How do you know if your body is full of infection

Are you experiencing unexplained fatigue, persistent fever, or random body aches? Do open wounds take forever to heal? You might have an infection lurking in your body, even if you don't have any visible symptoms. Infections occur when harmful microorganisms, such as bacteria or viruses, invade your tissues and cause a reaction in your immune system. While some infections are mild and go away on their own, others can be severe and require medical treatment. To maintain good health, it's essential to be aware of the signs and symptoms that indicate a potential infection in your body.
Recognizing the Signs of a Systemic Infection
Knowing when your body is fighting a widespread infection, also known as a systemic infection, is crucial for timely medical intervention. A systemic infection isn't just a localized issue like a cut getting infected; it's when the infection has spread throughout your bloodstream, affecting multiple organs or systems. This can be life-threatening, so understanding the signs is vital. These signs often go beyond the typical symptoms of a localized infection and are typically more severe and widespread. Early recognition and prompt medical attention are essential for successful treatment.
High Fever and Chills
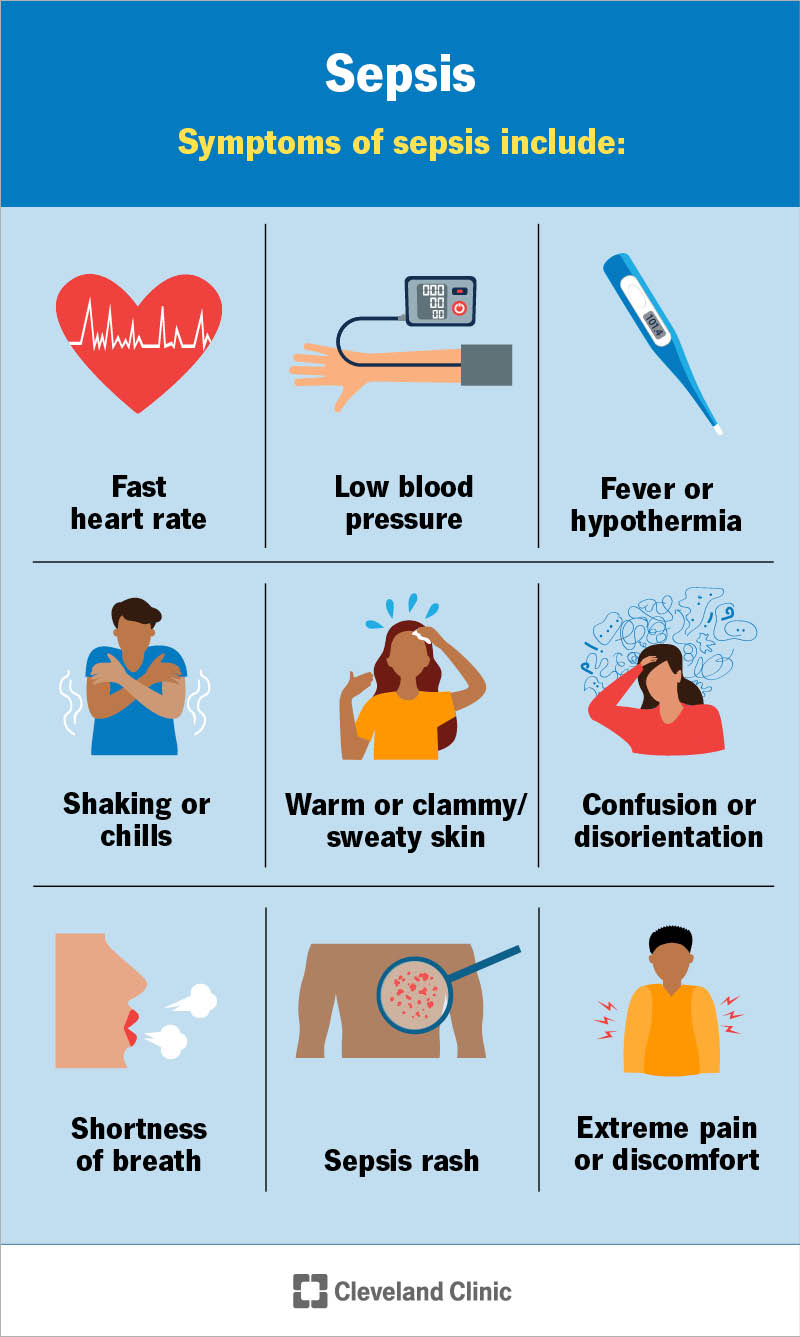
A high fever (generally above 101°F or 38.3°C) is a classic sign of a systemic infection. Your body is essentially ramping up its immune response to fight the invading pathogens. Accompanying this fever, you might experience intense chills, even while sweating. The chills are a result of your body trying to raise its temperature to fight the infection. This combination of fever and chills, especially if persistent and high, warrants immediate medical attention.
