How to check infection in body

Infections can occur in various parts of the body, ranging from mild to severe. Identifying an infection early on is crucial for effective treatment and recovery. This article provides a comprehensive guide on how to check for infections in your body, covering common signs and symptoms, home tests, and when to seek professional medical attention.
How to Detect an Infection in Your Body
Signs and Symptoms of Infection
Identifying an infection often starts with recognizing common symptoms. These can vary depending on the type and location of the infection, but some general indicators include: fever (a temperature of 100.4°F or higher), chills, sweats, fatigue, muscle aches, headache, and general malaise (feeling unwell). More localized symptoms might include redness, swelling, pain, or pus at the site of infection. For example, a skin infection might show redness and swelling, while a respiratory infection might cause coughing and shortness of breath. It's crucial to remember that these are just general indicators, and a specific diagnosis requires professional medical evaluation.
When to Seek Professional Medical Advice
While some minor infections might resolve on their own, it's essential to seek medical attention if you experience: a high fever that persists, severe pain, difficulty breathing, signs of dehydration (decreased urination, dry mouth), confusion, or any symptoms that worsen despite home care. Delaying treatment for serious infections can lead to complications, so prompt medical attention is vital. Don't hesitate to contact your doctor or seek emergency care if you have concerns.
Diagnostic Tests for Infections
Your doctor will likely conduct a physical examination and ask about your symptoms to assess the possibility of an infection. Depending on the suspected location and type of infection, various diagnostic tests might be ordered. These include: blood tests (to check for elevated white blood cell count, indicating infection), urine tests (to detect urinary tract infections), stool tests (to identify gastrointestinal infections), chest X-rays (to check for pneumonia or other lung infections), swabs (to culture bacteria or viruses from infected areas), and imaging tests (such as CT scans or MRIs for deeper infections).
Home Care for Minor Infections
For minor infections like a common cold or a small cut, home care can help manage symptoms and promote healing. This includes: getting plenty of rest, drinking plenty of fluids, taking over-the-counter pain relievers (like acetaminophen or ibuprofen, as directed), applying warm or cold compresses to the affected area, and keeping the wound clean and covered. However, it's important to monitor your symptoms closely. If they worsen or don't improve within a few days, seek professional medical advice.
Preventing Infections
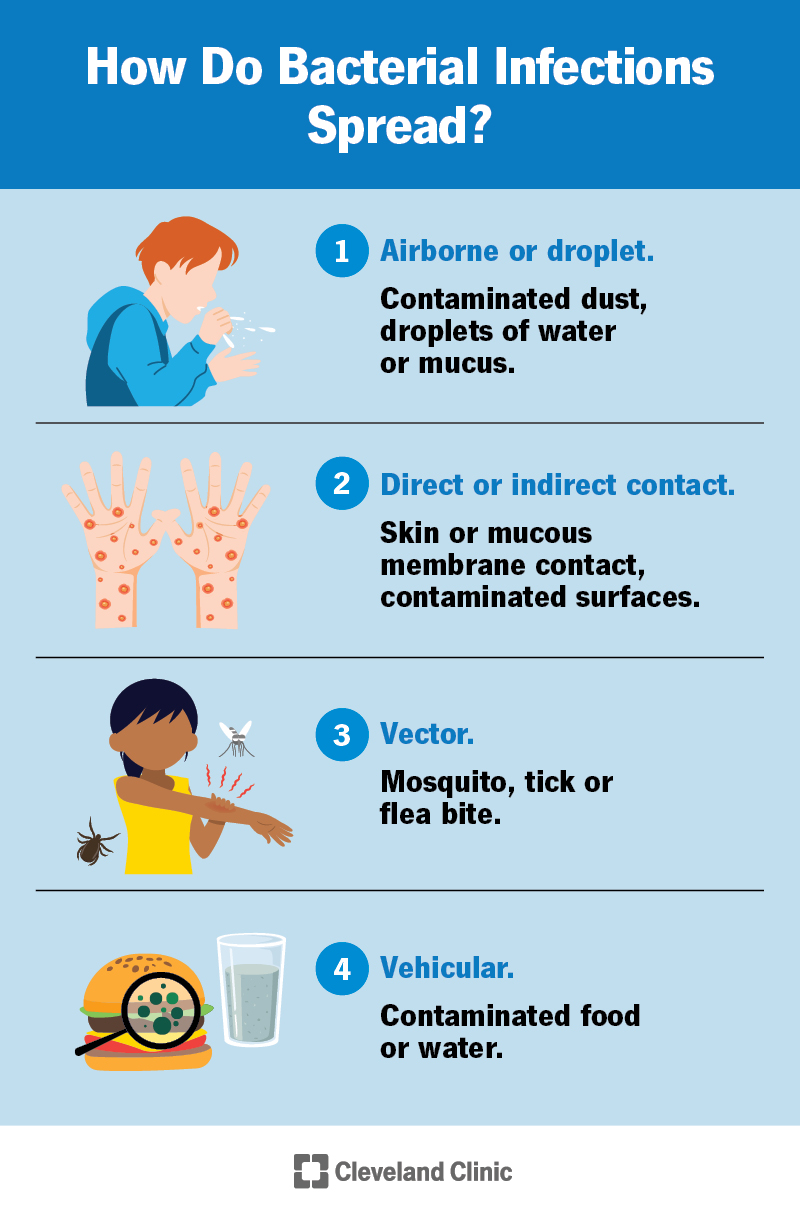
