What happens 2 weeks prior to death
In the twilight of life, as the mortal journey nears its end, a profound transformation unfolds within the human body. The final fortnight before death witnesses a cascade of subtle and remarkable changes, both physical and emotional, as the body prepares to embark upon its final transition. From altered breathing patterns to increased sensitivity and profound introspection, these pre-death phenomena offer a window into the intricate workings of our biology and the mysteries of the dying process.
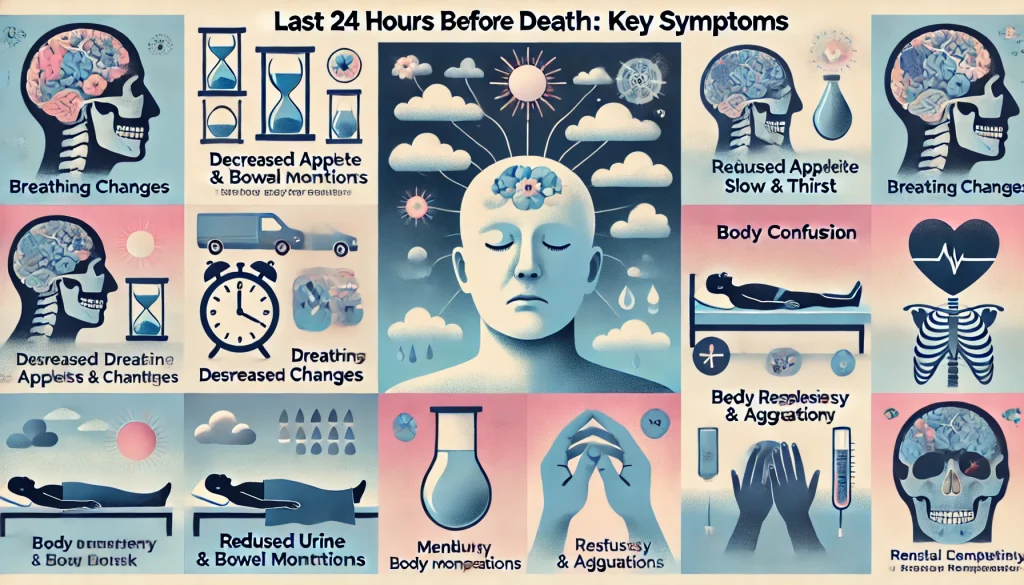
What Happens in the Two Weeks Before Death?
The two weeks leading up to death are highly variable and depend on numerous factors, including the underlying cause of death, the individual's overall health, and their age. There isn't a single, universally applicable timeline. However, some common signs and symptoms may appear during this period. It's crucial to remember that not everyone experiences all of these, and the severity and presence of these symptoms vary greatly. It's vital to consult with medical professionals for accurate assessment and personalized care.
Changes in Physical Function
In the final two weeks of life, a gradual decline in physical function is common. This can manifest as increasing weakness and fatigue. Individuals may struggle with simple tasks that were previously easy, such as walking, eating, or dressing themselves. Loss of appetite is also frequent, leading to reduced food and fluid intake. Changes in bowel and bladder control, such as incontinence, may also occur. The body's ability to regulate temperature might decrease, leading to increased sensitivity to cold. Finally, sleep patterns can become erratic, with periods of increased drowsiness interspersed with restlessness.
Cognitive and Mental Changes
Alongside physical decline, cognitive and mental changes are possible. Confusion and disorientation can occur, making it difficult for the individual to recognize loved ones or understand their surroundings. Short-term memory loss may worsen, and the individual might become more withdrawn or less responsive. Periods of agitation or restlessness are also possible, even alongside periods of lethargy. It's important to maintain a calm and reassuring environment during these times.
Respiratory Changes
Respiratory changes are a common sign in the final stages of life. Breathing may become labored and shallow, with periods of apnea (temporary cessation of breathing) becoming more frequent. Rales (wet, crackling sounds in the lungs) may be audible. The individual may experience shortness of breath, even while at rest. Oxygen levels may fluctuate, requiring supplemental oxygen in some cases. These respiratory changes reflect the body's gradual shutdown.
Circulatory Changes
As the body nears the end of life, circulatory changes become evident. Blood pressure may drop, leading to a weakened pulse and decreased circulation to the extremities. The extremities may appear pale, cool, and mottled. Peripheral pulses may become weak or difficult to palpate. These changes reflect the body's decreasing ability to pump blood effectively.