Rapid Heart Rate and Breathing
Your heart rate (tachycardia) and breathing rate (tachypnea) can increase significantly as your body works overtime to combat the infection. This is because your body needs to deliver more oxygen and nutrients to fight the infection and remove waste products. A rapid pulse and shortness of breath, even at rest, could indicate a serious infection.
Fatigue and Weakness
Feeling extremely tired and weak is another common indicator. The body's resources are being diverted to fight the infection, leaving you with limited energy for other bodily functions. This fatigue is often far more pronounced than the tiredness you might experience with a common cold or flu. It's a sign that your immune system is struggling to keep up.
Changes in Mental State
A systemic infection can affect brain function, leading to changes in mental state. This might include confusion, disorientation, lethargy, or even delirium. These changes are often indicative of sepsis, a life-threatening complication of infection, and require immediate medical attention. Don't ignore sudden or unusual changes in mental clarity.
Skin Changes
While not always present, changes in skin appearance can signal a systemic infection. This might include a rash, unusual paleness or discoloration, or even small purplish spots (petechiae), which indicate bleeding under the skin. These skin changes can be an indication of the infection's spread throughout the circulatory system.
| Symptom | Description | Severity |
|---|---|---|
| High Fever | Temperature above 101°F (38.3°C) | Severe - warrants immediate medical attention |
| Chills | Intense shivering, even while sweating | Moderate to Severe - depends on intensity and duration |
| Rapid Heart Rate | Heart beating faster than normal | Moderate to Severe - depends on resting heart rate and other symptoms |
| Rapid Breathing | Breathing faster and shallower than normal | Moderate to Severe - depends on resting breathing rate and other symptoms |
| Extreme Fatigue | Overwhelming tiredness and weakness | Moderate to Severe - depends on the inability to perform daily activities |
| Mental Confusion | Disorientation, lethargy, or delirium | Severe - requires immediate medical assistance |
| Skin Changes | Rash, paleness, or petechiae | Moderate to Severe - depends on the extent and type of skin changes |
What are the symptoms of high infection in the body?
:max_bytes(150000):strip_icc()/infection-symptoms-5185799-Final-7a28a6cc8d3143928418bc83bc7071bd.jpg)
The symptoms of a high infection, also known as sepsis, vary depending on the type and severity of the infection, as well as the individual's overall health. However, some common signs indicate a severe infection and should prompt immediate medical attention. These symptoms can range from mild to life-threatening and can develop quickly. It's crucial to understand that this information is for general knowledge and should not replace professional medical advice. Always seek immediate medical help if you suspect a serious infection.
Fever and Chills
A high fever is a common sign of infection, often accompanied by chills or shivering. This occurs because the body is trying to fight off the infection. The fever's intensity can vary. A high fever, over 103°F (39.4°C) or persistent high fever, is a significant cause for concern. Chills are often experienced even when the body temperature is actually elevated. A high, persistent fever coupled with chills warrants immediate medical attention.