Practicing good hygiene is crucial in preventing infections. This involves: frequent handwashing with soap and water, avoiding close contact with sick individuals, getting vaccinated against preventable infections (like the flu and pneumonia), maintaining a healthy immune system through proper nutrition, exercise, and stress management, and practicing safe sex to prevent sexually transmitted infections. These preventive measures significantly reduce your risk of developing infections.
| Symptom | Possible Infection | Action |
|---|---|---|
| Fever, cough, sore throat | Upper respiratory infection (URI), influenza | Rest, fluids, over-the-counter medications; seek medical advice if severe |
| Burning urination, frequent urge to urinate | Urinary tract infection (UTI) | Seek medical advice for diagnosis and treatment |
| Redness, swelling, pain at wound site | Skin infection | Keep clean and covered; seek medical advice if worsening |
| Diarrhea, vomiting, abdominal cramps | Gastrointestinal infection | Hydration is key; seek medical advice if severe dehydration or symptoms persist |
| Persistent fatigue, unexplained weight loss | Serious underlying infection (may require further investigation) | Seek immediate medical advice |
How do they check for an infection in your body?
Checking for an infection involves a multifaceted approach, depending on the suspected location and type of infection. Diagnosis often begins with a thorough medical history, including symptoms, recent travel, and potential exposures. This is followed by a physical examination, where the doctor will look for signs of infection such as redness, swelling, warmth, pain, and pus. Further investigation often involves laboratory tests to identify the causative agent and guide treatment.
Physical Examination
A physical exam is the first step in assessing a potential infection. The doctor will observe your overall appearance, checking for signs like fever, chills, fatigue, and changes in vital signs (heart rate, blood pressure, respiratory rate). They will palpate (feel) areas of suspected infection, checking for tenderness, warmth, swelling, or abnormalities in lymph nodes. The physical exam provides crucial visual and tactile clues about the presence and severity of an infection.
- Visual inspection: Checking for redness, swelling, pus, or rashes.
- Palpation: Feeling for warmth, tenderness, or abnormalities in lymph nodes.
- Auscultation: Listening to the lungs or heart for abnormal sounds indicative of infection.
Blood Tests
Blood tests are frequently used to detect infections. A complete blood count (CBC) measures the different types of blood cells. An elevated white blood cell count (leukocytosis) often suggests an infection, though it's not always definitive. Other blood tests may measure specific antibodies or inflammatory markers, providing more specific information about the type of infection. Blood cultures may be performed to identify the specific bacteria or fungus causing the infection. These tests are important for guiding treatment decisions.