Pain Management
Pain management is paramount during the final weeks of life. Medical professionals can provide effective pain relief measures, such as medication, to ensure the individual's comfort. It's crucial to discuss pain management options with the healthcare team to find the most appropriate approach for the individual's specific needs. Open communication about pain levels and response to medication is essential.
| Symptom | Description | Management |
|---|---|---|
| Weakness and Fatigue | Decreased energy and strength | Rest, supportive care |
| Loss of Appetite | Reduced desire to eat or drink | Small, frequent meals; hydration support |
| Confusion and Disorientation | Difficulty with awareness and orientation | Calm environment, reassurance |
| Shortness of Breath | Difficulty breathing | Oxygen therapy, comfort measures |
| Pain | Physical discomfort | Medication, pain management strategies |
What are the common physical changes two weeks before death?
Two weeks before death, a wide range of physical changes can occur, varying greatly depending on the underlying illness and individual circumstances. Weakness and fatigue are often prominent, with the individual experiencing a significant decrease in energy levels and a need for increased rest. Loss of appetite and difficulty eating are also common, sometimes leading to weight loss. Changes in sleep patterns are frequently observed, with some individuals sleeping excessively while others experience insomnia. Changes in bowel and bladder function can occur, including incontinence or constipation. Breathing may become labored or irregular, with periods of shallow breathing interspersed with deeper breaths (Cheyne-Stokes respiration). Skin changes are also possible, such as pallor, coolness to the touch, and mottling (discoloration of the skin). Decreased mental clarity, confusion, or delirium can occur due to a variety of factors, including medication side effects, dehydration, and underlying organ dysfunction. It's crucial to remember that not everyone will experience all these changes, and the severity and presence of these signs will vary significantly between individuals.
What about cognitive and emotional changes in the two weeks before death?
In the two weeks preceding death, cognitive and emotional changes are quite common and can be significantly impactful for both the dying person and their loved ones. Confusion and disorientation are frequently observed, potentially stemming from medication side effects, dehydration, or underlying medical conditions affecting brain function. Memory loss, particularly short-term memory, can also occur. Personality changes are possible, with some individuals becoming withdrawn and less responsive, while others exhibit increased agitation or restlessness. Emotional fluctuations are also common, ranging from periods of calmness and acceptance to intense anxiety, fear, or depression. These emotional changes are often linked to the complex experience of facing mortality and the uncertainty surrounding the future. Difficulty communicating may arise due to weakness, altered consciousness, or changes in cognitive function. It's crucial to approach these changes with patience and compassion, providing reassurance and support to the dying individual and their family. Professional palliative care can be invaluable in managing these cognitive and emotional challenges and ensuring the dying person's comfort and dignity.
How can I tell if someone is nearing the end of their life within this timeframe?
Determining when someone is nearing the end of life within two weeks can be challenging, as the process is highly individual. However, several indicators can suggest that death is approaching. A significant decline in overall physical functioning, marked by increasing weakness, inability to perform basic self-care tasks, and profound fatigue, is often a key sign. Changes in vital signs, such as a decrease in blood pressure, heart rate, and body temperature, can also indicate impending death. Decreased responsiveness and prolonged periods of unconsciousness are further potential indicators. Changes in breathing patterns, including Cheyne-Stokes respiration (alternating periods of deep and shallow breathing) or increasingly shallow and irregular breathing (agonal breathing), are strong predictors of imminent death. Withdrawal from social interaction and a decreased interest in surroundings can also suggest the individual is nearing the end of life. It’s crucial to note that these signs may not be present in every individual, and the progression can be unpredictable. Consulting with a healthcare professional is essential for accurate assessment and guidance.
What support is available for families during this time?
The two weeks leading up to death are an incredibly challenging time for families. Emotional support is paramount, and several resources are available to help families navigate this difficult period. Hospice care provides comprehensive support for the dying person and their loved ones, focusing on pain management, emotional support, and spiritual care. Palliative care teams offer medical, nursing, and social work support to improve the quality of life for individuals facing serious illness. Grief counseling and support groups can provide a safe space to process emotions and connect with others who have experienced similar losses. Spiritual advisors can offer comfort and guidance during this spiritually significant time. Family and friends can play a vital role in providing emotional support, practical assistance, and companionship. Online resources and books offering guidance on end-of-life care can also be helpful. It’s important for families to seek out the support that best meets their needs, remembering that accepting help is a sign of strength, not weakness, during this difficult time. Open communication within the family and with healthcare professionals is crucial to ensure the dying person’s comfort and the family’s well-being.
Deja una respuesta