- Temperature significantly above 100.4°F (38°C)
- Feeling cold and shivering, even when your body temperature is high
- Sweating and feeling hot, followed by chills
Rapid Heart Rate and Breathing
Your body works harder during an infection, leading to an increased heart rate (tachycardia) and breathing rate (tachypnea). This is the body's attempt to deliver more oxygen to combat the infection. A rapid heart rate that persists even at rest, combined with rapid breathing, is a serious warning sign. It indicates that the body is struggling to cope with the infection's effects.
- Heart rate significantly above normal resting rate
- Rapid, shallow breathing or shortness of breath
- Feeling breathless or gasping for air
Changes in Mental State
Severe infections can affect brain function. Symptoms might include confusion, disorientation, difficulty concentrating, or even a loss of consciousness. These changes in mental state are particularly alarming and indicate the infection might be overwhelming the body's systems. They can also be subtle initially, such as difficulty concentrating or feeling unusually confused.
- Confusion or disorientation
- Difficulty concentrating or remembering things
- Loss of consciousness or delirium
Low Blood Pressure (Hypotension)
In severe infections, blood pressure can drop dangerously low due to the body's inability to maintain adequate blood flow. This is known as septic shock, a life-threatening complication of sepsis. Low blood pressure, often coupled with other symptoms like rapid heart rate and shallow breathing, is an emergency situation requiring immediate hospitalization.
- Feeling dizzy or lightheaded
- Fainting or near fainting
- Rapid, weak pulse
Pain, Redness, Swelling, and Warmth at the Infection Site
Localized infections, such as skin infections or pneumonia, will present with symptoms at the infection site. These symptoms can manifest as pain, redness, swelling, and warmth in the affected area. While these symptoms are usually seen in localized infections, their severity or spread can point to a wider systemic infection.
- Pain, tenderness, or throbbing at the infection site
- Redness, warmth, or swelling around the infection
- Pus or other drainage from the infected area
How can I tell if I have an infection in my body?
:max_bytes(150000):strip_icc()/what-is-a-bacterial-infection-7705652_final-2f1b8b2429b2495c8333b584512d3afa.jpg)
How Can I Tell If I Have an Infection in My Body?
Determining if you have an infection requires considering a range of symptoms and factors. Infections can manifest in diverse ways depending on the type of pathogen (bacteria, virus, fungus, parasite) and the location of the infection within your body. No single symptom definitively indicates an infection, and some infections may be asymptomatic. It's crucial to consult a healthcare professional for diagnosis and treatment, as self-treating can be harmful.
Common Symptoms of Infection
Many infections share common symptoms, although their severity varies greatly. These symptoms often indicate your body's immune system is fighting off an invader. However, the absence of these symptoms doesn't guarantee the absence of infection. Always seek medical advice for diagnosis.
- Fever or chills: Your body's temperature rises as a defense mechanism against infection.
- Fatigue and weakness: Your body is working hard to combat the infection, leading to tiredness.
- Pain or soreness: Inflammation at the infection site causes pain.
- Swelling: Fluid accumulation at the infection site due to inflammation.
- Redness: Increased blood flow to the infected area.
Location-Specific Symptoms
Infections manifest differently depending on their location in the body. Identifying the specific area affected is crucial for accurate diagnosis. Understanding location-specific symptoms is vital for seeking appropriate medical attention. For example, a lung infection might present as a cough and shortness of breath, while a urinary tract infection might present with burning during urination.
- Respiratory Infections: Cough, shortness of breath, chest pain, sore throat.
- Urinary Tract Infections (UTIs): Painful urination, frequent urination, cloudy urine.
- Skin Infections: Redness, swelling, pus, warmth to the touch.
- Gastrointestinal Infections: Diarrhea, vomiting, nausea, abdominal cramps.
Severity of Symptoms
The severity of symptoms can be an indicator of the infection's seriousness. While a mild infection might cause only minor discomfort, a severe infection can lead to life-threatening complications. Severe infections require immediate medical attention.
- Mild infections: May only cause mild discomfort, such as a slight cough or headache.
- Moderate infections: Can cause more significant symptoms, such as high fever, severe fatigue, or persistent pain.
