What are the 7 signs of infection

In the realm of human health, infection remains a formidable foe, threatening our well-being and potentially causing serious harm. Understanding the telltale signs of an infection is crucial for timely intervention and effective treatment. This article delves into the seven key indicators of infection, providing readers with the knowledge they need to recognize this condition and seek appropriate medical attention when necessary.
Recognizing the 7 Signs of Infection
Recognizing the signs of infection is crucial for timely treatment and preventing complications. While the severity and presentation of infection can vary greatly depending on the type of infection and individual health, seven common signs can help you identify a potential problem.
1. Swelling (Edema)
Swelling or edema occurs when excess fluid accumulates in the infected area. This is often a result of the body's inflammatory response to the infection. The area may appear larger than normal and feel puffy or tight. The severity of the swelling can range from mild to severe, depending on the infection's severity and location. For example, a minor skin infection might only show slight swelling, while a more serious infection like cellulitis could cause significant swelling and redness.
2. Redness (Erythema)
Redness around the site of infection is another key indicator. This redness is caused by increased blood flow to the area as the body tries to fight the infection. The redness might be localized to a small area, or it could be more widespread, depending on the extent of the infection. The intensity of the redness can also vary – from a faint blush to a deep, fiery red. This is a visible sign of inflammation.
3. Pain or Tenderness
Pain or tenderness at the site of the infection is a common symptom. The pain can range from mild discomfort to severe throbbing or sharp pain. The severity of the pain often correlates with the severity of the infection. The infected area may be painful to the touch, even a gentle touch. This pain is often a result of inflammation, pressure from swelling, and tissue damage.
4. Warmth
The infected area may feel warmer than the surrounding tissue. This increased warmth is due to the increased blood flow to the area as part of the inflammatory response. You might notice this warmth by simply touching the area, comparing it to the surrounding skin temperature. This warmth is often accompanied by other signs, such as redness and swelling.
5. Loss of Function
Depending on the location of the infection, there might be loss of function in the affected area. For example, an infected finger joint might make it difficult to bend or straighten the finger. Similarly, an infection in the leg might make walking painful or difficult. This impaired function is often due to pain, swelling, and inflammation limiting the movement of the affected area.
6. Pus
Pus, a thick, yellowish-white or greenish fluid, is a common sign of infection, particularly bacterial infections. It is composed of dead white blood cells, bacteria, and other cellular debris. The presence of pus indicates that the body is fighting the infection, but it also signifies a more serious infection that might require medical attention. Pus often accompanies other symptoms, like pain, swelling, and redness.
7. Fever
A fever (body temperature above 100.4°F or 38°C) is a systemic sign of infection. This elevated temperature is the body's attempt to fight off the infection. While a fever isn't always present in all infections, it often accompanies more serious or systemic infections. A high fever warrants medical attention.
| Sign | Description |
|---|---|
| Swelling (Edema) | Excess fluid accumulation in the infected area. |
| Redness (Erythema) | Increased blood flow causing redness at the infection site. |
| Pain or Tenderness | Discomfort or pain in the infected area. |
| Warmth | Increased temperature at the infection site. |
| Loss of Function | Impaired use of the infected area. |
| Pus | Thick, yellowish-white or greenish fluid. |
| Fever | Elevated body temperature. |
How do you know if your body is full of infection?