- Complete Blood Count (CBC): Checks for elevated white blood cell count indicating infection.
- C-reactive protein (CRP): Measures inflammation in the body.
- Blood cultures: Identify the bacteria or fungus causing the infection.
Imaging Tests
Imaging techniques, such as X-rays, CT scans, ultrasounds, and MRIs, can be helpful in visualizing infected areas within the body. These tests can reveal abscesses, pneumonia, or other infections not readily apparent through physical examination or blood tests. Imaging is particularly useful when an infection is deep within the body or involves specific organs.
- X-rays: Detect pneumonia or bone infections.
- CT scans: Provide detailed images of internal organs and tissues.
- Ultrasound: Useful for visualizing abscesses or fluid collections.
Fluid and Tissue Samples
When a localized infection is suspected, samples of fluid (e.g., from a wound, abscess, or cerebrospinal fluid) or tissue may be collected and sent to a laboratory for testing. This allows for direct identification of the infectious agent through microscopy, culture, and other tests. Direct testing of infected material provides the most specific information about the type of organism causing the infection.
- Wound swabs: Collect samples from infected wounds or lesions.
- Aspiration of fluid: Obtaining fluid from an abscess or infected cavity.
- Biopsy: Removing a tissue sample for microscopic examination.
Other Diagnostic Tests
Depending on the suspected type of infection, other tests may be utilized. These might include urine tests for urinary tract infections (UTIs), stool tests for gastrointestinal infections, or specific antibody tests to identify viral or parasitic infections. The choice of diagnostic test is tailored to the individual’s specific symptoms and the suspected location of infection. A comprehensive approach, combining several tests, often provides the most accurate diagnosis.
- Urine culture: Detects bacteria in the urine, indicating a UTI.
- Stool culture: Identifies bacteria, viruses, or parasites causing gastrointestinal infections.
- Serological tests: Detect antibodies against specific infectious agents.
What are five 5 signs of infection?
:max_bytes(150000):strip_icc()/signs-of-inflammation-4580526_FINAL-5c6f21adc9e77c0001be5177.png)
1. Swelling
Swelling, also known as edema, is a common sign of infection. It occurs when the body's immune system sends fluids to the infected area to fight off the invading pathogens. This influx of fluid causes the tissue to become inflamed and swollen. The degree of swelling can vary depending on the severity and location of the infection. Significant swelling, especially if accompanied by other symptoms, warrants medical attention.
- Localized swelling: Swelling confined to a specific area, such as a finger, toe, or limb.
- Generalized swelling: Swelling affecting a larger area of the body, possibly indicating a more serious systemic infection.
- Painful swelling: Often indicative of inflammation and infection.
2. Redness
Redness, or erythema, is another hallmark sign of infection. It results from increased blood flow to the infected area as part of the body's inflammatory response. The redness can range from mild pinkness to intense, bright red depending on the severity of the infection. The area may feel warm to the touch. The presence of redness, particularly if it spreads rapidly, should be monitored closely.
- Localized redness: Redness confined to a specific area around the infection site.
- Expanding redness: Redness that spreads outward from the initial site, suggesting the infection is worsening.
- Red streaks: Streaks of redness extending from the infected area, possibly indicating blood poisoning (septicemia).
3. Pain
Pain is a common symptom associated with infections, although not always present. The pain arises from the inflammation and tissue damage caused by the infection. The intensity of pain can vary significantly depending on the type and location of the infection. Sharp, throbbing, or aching pain can all be indicative of an infection.
- Localized pain: Pain confined to the infected area.
- Referred pain: Pain felt in an area distant from the infection site.
- Increasing pain: Pain that worsens over time, suggesting the infection is getting worse.
4. Pus
Pus is a thick, yellowish or greenish fluid that often indicates the presence of a bacterial infection. It's made up of dead white blood cells, bacteria, and other cellular debris. The presence of pus is a clear sign that the body is fighting off an infection, but it also means the infection is likely localized and needs treatment.