- Severe infections: Can lead to life-threatening complications, such as sepsis or organ failure.
Risk Factors and Underlying Conditions
Certain individuals have a higher risk of developing infections due to weakened immune systems or other underlying health conditions. Individuals with compromised immune systems should seek medical attention promptly for even seemingly minor symptoms.
- Weakened immune system: Conditions like HIV/AIDS, cancer, or autoimmune diseases.
- Chronic illnesses: Diabetes, kidney disease, or heart disease.
- Recent surgeries or injuries: Increased risk of infection at the surgical site or injury location.
- Exposure to infectious agents: Contact with infected individuals or contaminated environments.
When to Seek Medical Attention
It is always best to err on the side of caution and seek medical attention if you suspect an infection. Delaying treatment can lead to serious complications. Certain situations warrant immediate medical attention.
- High fever (over 103°F or 39.4°C).
- Severe pain or discomfort.
- Difficulty breathing.
- Signs of dehydration.
- Confusion or disorientation.
How do you treat a full body infection?
Treating a full body infection, also known as sepsis or systemic infection, is a serious medical emergency requiring immediate and aggressive intervention. It's not something that can be effectively addressed with home remedies. The treatment depends entirely on the type of infecting organism (bacteria, virus, fungus, parasite) and the severity of the infection. Diagnosis involves blood tests to identify the pathogen, along with imaging tests like X-rays or CT scans to assess the extent of organ damage. Treatment typically involves a combination of approaches, focusing on eliminating the infection and supporting the body's functions.
Identifying the Source of Infection
Before treatment can begin, accurate identification of the infectious agent is crucial. This often involves blood cultures to identify the bacteria, viruses, or fungi causing the infection. Other diagnostic tests such as urine cultures, sputum cultures, or cerebrospinal fluid analysis may be needed depending on the suspected site of infection. Once identified, the appropriate antibiotic, antiviral, or antifungal medication can be administered.
- Blood cultures: Identifying the specific bacteria or fungi in the bloodstream.
- Urine cultures: Checking for urinary tract infections (UTIs) which can become systemic.
- Imaging techniques (X-rays, CT scans, ultrasounds): Locating the infection’s source within the body.
Antibiotic Therapy
Antibiotics are the cornerstone of treating bacterial infections causing sepsis. The choice of antibiotic depends on the identified pathogen and its susceptibility to various drugs. Broad-spectrum antibiotics may be initially used if the causative organism is unknown, followed by a narrower-spectrum antibiotic once the pathogen is identified and its sensitivities are determined through antibiotic susceptibility testing. Intravenous (IV) administration is usually preferred for severe infections to ensure rapid and effective delivery of the medication.
- Broad-spectrum antibiotics: Used initially to cover a wide range of potential pathogens.
- Narrow-spectrum antibiotics: Used once the infecting organism is identified, targeting it specifically.
- Intravenous administration: Ensures rapid and efficient drug delivery, especially crucial in severe cases.
Supportive Care
In addition to directly combating the infection, supportive care is essential. This focuses on maintaining vital organ functions. This might include fluid resuscitation to address dehydration, oxygen therapy to improve oxygen levels, and mechanical ventilation if breathing is compromised. Monitoring vital signs, blood pressure, and organ function is crucial to ensure the effectiveness of treatment and identify any complications. Nutritional support might also be needed to aid the body's recovery.
- Fluid resuscitation: Correcting dehydration and improving blood circulation.
- Oxygen therapy: Supporting adequate oxygenation of tissues and organs.
- Mechanical ventilation: Assisting with breathing if respiratory failure occurs.
Antifungal and Antiviral Medications
If the full body infection is caused by a fungus (such as Candida) or a virus, then antifungal or antiviral medications are necessary. These medications work differently than antibiotics and target specific fungal or viral components. The specific choice of medication depends on the type of organism involved and its resistance profile. These are often administered intravenously in severe cases.
- Antifungal medications: Targeting fungal infections like candidiasis.
