What disease almost killed humanity

On the brink of extinction, humanity faced a terrifying foe—a relentless disease that ravaged populations and threatened to obliterate civilizations. From Egypt's ancient curses to Europe's darkest chapter, history bears witness to its destructive power. This article delves into the chilling tale of the disease that almost extinguished the human flame.
The Black Death: A Plague That Nearly Wiped Out Humanity
The Black Death, also known as the Plague, is arguably the disease that came closest to extinguishing humanity. Between 1346 and 1353, it swept across Eurasia, killing an estimated 30-60% of Europe's population. This devastating pandemic, caused by the bacterium Yersinia pestis, left an indelible mark on history, profoundly impacting society, culture, religion, and the very fabric of human civilization. The sheer scale of mortality was unprecedented, leading to widespread social disruption, economic collapse, and significant shifts in power dynamics. The speed of transmission and the high mortality rate made it exceptionally dangerous, with victims often succumbing within days of showing symptoms.
The Bacterial Culprit: Yersinia pestis
The Black Death was caused by the bacterium Yersinia pestis, transmitted primarily through the bites of infected fleas that lived on black rats. These rats were common in medieval cities, providing an ideal breeding ground for the disease. The bacteria rapidly multiplied within the host, leading to various forms of the plague: bubonic, septicemic, and pneumonic. The bubonic plague, characterized by swollen lymph nodes (buboes), was the most common form. Septicemic plague affected the bloodstream, while pneumonic plague infected the lungs and could spread through airborne droplets, making it particularly contagious and deadly.
The Spread and Impact of the Plague
The Black Death originated in Central Asia and spread rapidly along trade routes, particularly the Silk Road. The disease's rapid spread was facilitated by the dense populations in medieval cities and the lack of sanitation and hygiene. Ships carrying infected rats traveled to port cities, disseminating the plague across vast distances. The pandemic's impact was catastrophic. Mass graves became commonplace, and entire villages and towns were decimated. The social and economic consequences were far-reaching, with labor shortages leading to significant changes in social structures and the feudal system.
Long-Term Effects on Society and Culture
The Black Death’s legacy extends far beyond its immediate mortality. The massive loss of life significantly altered the social landscape of Europe. The shortage of workers led to increased wages and improved working conditions for the surviving population, albeit temporarily. The plague also profoundly influenced religious beliefs and practices, with some attributing the pandemic to divine punishment. This led to increased religious fervor but also fueled antisemitism, as Jews were often scapegoated for the calamity.
Medical Understanding and Treatments of the Time
Medieval medical understanding of the plague was severely limited. Treatments were often ineffective and sometimes even harmful. Common practices included bloodletting, applying herbal remedies, and religious rituals. The lack of understanding about the disease's transmission meant that effective preventative measures were absent. The development of effective treatments and preventive measures had to wait for centuries until the discovery of antibiotics.
| Plague Type | Transmission | Symptoms | Mortality Rate |
|---|---|---|---|
| Bubonic | Flea bites | Swollen lymph nodes (buboes), fever, chills | 30-60% |
| Septicemic | Direct contact with infected blood | Fever, chills, internal bleeding, organ failure | High (often fatal) |
| Pneumonic | Airborne droplets | Fever, chills, cough, bloody sputum | Very high (often fatal) |
https://youtube.com/watch?v=the-diseases-that-changed-humanity-forever-381514
What disease almost made humans extinct?
What Disease Almost Made Humans Extinct?
There's no single disease definitively proven to have nearly wiped out humanity. However, several severe bottlenecks in human population history have been linked to potential infectious disease outbreaks. The most compelling candidate is a retrovirus similar to HIV, although the specific pathogen remains unknown. Genetic evidence suggests a significant population crash around 70,000 years ago, a period often referred to as the Toba catastrophe theory (though the cause of this bottleneck is debated). While volcanic eruptions and other environmental factors are also considered, the rapid spread and severity of a highly infectious disease could significantly contribute to such a dramatic reduction in human numbers. It's important to note that this is a hypothesis based on indirect evidence, and the precise nature and impact of any such disease remain a subject of ongoing research. Other infectious diseases, while not necessarily causing near extinction, had profound and devastating effects on human populations throughout history (e.g., the Black Death).