- Localized pus: Pus concentrated at the site of infection.
- Color of pus: The color of pus can give clues about the type of bacteria involved (e.g., yellow, green).
- Amount of pus: The amount of pus can indicate the severity of the infection.
5. Fever
Fever (body temperature above 100.4°F or 38°C) is a systemic sign of infection. It's triggered by the body's immune response to fight off infection. While not all infections cause fevers, a fever often suggests a more serious infection, especially if it's high or accompanied by other symptoms. High fevers should be monitored carefully, and medical attention should be sought if they persist or are accompanied by other concerning symptoms.
- High fever: Temperature significantly above normal.
- Persistent fever: Fever lasting for several days.
- Fever with chills: Indicates the body is actively fighting off infection.
How do you detect a hidden infection in your body?
Detecting a hidden infection in your body is challenging because many infections initially produce subtle or no symptoms. Diagnosis relies on a combination of recognizing potential symptoms, undergoing various medical tests, and considering your medical history and risk factors. There is no single definitive test for all hidden infections.
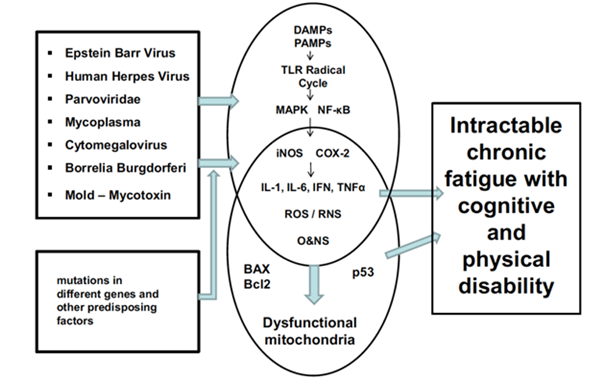
Persistent Fatigue and Low-Grade Fever
Persistent fatigue, often described as unrelenting tiredness, even after adequate rest, is a common, albeit non-specific, sign of a hidden infection. A low-grade fever, meaning a temperature slightly above normal (around 100-101°F), that persists for days or weeks, can also indicate an underlying infection. These symptoms often go unnoticed or are attributed to other causes, delaying diagnosis. It's crucial to monitor these symptoms and consult a doctor if they don't improve or worsen.
- Persistent fatigue can manifest as exhaustion that doesn't improve with rest.
- Low-grade fever can be subtle and easily missed; use a thermometer for accurate readings.
- Consult a doctor if fatigue or fever persist for more than a few days.
Unexplained Weight Loss or Loss of Appetite
Significant and unexplained weight loss, independent of dietary changes or increased physical activity, is a red flag. Similarly, a sudden and persistent loss of appetite, leading to decreased food intake, should not be ignored. These symptoms are often indicative of a more serious underlying condition, including infections that may be hidden from initial detection. Tracking your weight and appetite changes can help you and your doctor identify potential problems.
- Unexplained weight loss exceeding 5% of body weight warrants medical attention.
- Loss of appetite, especially if combined with other symptoms, necessitates a doctor's visit.
- Keep a food and weight diary to track changes over time.
Swollen Lymph Nodes
Lymph nodes are small, bean-shaped glands part of the immune system. Swelling of lymph nodes, particularly those in the neck, armpits, or groin, can indicate an infection. While swollen lymph nodes can be a sign of a minor infection, persistent or unusually large swelling may suggest a hidden or more serious infection that requires investigation. Do not attempt self-diagnosis; consult a physician for evaluation.
- Swollen lymph nodes that are tender or persist for more than two weeks require medical attention.
- Multiple swollen lymph nodes in different areas of the body are concerning.
- A doctor can determine if the swelling is caused by infection or another condition.