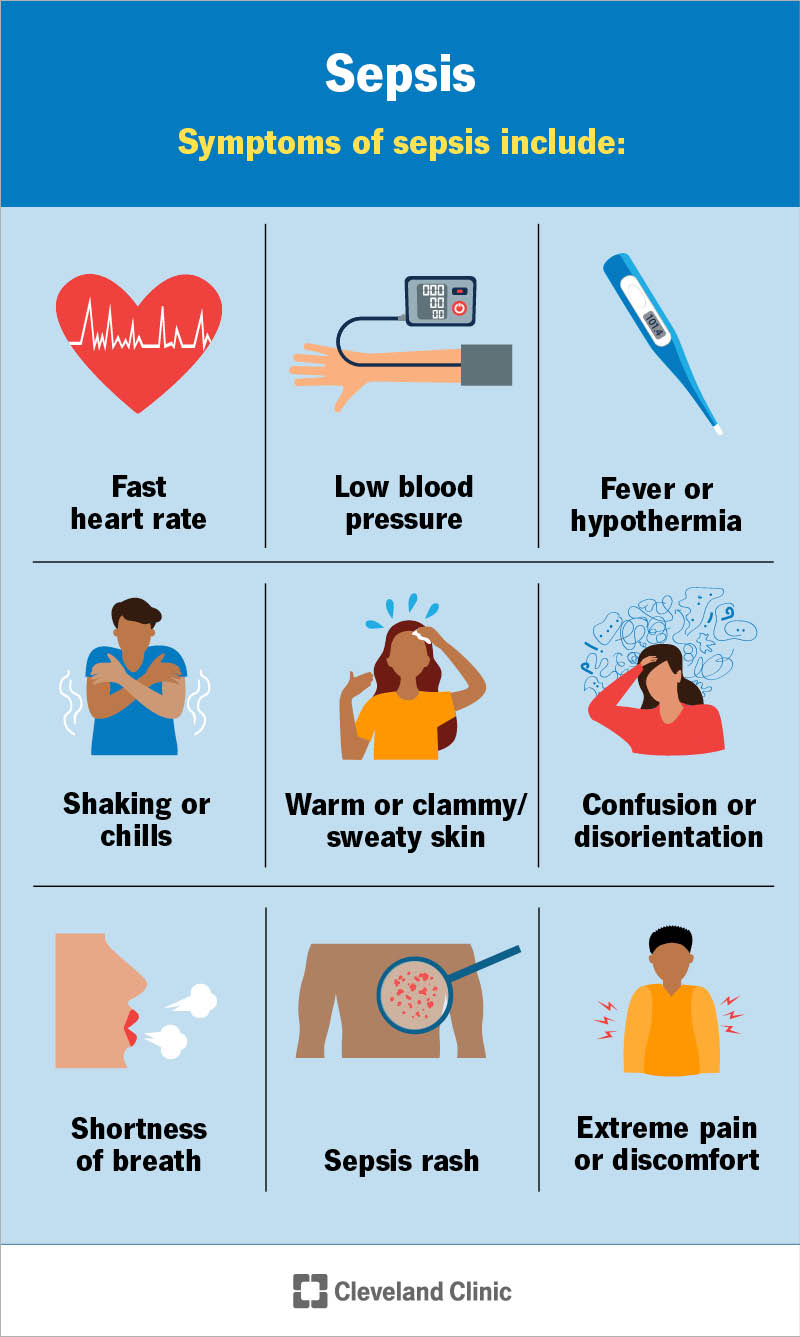
Determining if your body is fighting a widespread infection (septicemia or sepsis) is complex and requires professional medical evaluation. There's no single symptom that guarantees an infection, and symptoms can vary greatly depending on the type of infection and your overall health. However, several signs indicate a potential problem that necessitates immediate medical attention. Fever, chills, and extreme fatigue are common, but often, infections manifest in more subtle ways, making early diagnosis challenging. The severity of symptoms also depends on the location and type of infection. A localized infection like a skin boil might have limited symptoms, while a systemic infection like pneumonia can cause widespread effects.
1. Fever and Chills
A high fever (over 101°F or 38.3°C) is a classic sign of infection. Your body's immune system is raising your temperature to fight off invaders. Accompanying chills, despite the fever, indicate that your body is working hard to combat the infection. However, it's important to note that not all infections cause a fever, and some conditions can cause fever without infection.
- High temperature: Sustained fever above the usual range.
- Shivering and chills: Even while feeling hot, experiencing intense shaking.
- Sweating: Profuse sweating can accompany fever as the body attempts to regulate temperature.