Possible Candidates for a Near-Extinction Event
Several infectious agents are theorized to have potentially caused massive population reductions in early humans. While definitive proof is elusive due to the limitations of archaeological and genetic data from that time period, analyzing patterns in human genetic diversity provides clues. For instance, the low genetic diversity observed in modern humans suggests a period of severe population constriction, potentially caused by a pandemic disease that could have easily swept through small, interconnected populations. The timing of this bottleneck aligns with theories about the impact of a supervolcano eruption. However, a virulent disease could have exacerbated the effects of the environmental disaster.
- Retroviruses: These viruses integrate their genetic material into the host's DNA, making them particularly difficult to eradicate. A powerful retrovirus, potentially similar to HIV but with higher mortality rates, is considered a plausible candidate for a near-extinction event.
- Other Unknown Pathogens: The possibilities extend beyond known pathogens. Ancient viruses or bacteria that no longer exist or have evolved significantly could be responsible. Lack of contemporary records leaves a gap in our understanding of these possible culprits.
- Combination of Factors: A disease alone might not have been enough to cause near-extinction. The combined effects of disease, climate change, or other environmental disasters likely played a role in shaping human population dynamics in the past.
The Toba Catastrophe Theory and Disease
The Toba supervolcanic eruption approximately 74,000 years ago is widely discussed as a potential cause for a significant human population bottleneck. The eruption unleashed massive amounts of ash and gases into the atmosphere, causing a "volcanic winter" that drastically affected the environment. This environmental catastrophe could have made human populations more vulnerable to disease. A widespread infectious disease could have ravaged already weakened communities, accelerating population decline.
- Environmental Stress: The Toba eruption created widespread environmental devastation, leading to food shortages and habitat loss. Such conditions would severely weaken human immune systems, making them highly susceptible to infectious diseases.
- Increased Disease Transmission: Environmental disruption could have forced humans into closer proximity, increasing the rate of disease transmission among individuals and groups.
- Resource Competition: Scarcity of resources in the aftermath of the eruption likely triggered conflict and migration, further spreading diseases.
Genetic Evidence and Population Bottlenecks
Genetic research has been instrumental in providing insights into human population history. By analyzing genetic diversity within and between human populations, scientists can infer past population sizes and migration patterns. Low genetic diversity in modern humans strongly suggests a period of extremely low population numbers in the past. This limited genetic variability could be a direct consequence of a severe population bottleneck caused, at least in part, by an infectious disease outbreak.
- Mitochondrial DNA Analysis: Studies of mitochondrial DNA (mtDNA), which is passed down maternally, have been used to trace human lineages and estimate past population sizes. Findings suggest a dramatic reduction in human population thousands of years ago.
- Y-Chromosome Analysis: Similarly, Y-chromosome analysis, focusing on the paternal lineage, supports the findings from mtDNA studies and provides additional evidence of a past population bottleneck.
- Nuclear DNA Analysis: Analysis of nuclear DNA provides a more complete picture of human genetic diversity and further supports the theory of a significant population constriction.
The Challenges of Studying Ancient Diseases
Reconstructing the history of ancient diseases is incredibly challenging. Direct evidence, such as preserved viral or bacterial remains, is extremely rare. Researchers rely on indirect evidence, such as genetic data, archaeological findings, and historical accounts (when available), to make inferences. The limitations of these sources often lead to uncertainty in determining the exact causes and consequences of past pandemics.
- Preservation of Pathogens: Ancient pathogens are rarely preserved in a way that allows for direct analysis. The conditions required for preservation are often not met.
- Interpretation of Genetic Data: Genetic evidence can be difficult to interpret, and different methods can lead to varying conclusions about population history and the role of disease.
- Limited Historical Records: For many historical periods, reliable written records of disease outbreaks are scarce or nonexistent, leaving significant gaps in our understanding.