- Antiviral medications: Addressing viral infections causing sepsis.
- Intravenous administration: Ensuring rapid and effective delivery of medication.
Surgical Intervention
In some cases, surgical intervention may be necessary to drain abscesses, remove infected tissues, or repair damaged organs. This is particularly important if a localized infection is the source of the systemic infection. Surgery aims to remove the source of the infection and improve the chances of successful antibiotic therapy. The decision to perform surgery is made on a case-by-case basis, considering the severity of the infection and the overall condition of the patient.
- Drainage of abscesses: Removing pus and infected material.
- Debridement of infected tissue: Removing dead or damaged tissue.
- Surgical repair: Addressing damage to organs caused by the infection.
What happens if an infection stays in your body?
If an infection stays in your body, the consequences depend on several factors, including the type of infection, the location of the infection, the strength of your immune system, and whether or not you seek medical treatment. A persistent infection can lead to a wide range of problems, from relatively mild discomfort to severe, life-threatening complications. The body's initial response to an infection involves inflammation, which, while necessary to fight off the invader, can also cause damage to surrounding tissues if prolonged. The infection itself may directly damage tissues and organs through the release of toxins or by physically disrupting normal cellular function. Untreated or inadequately treated infections can spread to other parts of the body, leading to systemic infection (sepsis), a potentially fatal condition. Chronic infections can also weaken the immune system, making a person more susceptible to other infections and illnesses. The specific symptoms will vary based on the type and location of the infection, but prolonged infections often result in persistent fatigue, fever, pain, and other non-specific symptoms that can significantly impact a person's quality of life.
What are the possible complications of a persistent infection?
Complications from a persistent infection can be numerous and serious. The specific complications depend heavily on the type of infection and its location in the body. For example, a persistent lung infection could lead to lung damage, abscess formation, or even respiratory failure. A persistent urinary tract infection could lead to kidney damage or sepsis. Untreated infections, regardless of their location, increase the risk of sepsis, a life-threatening condition characterized by widespread inflammation and organ dysfunction. The immune system's chronic battle against the infection can also lead to generalized fatigue, weakness, and malnutrition.
- Organ Damage: Prolonged infection can directly damage organs and tissues, affecting their function.
- Sepsis: A life-threatening condition where the body's response to infection harms its own tissues and organs.
- Chronic Fatigue and Weakness: The body's continuous fight against infection exhausts its resources, resulting in persistent fatigue.
How does a persistent infection affect the immune system?
A persistent infection puts a significant strain on the immune system. The constant battle against the pathogen can lead to immune exhaustion, leaving the body more vulnerable to other infections and illnesses. Furthermore, some infections can directly suppress or alter the immune response, further compromising the body's ability to fight off new invaders. This immunosuppression can manifest as increased susceptibility to opportunistic infections, meaning infections that typically wouldn't cause problems in a healthy individual.
- Immune Exhaustion: The immune system becomes weakened and less effective.
- Immunosuppression: The infection may directly suppress the immune system's ability to fight off pathogens.
- Increased Susceptibility to Other Infections: A weakened immune system increases the risk of secondary infections.
What are the long-term effects of untreated infections?
The long-term effects of untreated infections can be profound and wide-ranging. These effects can affect various organ systems and significantly impact a person's overall health and well-being. Some infections can lead to permanent organ damage, affecting their ability to function properly. For instance, untreated kidney infections can lead to chronic kidney disease. Similarly, untreated heart infections (endocarditis) can lead to long-term heart damage and failure. Moreover, persistent inflammation associated with chronic infections can contribute to the development of other chronic diseases like autoimmune disorders.
- Permanent Organ Damage: Untreated infections can cause lasting damage to various organs.
- Chronic Diseases: Persistent inflammation contributes to the risk of developing chronic conditions.
- Reduced Quality of Life: Long-term effects impact daily life, causing discomfort, pain, and fatigue.
How is a persistent infection diagnosed and treated?