2. Fatigue and Weakness
Feeling unusually tired or weak is a common sign your body is battling an infection. Your immune system is working overtime, diverting energy from other bodily functions. This fatigue can range from mild tiredness to debilitating exhaustion, preventing you from performing everyday activities. Prolonged or excessive fatigue warrants immediate medical attention.
- Unexplained tiredness: Persistent fatigue not relieved by rest.
- Muscle weakness: Difficulty with simple movements or physical exertion.
- Lack of energy: Feeling drained and unable to participate in daily life.
3. Changes in Heart Rate and Breathing
Your heart rate and breathing rate can increase as your body fights infection. This is because your body needs more oxygen to power the immune response. Rapid heart rate (tachycardia) and rapid breathing (tachypnea) are significant indicators of a potential systemic infection and should be evaluated by a doctor. Pay close attention to any changes in your breathing, especially if you experience shortness of breath.
- Increased heart rate: A persistently elevated heart rate above your normal resting rate.
- Rapid breathing: Breathing faster and shallower than usual.
- Shortness of breath: Difficulty catching your breath or feeling winded easily.
4. Skin Changes
Infections can manifest on your skin through various changes. These might include redness, swelling, warmth, and pain around an area of infection. More serious infections can lead to widespread rashes, lesions, or changes in skin color. Any unexpected skin changes, particularly those accompanied by fever or other symptoms, warrant prompt medical attention.
- Redness and swelling: Inflammation around a wound or infected area.
- Pus or drainage: Discharge from a wound or infected area.
- Rashes or lesions: Unexplained skin eruptions or sores.
5. Other Systemic Symptoms
Several other symptoms can indicate a widespread infection. These include nausea, vomiting, diarrhea, confusion, and disorientation. These symptoms reflect the body's overall response to the infection, and often indicate a serious condition. Severe abdominal pain can also be a sign of infection within the abdominal cavity. Don't hesitate to seek immediate medical help if you experience these symptoms along with other warning signs.
- Nausea and vomiting: Feeling sick to your stomach and throwing up.
- Diarrhea: Loose, watery stools.
- Confusion and disorientation: Difficulty thinking clearly or being aware of your surroundings.
How to remove an infection from the body?