The Ongoing Search for Answers
The question of which disease, if any, nearly wiped out humanity continues to be a topic of intense scientific investigation. Advances in genetic sequencing, paleopathology, and other research methods are constantly improving our ability to understand past pandemics. Although pinpointing the specific agent responsible for a potential near-extinction event remains elusive, ongoing research provides valuable insights into the interplay between infectious diseases and human evolution. This knowledge is vital for understanding present-day disease dynamics and preparing for future challenges.
- Improved Sequencing Technologies: Next-generation sequencing technologies offer the potential to analyze ancient DNA with greater accuracy and detail.
- Interdisciplinary Collaboration: Collaborations between geneticists, archaeologists, anthropologists, and epidemiologists are essential for integrating different sources of evidence and building a more comprehensive picture.
- Modeling Disease Dynamics: Mathematical models can be used to simulate past disease outbreaks and investigate the potential impact of various factors on population size.
What disease has killed the most humans ever?
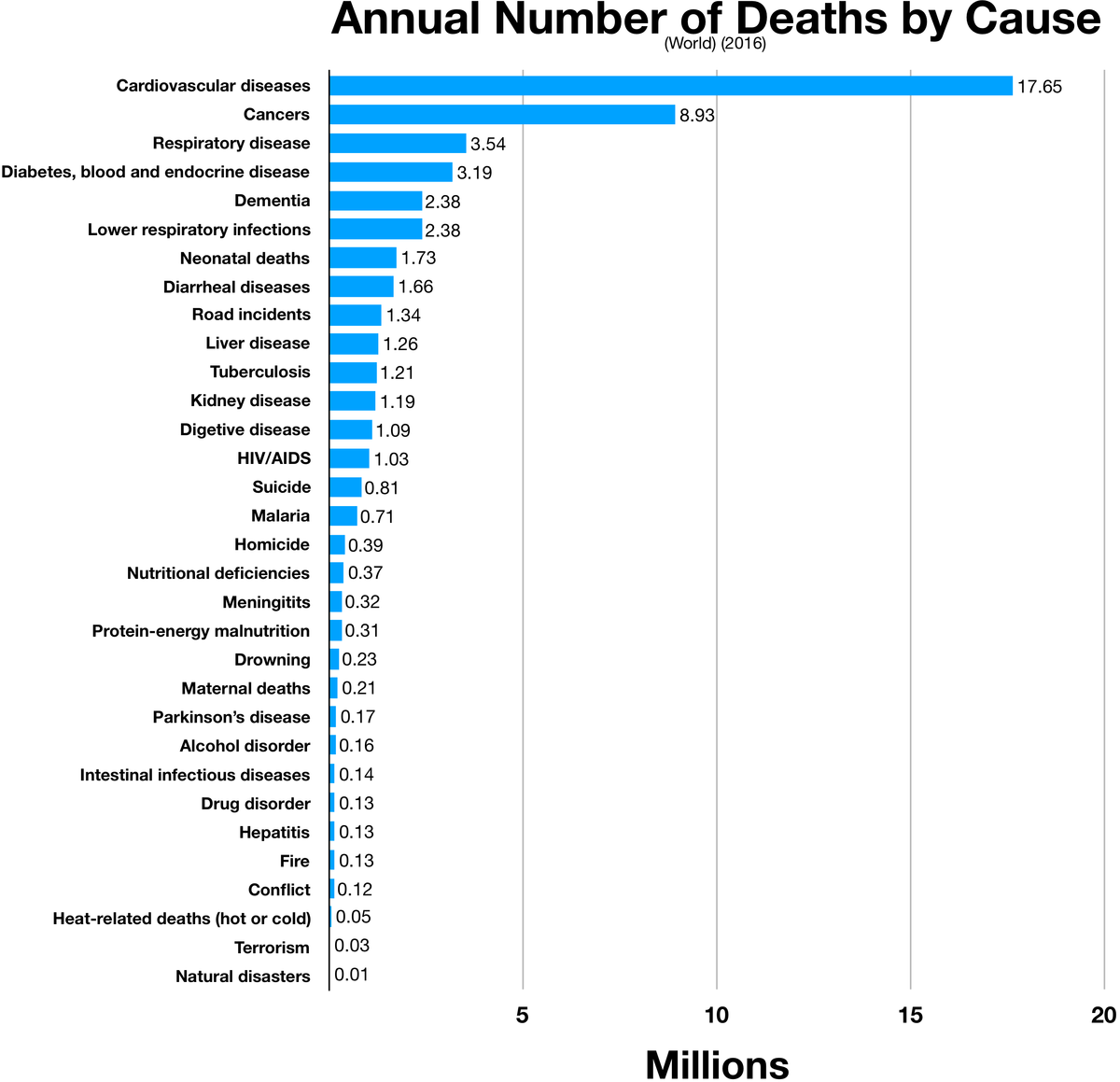
The disease that has killed the most humans ever is arguably smallpox. While precise figures are impossible to obtain due to historical record-keeping limitations, estimates suggest that smallpox has been responsible for hundreds of millions, possibly even over 500 million, deaths throughout history. Other contenders, such as the plague and malaria, have also caused immense devastation, but the sheer longevity and global reach of smallpox, prior to its eradication in 1980, makes it a strong candidate for the deadliest disease in human history. The highly contagious nature of smallpox and its devastating effects contributed significantly to its immense death toll.
Smallpox's Global Impact
Smallpox's impact was felt worldwide, regardless of socioeconomic status or geographic location. The disease's devastating effects were felt across continents, leaving a trail of death and suffering in its wake. Its high mortality rate, often exceeding 30% even with basic supportive care, and its ability to spread rapidly through populations, ensured it remained a leading cause of death for centuries. The lack of effective treatments further compounded the problem, leaving communities utterly vulnerable.
- Widespread Prevalence: Smallpox affected all continents, impacting diverse populations regardless of social standing.
- High Mortality Rate: A significant percentage of those infected succumbed to the disease.
