its treatment. A well-functioning diversion, coupled with proper post-operative care and management, generally allows patients to maintain a relatively normal lifestyle. Therefore, the type of urinary diversion is more strongly linked to quality of life post-surgery than to a direct reduction in life expectancy. The focus should remain on minimizing complications through diligent post-operative care and regular monitoring.
What are the most significant factors impacting survival rates after bladder removal?
Several crucial factors heavily influence survival rates after bladder removal surgery. Stage of cancer at diagnosis is undoubtedly the most significant factor. Early-stage bladder cancers diagnosed and treated early often result in much higher survival rates compared to advanced-stage cancers that have metastasized. The presence of lymph node involvement at the time of surgery is another important predictor of prognosis. If cancer cells have spread to nearby lymph nodes, the chances of recurrence and poorer survival are higher. The patient's overall health and the presence of other medical conditions (comorbidities) also play a significant role. Patients with pre-existing conditions like heart disease, diabetes, or lung disease may have a reduced ability to tolerate the rigors of surgery and subsequent treatments. The surgical margins are crucial; if cancer cells remain at the edges of the resected tissue, the risk of recurrence increases, thus lowering survival rates. Finally, the effectiveness and response to adjuvant therapies, such as chemotherapy or immunotherapy, significantly impact survival. Patients who respond well to post-surgical treatments have a much better prognosis than those who do not. Therefore, a comprehensive evaluation of all these factors is crucial in accurately assessing individual survival prospects after cystectomy.
Can I expect a normal life after bladder removal surgery?
While a "normal" life after bladder removal surgery is subjective, many patients can lead fulfilling and active lives. The surgery itself doesn't automatically mean a drastically reduced lifespan, but it does involve significant adjustments. The type of urinary diversion significantly impacts daily routines. An ileal conduit, for instance, requires the use of a stoma bag, which can be initially challenging to adapt to. However, with proper training and support, most patients learn to manage their diversion efficiently. Neobladders, on the other hand, offer a more natural urinary experience, although potential complications such as incontinence or reflux can arise. Beyond the urinary system, the impact of the underlying cancer and its treatment must also be considered. Chemotherapy and radiation can lead to fatigue, nausea, and other side effects that temporarily affect daily life. However, many patients regain their strength and energy over time. A supportive medical team, including surgeons, urologists, oncologists, and stoma nurses, is crucial for addressing any physical or emotional challenges. Regular follow-up appointments, including imaging and blood tests, are vital to monitor for cancer recurrence. Therefore, while life after a cystectomy may differ from life before the surgery, with proper management and a positive attitude, many patients successfully adjust and enjoy high quality of life.
Deja una respuesta