How to remove an infection from the body depends entirely on the type of infection, its severity, and your overall health. There's no single answer, and attempting self-treatment can be dangerous. Always consult a medical professional for diagnosis and treatment. They can accurately identify the infection (bacterial, viral, fungal, parasitic) and prescribe the appropriate course of action. This might involve antibiotics, antiviral medications, antifungals, or antiparasitics, depending on the causative agent. In some cases, surgical intervention may be necessary to drain an abscess or remove infected tissue. Supportive care, such as rest, fluids, and pain management, will also be important.
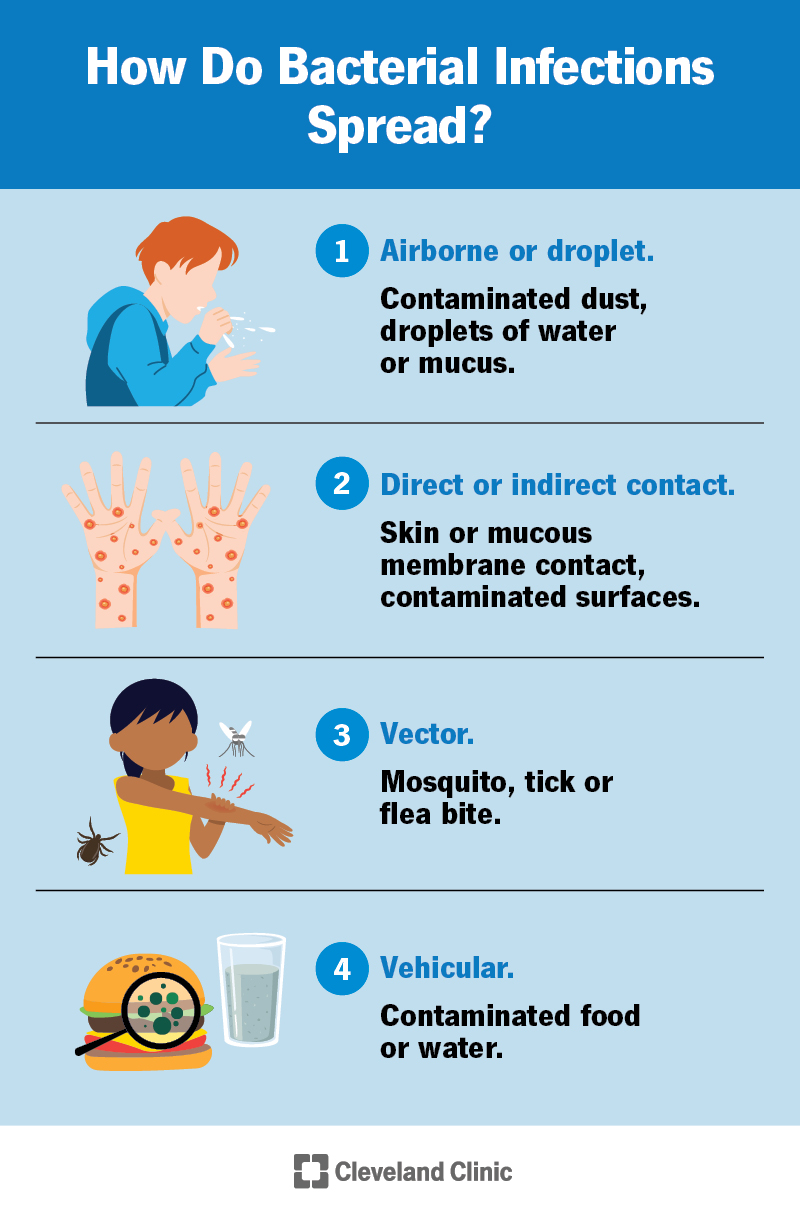
Understanding the Different Types of Infections
Infections are caused by various pathogens, each requiring a specific treatment approach. Bacterial infections are often treated with antibiotics, while viral infections typically require supportive care as the body's immune system fights the virus. Fungal infections might necessitate antifungal medications, and parasitic infections demand antiparasitic drugs. Correct identification is crucial for effective treatment. Misdiagnosis and improper treatment can lead to complications and antibiotic resistance.
- Bacterial infections: These are treated with antibiotics. Examples include strep throat, pneumonia, and urinary tract infections.
- Viral infections: Often resolve on their own with supportive care. Examples include the common cold, influenza, and some types of gastroenteritis.
- Fungal infections: Can affect the skin, nails, or internal organs and require antifungal medications.
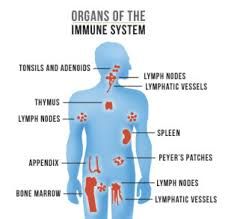
The Role of Your Immune System
Your body's immune system plays a crucial role in fighting infections. A healthy immune system is better equipped to combat pathogens. Therefore, maintaining a healthy lifestyle is vital in preventing and managing infections. This includes: getting enough sleep, eating a balanced diet, managing stress, and exercising regularly. Boosting your immune system isn't about taking magic supplements; it's about consistently adopting healthy habits. If your immune system is compromised, you're at higher risk of developing severe infections.
- Adequate sleep: Allows your body to repair and regenerate.
- Balanced nutrition: Provides the necessary nutrients for immune function.
- Stress management: Chronic stress weakens the immune system.
Medical Interventions for Infections
Depending on the type and severity of the infection, your doctor might recommend various medical interventions. Antibiotics are used for bacterial infections, while antivirals target viruses. Antifungals combat fungal infections, and antiparasitics are used for parasitic infections. In more severe cases, surgery might be necessary to drain abscesses or remove infected tissue. Intravenous (IV) fluids might be administered to treat dehydration, a common symptom of many infections. Always follow your doctor's prescribed treatment plan meticulously.