- Lack of Effective Treatment: No treatments existed to combat the disease effectively until the development of a vaccine.
The Eradication of Smallpox
The successful eradication of smallpox in 1980 stands as a monumental achievement in global public health. This triumph demonstrated the power of concerted international effort, technological advancements (such as the development of an effective vaccine), and comprehensive public health strategies. The World Health Organization (WHO)'s dedicated campaign played a crucial role in the eventual elimination of the virus from the human population, a feat unprecedented in the history of infectious diseases.
- Global Collaboration: The eradication effort involved coordinated international collaboration on an unprecedented scale.
- Vaccine Development: The development of a safe and effective vaccine was critical to the eradication effort.
- WHO's Role: The WHO led and coordinated the global campaign to eradicate smallpox.
The Plague's Devastating Effects
The plague, particularly the bubonic plague, is another strong contender for the title of deadliest disease. Historically, plagues have resulted in devastating pandemics, wiping out significant portions of populations. The Black Death of the 14th century is a prime example, killing an estimated 30-60% of Europe's population. While less prevalent now, thanks to advancements in sanitation and medical treatment, the plague still poses a threat in some parts of the world.
- The Black Death: This devastating pandemic killed a significant portion of the European population.
- Recurring Outbreaks: Throughout history, the plague has caused numerous outbreaks and pandemics.
- Modern Treatments: Antibiotics are now effective in treating the plague, significantly reducing its mortality rate.
Malaria's Persistent Threat
Malaria, caused by the Plasmodium parasite transmitted through mosquito bites, remains a significant global health concern. While not as deadly in a single outbreak as smallpox or some plague pandemics, its persistent presence and immense cumulative death toll make it another strong contender for the deadliest disease ever. Millions of people are infected annually, resulting in hundreds of thousands of deaths, primarily among children in sub-Saharan Africa.
- High Prevalence in Sub-Saharan Africa: Malaria disproportionately affects populations in sub-Saharan Africa.
- High Child Mortality: Malaria is a major cause of death among young children in many parts of the world.
- Ongoing Research and Efforts: Considerable research is underway to develop effective vaccines and treatments for malaria.