Diagnosing a persistent infection requires a thorough medical evaluation, including a physical examination, review of medical history, and various diagnostic tests such as blood tests, imaging studies (X-rays, CT scans, ultrasounds), and cultures to identify the infecting pathogen. Treatment depends entirely on the type of infection. Antibiotics are effective against bacterial infections, while antiviral medications target viral infections. Fungal and parasitic infections require different treatments. In some cases, surgery may be necessary to remove infected tissue or drain abscesses. The course of treatment will depend on the severity of the infection and the patient's overall health.
- Physical Examination and Medical History: Doctors assess symptoms and past medical history.
- Diagnostic Tests: Blood tests, imaging studies, and cultures help identify the infection and its severity.
- Targeted Treatment: Treatment strategies vary depending on the type of infection (antibiotics, antivirals, antifungals).
What preventative measures can be taken to avoid persistent infections?
Preventing persistent infections involves a multi-pronged approach focusing on strengthening the immune system and avoiding exposure to pathogens. Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and adequate sleep, significantly boosts the immune system's ability to fight off infections. Practicing good hygiene, such as frequent handwashing, can significantly reduce the risk of infection. Staying up-to-date on vaccinations protects against many infectious diseases. Early diagnosis and treatment of any infections that do occur is also crucial in preventing them from becoming persistent.
- Healthy Lifestyle: Good nutrition, regular exercise, and adequate sleep boost immune function.
- Good Hygiene: Frequent handwashing helps prevent the spread of infection.
- Vaccinations: Immunizations protect against many infectious diseases.
What are the common signs and symptoms of infection?
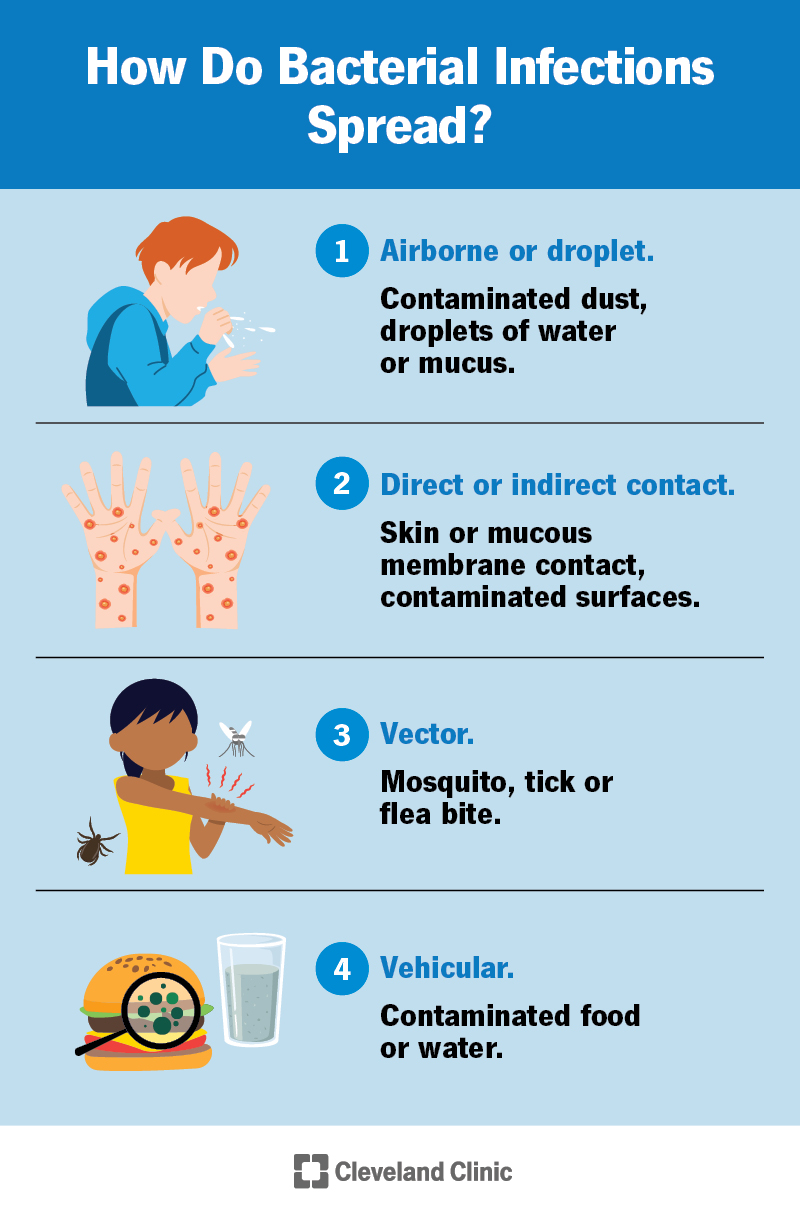
Infections manifest in a variety of ways, depending on the type of infection and the location in the body. Some general symptoms that might indicate an infection include fever (often accompanied by chills), sweating, fatigue, and muscle aches. You might also experience headaches, nausea, or vomiting. More localized symptoms depend on the site of infection. For example, a respiratory infection might present with a cough, sore throat, and congestion, while a skin infection might show redness, swelling, pain, and pus. Gastrointestinal infections can cause diarrhea, abdominal cramps, and vomiting. It’s important to remember that these are just some common symptoms, and not everyone experiences all of them. The severity of symptoms can also vary widely. Some infections cause mild discomfort, while others can be life-threatening. If you're concerned about a potential infection, it is crucial to seek medical attention for proper diagnosis and treatment. Delaying treatment can lead to serious complications.