- Antibiotics: Kill bacteria or stop their growth.
- Antivirals: Inhibit viral replication.
- Surgery: To drain abscesses or remove infected tissue.
Home Remedies and Supportive Care
While home remedies cannot cure infections, they can provide supportive care to alleviate symptoms and help your body fight off the infection. These include: getting plenty of rest, drinking plenty of fluids, and eating a nutritious diet. Over-the-counter pain relievers can help manage fever and discomfort. However, it's important to remember that home remedies should never replace medical treatment. They are only supplemental.
- Rest: Allows your body to focus its energy on fighting the infection.
- Hydration: Prevents dehydration and helps flush out toxins.
- Nutritious diet: Provides essential nutrients to support immune function.
Preventing Infections
Preventing infections is far easier than treating them. Practicing good hygiene, such as regular handwashing, is crucial. Avoiding contact with infected individuals, getting vaccinated against preventable diseases, and maintaining a healthy lifestyle significantly reduce the risk of infection. Proper wound care is also essential to prevent infections from developing. Regular checkups with your doctor can also help identify and address potential health issues before they escalate into serious infections.
- Handwashing: The most effective way to prevent the spread of infections.
- Vaccinations: Protect against various infectious diseases.
- Healthy lifestyle: A strong immune system is the body's first line of defense.
How do you know your body is fighting an infection?
How Do You Know Your Body is Fighting an Infection?
Your body's immune system is constantly working to protect you from invading pathogens like bacteria, viruses, fungi, and parasites. When an infection occurs, your body initiates a complex response to eliminate the threat. This response can manifest in a variety of ways, depending on the type and severity of the infection, as well as your individual immune response. Recognizing these signs can help you seek appropriate medical attention when necessary. However, it's crucial to remember that these symptoms can also be indicative of other conditions, so a medical professional's diagnosis is vital.
Signs and Symptoms of Infection
Infections often trigger a noticeable inflammatory response. This means your body sends immune cells to the site of the infection to combat the invaders. This process can cause various symptoms, ranging from mild discomfort to severe illness. Fever is a common symptom, as your body increases its temperature to hinder the growth of pathogens. Other common signs include fatigue, muscle aches, and general malaise (feeling unwell). The specific symptoms will largely depend on where the infection is located and the type of pathogen involved. For example, a respiratory infection might cause coughing and a sore throat, while a urinary tract infection might lead to painful urination and abdominal discomfort. Recognizing these early warning signs is crucial for prompt treatment.
- Fever: Elevated body temperature (usually above 100.4°F or 38°C).
- Chills: Feeling cold despite a warm environment.
- Fatigue: Extreme tiredness and lack of energy.
Changes in Your Blood
Your blood plays a central role in fighting infection. During an infection, your body increases the production of white blood cells (leukocytes), the primary cells of your immune system that combat pathogens. A complete blood count (CBC) test can reveal these changes. Elevated white blood cell count (leukocytosis) is often a strong indication of an infection. Moreover, other blood markers, like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), can also increase during infection reflecting the inflammatory response. These tests, ordered and interpreted by a doctor, help determine the severity and type of infection.
- Increased White Blood Cell Count: Indicates your body is actively fighting infection.
- Elevated CRP and ESR: These are markers of inflammation, often elevated during infection.
- Changes in other blood components: Depending on the infection, other blood components might show alterations.
Localized Symptoms at the Site of Infection
The location of the infection significantly influences the symptoms you experience. For instance, a skin infection might present with redness, swelling, warmth, and pain at the infected site. This is due to the body's inflammatory response localized to the area. A respiratory infection might cause coughing, congestion, and shortness of breath, while a gastrointestinal infection may lead to nausea, vomiting, diarrhea, and abdominal cramps. These localized symptoms provide crucial clues about the infection's location and can help guide diagnosis and treatment.
- Redness, Swelling, and Pain: Common signs of localized infection, particularly in skin infections.
- Pus or Drainage: Indicates the presence of infection and the body's attempt to eliminate it.