Tuberculosis's Enduring Impact
Tuberculosis (TB), a bacterial infection that primarily affects the lungs, has a long and devastating history, killing millions throughout human history. While treatable with antibiotics, drug-resistant strains have emerged, posing a significant challenge to global public health efforts. The high prevalence of TB, coupled with the increasing emergence of drug resistance, continues to make it a major public health concern, leading to many deaths annually.
- Global Prevalence: TB remains a widespread infectious disease affecting millions globally.
- Drug Resistance: The emergence of drug-resistant strains of TB complicates treatment and control efforts.
- Treatment Challenges: TB treatment can be lengthy and complex, requiring strict adherence to medication regimens.
What disease kills within 24 hours?

There is no single disease that definitively kills within 24 hours for every individual. The timeframe for death from any illness depends heavily on a multitude of factors, including the individual's overall health, the severity of the infection or condition, the promptness and effectiveness of treatment, and the specific strain or virulence of the pathogen involved. However, some conditions can progress rapidly and lead to death within a day in severe cases. These often involve overwhelming infections or catastrophic organ failure.
Rapidly Progressive Infections
Certain bacterial infections, if untreated, can cause sepsis, a life-threatening condition characterized by widespread inflammation. This can lead to organ failure and death within hours to days. The speed of progression depends on factors such as the bacteria's virulence, the individual's immune response, and the presence of underlying health conditions. Examples include:
- Meningococcal septicemia: This is a severe form of meningococcal disease that can progress very quickly, causing widespread blood clotting and organ damage.
- Severe necrotizing fasciitis: Also known as flesh-eating bacteria, this aggressive infection rapidly destroys tissue and can overwhelm the body's defenses.
- Certain types of pneumonia: Severe pneumonia can lead to respiratory failure and death within a short timeframe, particularly in vulnerable populations such as the elderly or immunocompromised.
Cardiovascular Events
Sudden cardiac events, such as a massive myocardial infarction (heart attack) or a ruptured aortic aneurysm, can be fatal within a matter of hours. These events often involve a sudden blockage of blood flow to a vital organ, leading to rapid cellular death and organ failure. The survival rate depends heavily on immediate medical intervention.
- Acute myocardial infarction: A large blockage in a coronary artery can cause extensive heart muscle damage, quickly leading to cardiac arrest.
- Aortic dissection: A tear in the aorta, the body's main artery, can cause catastrophic internal bleeding and rapid death.
- Pulmonary embolism: A blood clot traveling to the lungs can block blood flow, leading to sudden respiratory failure and death.
Neurological Conditions
Certain neurological conditions can progress rapidly and cause death within a short time frame. These conditions often involve significant brain swelling or damage to vital brain structures. Rapid onset and severity are key features.
- Hemorrhagic stroke: Bleeding into the brain tissue causes swelling and pressure, damaging brain cells and quickly leading to death.
- Severe head trauma: Significant head injuries can cause brain swelling, bleeding, and damage to vital brain structures, potentially leading to death.
- Certain types of encephalitis: Inflammation of the brain, which can be caused by viral or bacterial infections, can rapidly cause brain damage and death.
Toxicological Emergencies
Exposure to certain toxins or poisons can lead to rapid death. The speed of onset and lethality depend on factors such as the type and amount of toxin ingested, inhaled, or absorbed. Immediate medical intervention is crucial.
- Cyanide poisoning: Cyanide is a potent toxin that prevents cells from using oxygen, leading to rapid cellular death and organ failure.
- Certain types of mushroom poisoning: Consumption of highly toxic mushrooms can cause rapid liver and kidney failure, and death.
- Drug overdose: Overdose on certain drugs, particularly opioids and other central nervous system depressants, can cause respiratory depression and death.
Severe Allergic Reactions
Anaphylaxis is a severe, life-threatening allergic reaction that can cause a rapid drop in blood pressure, airway constriction, and circulatory collapse. Prompt treatment with epinephrine is critical to prevent death.
- Insect stings (bees, wasps, hornets): These can trigger anaphylaxis in susceptible individuals.