Changes in Bowel Habits or Skin Rashes
Alterations in bowel movements, such as persistent diarrhea or constipation, can signify infection, particularly in the gastrointestinal tract. Skin rashes, which can manifest in various ways (redness, itching, bumps), may also point to infections. These symptoms are often nonspecific, but their persistence or unusual presentation should prompt a medical evaluation. Detailed descriptions to your doctor are crucial for proper diagnosis.
- Persistent diarrhea or constipation for more than a few days needs medical assessment.
- Unexplained skin rashes, particularly if accompanied by other symptoms, should be evaluated.
- Provide a detailed description of the rash and its location to your doctor.
Elevated Inflammatory Markers in Blood Tests
Blood tests can reveal elevated levels of inflammatory markers like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). While these markers don't pinpoint the specific infection, elevated levels often indicate the presence of inflammation, a key response to infection. Your doctor may order these tests if they suspect an underlying infection based on your symptoms or medical history. These tests provide essential clues, aiding in diagnosis and guiding further investigations.
- CRP and ESR levels are indicators of inflammation in the body.
- Elevated levels may suggest an infection, but further tests are needed for confirmation.
- Blood tests are a crucial part of investigating suspected infections.
What blood tests show infection?

Several blood tests can indicate the presence of an infection. These tests generally measure things that change in your body when you're fighting off an infection, such as the number of certain types of white blood cells or the presence of specific antibodies. The specific test ordered will depend on the suspected type of infection and the patient's overall health.
Complete Blood Count (CBC)
A complete blood count (CBC) is a common blood test that provides a snapshot of your blood's components, including red blood cells, white blood cells, and platelets. In the context of infection, the white blood cell count is particularly important. A high white blood cell count (leukocytosis) often suggests the presence of an infection, though it can also be elevated due to other factors. A CBC also looks at the different types of white blood cells, which can help pinpoint the type of infection.
- Elevated white blood cell count (leukocytosis): Indicates the body is fighting an infection.
- Increased neutrophils: Suggests a bacterial infection.
- Increased lymphocytes: May indicate a viral infection, although other conditions can also cause this.
C-Reactive Protein (CRP)
C-reactive protein (CRP) is a protein produced by your liver in response to inflammation. Elevated CRP levels often signal the presence of infection, inflammation, or tissue damage. While not specific to a particular type of infection, a high CRP level can indicate that an infection is present and help monitor its response to treatment. The CRP test is often used along with other tests to get a clearer picture.
- High CRP levels: Often indicate infection, inflammation, or tissue damage.
- CRP is a nonspecific marker: It doesn't identify the type of infection.
- Useful for monitoring treatment response: CRP levels will typically decrease as the infection resolves.
Erythrocyte Sedimentation Rate (ESR)
The erythrocyte sedimentation rate (ESR) measures how quickly red blood cells settle at the bottom of a test tube. A higher than normal ESR indicates inflammation in the body, which is often associated with infection, but also other conditions like autoimmune diseases. Like CRP, the ESR is a nonspecific marker and doesn't identify the type of infection.
- Elevated ESR: Indicates inflammation, often associated with infection.
- Nonspecific marker: Doesn't specify the type of infection.
- Useful for monitoring disease activity: Changes in ESR can be used to track the progress of an infection or inflammatory condition.
Procalcitonin (PCT)
Procalcitonin (PCT) is a protein produced by certain cells in response to bacterial infection. PCT levels are generally elevated in severe bacterial infections, and monitoring PCT levels can help differentiate between bacterial and viral infections. It is less useful for other types of infections.
- Elevated PCT: Strongly suggests a bacterial infection.
- Useful in differentiating bacterial from viral infections: PCT is typically not elevated in viral infections.
- Can aid in antibiotic stewardship: Helps determine the need for antibiotics.
Blood Cultures
Blood cultures are the most direct way to identify the specific bacteria or fungi causing an infection. A sample of blood is cultured in a lab to allow any microorganisms present to grow. Blood cultures are crucial for identifying the specific pathogen and determining the most effective antibiotic treatment. This test is more often performed when a serious or life-threatening infection is suspected.