- Specific Symptoms based on Location: Respiratory, gastrointestinal, urinary, and other infections have their specific symptoms.
Swollen Lymph Nodes
Lymph nodes are small, bean-shaped glands that are part of your immune system. They filter lymph fluid, trapping pathogens and immune cells. When your body is fighting an infection, the lymph nodes nearest to the infection site may become swollen and tender. This is because they are working overtime to filter out the infection. Swollen lymph nodes are not always a sign of infection, but they are a significant indicator, especially when combined with other symptoms. Palpable swollen lymph nodes, often felt in the neck, armpits, or groin, should be evaluated by a healthcare professional.
- Swelling in lymph nodes: Often indicates a nearby infection.
- Tenderness to the touch: Swollen nodes are often painful when pressed.
- Localized swelling: Swelling is usually near the site of the infection.
Systemic Symptoms of Infection
Beyond localized symptoms, infections can cause more widespread systemic effects. This means that the infection impacts your entire body, leading to general malaise, fatigue, weakness, headache, and loss of appetite. These symptoms arise from the body's overall immune response and the release of inflammatory mediators. The severity of systemic symptoms can vary greatly depending on the type of infection and the individual's health status. These symptoms often necessitate seeking medical attention, particularly if they are severe or persistent.
- Malaise: A general feeling of discomfort, illness, or unease.
- Fatigue and Weakness: Significant tiredness and lack of strength.
- Headache, Muscle aches: Widespread pain throughout the body.
How to check infection in body?
How to Check for Infection in the Body
Checking for infection involves a multifaceted approach, combining self-assessment with professional medical evaluation. There's no single test to definitively identify all types of infections. The methods used depend on the suspected location and type of infection (bacterial, viral, fungal, parasitic). Symptoms are often the first indicator, but these can vary widely depending on the infectious agent and the individual's immune response. A doctor will utilize a combination of methods to arrive at a diagnosis, including a physical examination, medical history review, and various laboratory tests.
Observing Symptoms
Many infections present with characteristic symptoms, though some may be subtle or mimic other conditions. Paying close attention to your body is crucial. If you experience persistent symptoms, it's essential to seek medical advice. Early detection and treatment are key for most infections.
- Fever: A consistently elevated body temperature (above 100.4°F or 38°C) is a common sign of infection.
- Pain: Localized pain, swelling, redness, or tenderness at the site of a potential infection.
- Other Symptoms: These can include fatigue, chills, nausea, vomiting, diarrhea, cough, shortness of breath, or changes in mental status.
Physical Examination by a Doctor
A doctor will conduct a thorough physical examination to assess for signs of infection. This may involve checking vital signs (temperature, pulse, blood pressure, breathing rate), examining the affected area (if applicable), and listening to the heart and lungs. The physical exam provides valuable clues, helping to guide further investigations.
- Visual Inspection: Examining the skin for redness, swelling, pus, or other signs of localized infection.
- Palpation: Feeling the affected area for tenderness, warmth, or firmness.
- Auscultation: Listening to the lungs or heart for abnormal sounds indicative of infection (e.g., wheezing, crackles).
Laboratory Tests
Laboratory tests play a vital role in confirming the presence of an infection and identifying the causative organism. The specific tests ordered will depend on the suspected type of infection and its location. Results provide crucial information for effective treatment.
- Blood Tests: Complete blood count (CBC) to assess white blood cell count (an indicator of infection), blood cultures to identify bacteria in the bloodstream.
- Urine Tests: To detect urinary tract infections (UTIs) through urinalysis and urine cultures.
- Other Tests: Depending on the suspected infection, other tests may include stool cultures, sputum cultures, biopsies, imaging studies (X-rays, CT scans, ultrasounds).
Medical History Review
A comprehensive medical history is crucial in assessing the risk of infection and guiding diagnostic testing. This involves discussing past medical conditions, current medications, recent travel history, and any potential exposure to infectious agents. Understanding a patient's history is vital in the diagnostic process.