How can I tell the difference between a viral and bacterial infection?
Differentiating between a viral and bacterial infection based solely on symptoms can be difficult, as many symptoms overlap. Both can cause fever, fatigue, and aches. However, some subtle differences might provide clues. Bacterial infections often present with localized symptoms like pus, swelling, and redness. They may also be accompanied by more intense localized pain. Viral infections, on the other hand, often cause more widespread symptoms, like body aches and fatigue, and less localized inflammation. It’s important to note that some infections are caused by neither bacteria nor viruses, but by other microorganisms like fungi or parasites. Ultimately, the only way to definitively determine the type of infection is through laboratory testing, such as a blood culture, urine culture, or swab test. A healthcare professional can assess your symptoms and order the appropriate tests to reach an accurate diagnosis and recommend the most effective treatment.
When should I seek medical attention for a suspected infection?
Seeking prompt medical attention is crucial if you suspect an infection, especially if symptoms are severe or worsening. You should consult a doctor if you have a high fever (over 103°F or 39.4°C), severe chills, difficulty breathing, persistent vomiting or diarrhea leading to dehydration, significant pain or swelling, or any signs of sepsis (such as confusion, rapid heart rate, or shortness of breath). Furthermore, if you have a compromised immune system, are pregnant, or have pre-existing medical conditions, even mild infections warrant a doctor's visit. Ignoring an infection can lead to serious complications, including sepsis, organ damage, and even death. Early diagnosis and treatment significantly improve the chances of a full recovery. Don’t hesitate to contact your doctor or seek emergency medical care if you have any concerns.
What are some ways to prevent infections?
Preventing infections involves practicing good hygiene and making healthy lifestyle choices. Regular handwashing with soap and water for at least 20 seconds, especially after using the restroom and before eating, is essential. Avoid touching your face, particularly your eyes, nose, and mouth, to prevent the spread of germs. Maintaining a healthy immune system through proper nutrition, adequate sleep, and regular exercise strengthens your body's natural defenses against infections. Vaccination is a crucial preventative measure against many infectious diseases, including influenza, pneumonia, and COVID-19. Practicing safe sex reduces the risk of sexually transmitted infections. In food preparation, maintaining proper hygiene and cooking food to safe internal temperatures minimizes the risk of foodborne illnesses. Proper wound care is also critical to prevent infections from occurring. Taking these precautions can significantly reduce your risk of contracting various infections.
Deja una respuesta