- Food allergies (peanuts, shellfish, etc.): Severe allergic reactions to food can cause anaphylaxis.
- Medication allergies: Some medications can trigger severe allergic reactions, including anaphylaxis.
What disease did we almost eradicate?
The disease we almost eradicated is polio (poliomyelitis). Through a massive global vaccination campaign, the incidence of polio has been reduced by over 99% since 1988. While cases remain, the goal of eradication is still actively pursued by organizations like the Global Polio Eradication Initiative (GPEI).
The Success of the Polio Vaccine
The success in drastically reducing polio cases is largely attributed to the development and widespread use of the oral polio vaccine (OPV) and the inactivated polio vaccine (IPV). These vaccines have proven highly effective in preventing infection and transmission. The global coordination and commitment to mass vaccination campaigns were also crucial.
- OPV: Provides herd immunity, meaning even unvaccinated individuals are protected when a sufficient portion of the population is vaccinated.
- IPV: Offers highly effective individual protection, particularly important in areas with low vaccination coverage.
- Mass Vaccination Campaigns: These campaigns involved reaching remote and underserved populations, requiring significant logistical planning and resources.
Challenges in Eradicating Polio
Despite the significant progress, several challenges hinder the complete eradication of polio. Political instability and conflict in certain regions make vaccination campaigns difficult to implement effectively. Misinformation and vaccine hesitancy also pose significant obstacles, as do the challenges of reaching every child in every corner of the world. The virus itself is also particularly resilient.
- Accessibility: Reaching every child, especially in conflict zones or areas with poor infrastructure, remains a major hurdle.
- Vaccine Hesitancy: Mistrust of vaccines and misinformation campaigns can undermine vaccination efforts.
- Environmental Persistence: The poliovirus can persist in the environment, leading to potential outbreaks even in areas with high vaccination rates.
The Global Polio Eradication Initiative (GPEI)
The GPEI is a public-private partnership committed to eradicating polio worldwide. This initiative plays a vital role in coordinating global efforts, providing funding, and deploying resources to support national polio programs. Their work encompasses surveillance, vaccination campaigns, and research to improve vaccination strategies and address emerging challenges.
- Coordination: GPEI works with governments, NGOs, and international organizations to ensure a coordinated global response.
- Funding: GPEI secures and distributes funding for vaccination campaigns and other eradication efforts.
- Research & Development: The initiative supports research into improving polio vaccines and addressing challenges to eradication.
The Importance of Continued Efforts
Sustained commitment and investment in polio eradication are critical. Although the disease has been pushed to the brink of extinction, continued vigilance and ongoing vaccination programs are necessary to prevent the re-emergence of polio and achieve its complete eradication. Any complacency could lead to a resurgence, undoing decades of progress.
- Sustained Funding: Continued financial support is crucial for maintaining vaccination programs and surveillance efforts.
- Community Engagement: Building trust and addressing vaccine hesitancy through community engagement is essential.
- Improved Surveillance: Robust surveillance systems are necessary to detect and respond rapidly to any outbreaks.
Wild Poliovirus Type 2 Eradication
A significant milestone in the fight against polio was the eradication of wild poliovirus type 2 (WPV2) in 2015. This achievement demonstrated the effectiveness of global collaboration and the power of targeted vaccination campaigns. The eradication of WPV2 serves as a testament to what can be achieved when the international community unites in the face of a global health threat. Further work needs to focus on the eradication of the remaining two wild poliovirus types.
- Global Collaboration: The success of WPV2 eradication highlights the importance of international cooperation.
- Targeted Interventions: Effective eradication requires targeted strategies to reach high-risk populations.
- Lessons Learned: The strategies used to eradicate WPV2 can inform future efforts to eradicate the remaining wild poliovirus types.
What disease almost wiped out humanity?