- Identifies specific pathogens: Allows for targeted antibiotic therapy.
- Essential for serious infections: Guides treatment decisions in severe cases.
- Can be time-consuming: Results may take several days to become available.
How can I tell if I have an infection?
Determining if you have an infection can be tricky, as symptoms can vary widely depending on the type and location of the infection. Common signs include fever, chills, sweating, fatigue, and muscle aches. However, these are general symptoms and don't pinpoint a specific infection. More localized symptoms might include redness, swelling, pain, or pus at the site of infection. For example, a skin infection might present with a red, warm, and painful bump, while a respiratory infection might cause a cough, sore throat, and congestion. Gastrointestinal infections often manifest as diarrhea, vomiting, and stomach cramps. It's crucial to remember that many infections are asymptomatic, meaning they don't produce noticeable symptoms. If you suspect an infection, particularly if you're experiencing severe symptoms, it's essential to seek professional medical advice. A doctor can perform a physical examination, order laboratory tests (like blood cultures or urine analysis), or imaging studies (such as X-rays or ultrasounds) to accurately diagnose the infection and recommend appropriate treatment. Self-treating an infection can be dangerous and may delay proper care, leading to complications.
What are some common tests to check for infection?
Several tests can help diagnose an infection, depending on the suspected location and type. Blood tests are frequently used to detect infections. A complete blood count (CBC) can reveal elevated white blood cell counts, indicating the body's response to an infection. Blood cultures are used to identify the specific bacteria or fungi causing the infection. Urine tests are useful for detecting urinary tract infections (UTIs), looking for bacteria or signs of inflammation. Sputum cultures are employed for respiratory infections, analyzing the mucus coughed up to identify the causative agent. Stool tests can identify intestinal infections by examining stool samples for bacteria, viruses, or parasites. Imaging techniques such as X-rays, CT scans, or ultrasounds might be used to visualize infections in specific body areas, like pneumonia in the lungs or an abscess. Finally, wound cultures are performed by taking a sample from an infected wound to determine the type of bacteria present. The specific test(s) recommended will depend on your symptoms and the doctor's assessment.
How can I prevent infections?
Preventing infections involves a combination of hygiene practices and lifestyle choices. Good hand hygiene is crucial: wash your hands frequently with soap and water for at least 20 seconds, especially after using the restroom, before eating, and after touching public surfaces. Avoid touching your face, particularly your eyes, nose, and mouth, as this can transfer germs. Maintaining a healthy immune system is key; ensure you get enough sleep, eat a nutritious diet, and manage stress effectively. Vaccination is a powerful preventative measure against numerous infectious diseases. Stay up-to-date on recommended vaccines, including flu shots and others specific to your age and health status. Practice safe sex to prevent sexually transmitted infections (STIs). Proper food handling and preparation are essential to avoid foodborne illnesses. Cook food thoroughly, wash fruits and vegetables, and refrigerate perishable items promptly. If you have a wound, keep it clean and covered to prevent infection. Finally, be mindful of your surroundings; avoid contact with individuals who are sick and practice good respiratory etiquette (covering your mouth and nose when coughing or sneezing).
When should I see a doctor about a possible infection?
You should seek immediate medical attention if you experience any of the following: a high fever (over 101°F or 38.3°C), severe chills, difficulty breathing, chest pain, severe abdominal pain, signs of dehydration (decreased urination, dizziness), a wound that shows signs of serious infection (excessive swelling, redness, pus, or increasing pain), or any symptoms that worsen rapidly or are accompanied by significant discomfort. While many infections can be managed at home with rest and over-the-counter medications, it's important to seek professional medical care for infections that don't improve or worsen despite self-care measures. Early diagnosis and treatment are crucial for preventing complications and ensuring a full recovery. Delaying treatment can lead to the spread of infection, organ damage, and even life-threatening conditions in some cases. Don't hesitate to contact your doctor or other healthcare provider if you have any concerns about a possible infection.
Deja una respuesta