- Recent Illnesses: Details about any recent illnesses or infections.
- Medications: Current medications, including antibiotics or immunosuppressants.
- Exposure History: Information about potential exposure to infectious agents (e.g., contaminated food or water, contact with infected individuals).
Imaging Studies
Imaging techniques like X-rays, CT scans, MRIs, and ultrasounds can help visualize infections in different parts of the body. These are especially useful for detecting infections in organs or deep tissues that are not easily accessible for direct examination. Imaging provides visual confirmation of the infection's location and extent.
- X-rays: Useful for detecting pneumonia or bone infections.
- CT scans: Provide detailed images of internal organs and can detect abscesses or other localized infections.
- Ultrasound: Often used for examining soft tissues and identifying fluid collections associated with infection.
What are the seven classic signs of infection?
The seven classic signs of infection, often remembered by the acronym "rubor, calor, dolor, tumor, functio laesa, plus loss of function and fever", are a helpful starting point, but it's crucial to remember that not all infections present with all seven. Rubor (redness) indicates increased blood flow to the affected area due to inflammation. Calor (heat) is a related symptom, also stemming from increased blood flow. Dolor (pain) arises from the inflammation and irritation of nerve endings. Tumor (swelling) is caused by the accumulation of fluid in the infected tissue. Functio laesa (loss of function) means the affected area is not working properly. This could be anything from a stiff joint to difficulty moving a limb. Finally, fever is a systemic sign of infection, representing the body's attempt to fight off the invading pathogen. However, it’s important to understand that not all infections cause fever, particularly localized infections. The presence of these signs should prompt a medical evaluation.
Can an infection occur without all seven classic signs?
Absolutely. The seven classic signs are a guideline, not an absolute rule. Many infections present with only some of these signs, or even with none of them at all. For example, a urinary tract infection (UTI) may primarily present with pain during urination and increased urgency, with few or no other visible signs. Similarly, a viral infection might present mostly with fatigue and a low-grade fever, lacking the localized signs of redness, swelling, or pain. Systemic infections, such as sepsis, may primarily manifest as fever, chills, and a general feeling of unwellness, without localized symptoms. Atypical infections, caused by unusual or less common pathogens, may show completely different symptoms. Therefore, relying solely on the presence or absence of all seven signs to diagnose an infection is insufficient. Medical attention is needed for proper diagnosis and treatment. It's crucial to seek medical advice if you suspect an infection, even if you don't experience all seven classic signs.
What are some less obvious signs of infection?
Beyond the classic seven, several less obvious signs can indicate an infection. These can be subtler symptoms that are easily missed or attributed to other causes. For example, unexplained fatigue, persistent chills, muscle aches, headache, nausea, vomiting, and diarrhea can all be indicative of infection, particularly systemic infections. Changes in mental state, such as confusion or disorientation, can also be a sign of a severe infection. Changes in bowel habits beyond diarrhea, like constipation, can point towards infection, depending on the location and nature of the infection. Furthermore, seemingly unrelated symptoms like persistent cough or skin rashes may be connected to an underlying infection. Early recognition of these subtle signs is essential for timely treatment to prevent serious complications.
When should I seek medical attention for a suspected infection?
You should seek medical attention immediately if you suspect an infection and are experiencing any of the following: a high fever (especially over 103°F or 39.4°C), severe pain, rapidly spreading redness or swelling, difficulty breathing, signs of dehydration, confusion or disorientation, or any signs of sepsis (such as a rapid heart rate, low blood pressure, and difficulty breathing). Even if the symptoms appear mild, don't hesitate to contact a doctor if you have concerns or the infection doesn't improve with home care within a reasonable time. Early diagnosis and treatment are vital in preventing complications and ensuring a faster recovery. Delaying treatment could lead to serious health consequences, especially with infections like pneumonia, meningitis, or sepsis. Your doctor can properly assess your condition, perform necessary tests, and prescribe appropriate medication.
Deja una respuesta