There's no single disease that definitively "almost wiped out humanity," though several have come close to causing catastrophic population declines. The most significant candidate is likely the Black Death (also known as the bubonic plague), which ravaged Eurasia and North Africa in the mid-14th century. Estimates vary wildly, but it's thought that the plague killed somewhere between 30% and 60% of Europe's population, and possibly even more across its wider range. The sheer scale of mortality, coupled with the swiftness of its spread, made it a terrifying and devastating event with long-lasting societal impacts. While humanity didn't face extinction, the Black Death drastically altered the course of history, leading to significant social, economic, and religious upheaval. Other contenders for significant population reduction, though perhaps not quite reaching the level of the Black Death, include various pandemics of smallpox, influenza (particularly the 1918 Spanish flu pandemic), and other infectious diseases which frequently struck vulnerable populations particularly hard, especially before the development of effective medicine and sanitation. The severity of these events often depended on factors such as population density, hygiene levels, and the virulence of the disease strain. It's crucial to remember that human populations have been impacted repeatedly by devastating diseases throughout our history, and that the possibility of future pandemics remains a very real and significant concern.
What are the factors that determine a disease's potential to decimate humanity?
Several crucial factors contribute to a disease's potential for widespread devastation. A disease's lethality (its ability to cause death) is obviously paramount. A highly lethal disease with a high case-fatality rate will inflict more severe damage than a milder one. However, lethality alone doesn't tell the whole story. The transmission rate is just as, if not more, important. Diseases that spread easily through various means (airborne, through contact, etc.) are far more dangerous than those confined to specific vectors or transmission methods. This is why highly contagious diseases like influenza and measles historically caused widespread epidemics. The existence of effective treatments or vaccines is another critical factor; diseases for which there are effective treatments or prevention methods are far less likely to cause widespread mortality. The pre-existing health status of the population is also significant: a population already weakened by malnutrition, poverty, or other diseases is far more vulnerable to new outbreaks. Finally, the ability of a government or organization to respond effectively to an outbreak through measures such as quarantine, public health initiatives and resource allocation significantly influences the final impact. The interplay of all these factors determines a disease's potential to drastically reduce or even threaten the human population.
Could a disease ever completely wipe out humanity?
While a disease completely wiping out humanity is considered highly unlikely, it's not impossible. The scenario is typically explored in science fiction, but the possibility is informed by scientific understanding. A pathogen with several extremely unfavorable characteristics, such as extremely high lethality and transmissibility, coupled with a lack of any effective treatment or prevention, could theoretically cause catastrophic population loss. Moreover, a combination of factors, such as a particularly virulent disease affecting a highly susceptible population during a period of global instability or other crisis, could exacerbate the effects. However, humanity's biological diversity works to our advantage. Genetic variation within the human population means that some individuals might be naturally resistant to a particular disease, allowing for survival and the possibility of future immunity. Moreover, human ingenuity, the capacity for rapid scientific advancements (such as vaccine development) and the ability to adapt and cooperate remain critical factors mitigating the potential for complete extinction. The likelihood of a total human extinction via a single disease is, however, considered extremely low compared to other potential existential threats.
What are we doing to prevent future pandemics?
The prevention of future pandemics is a complex and multifaceted endeavor requiring global cooperation and significant resources. Strengthening global surveillance systems to detect and monitor outbreaks quickly and effectively is a primary focus. This includes enhancing laboratory capacity for disease identification and sharing information promptly between nations. Investing in research and development for new vaccines and treatments is crucial. This includes creating stockpiles of essential medical supplies and developing rapid response strategies for emerging diseases. Improving public health infrastructure globally is also paramount. This involves strengthening healthcare systems in vulnerable regions, promoting sanitation and hygiene, and improving access to healthcare for all populations. Increased efforts in One Health initiatives, which recognize the interconnectedness of human, animal, and environmental health, are essential. This approach involves addressing factors that increase the risk of zoonotic disease transmission (diseases that jump from animals to humans). Finally, promoting international cooperation and information sharing is vital for a coordinated global response to any potential pandemic. This requires strong political will and collaborative efforts from governments, international organizations, and scientific communities worldwide. The threat of future pandemics remains a significant challenge, but proactive measures can significantly reduce the risk of another catastrophic event.
Deja una respuesta