What disease has no cure

In the tapestry of life, health holds a precious thread, yet disease can unravel its delicate fibers. While medical advancements have woven cures for countless ailments, there remain strands of despair, enigmas that elude our grasp. Among these medical mysteries lies a formidable foe, a disease that has cast a long shadow over humanity, defying our best efforts to vanquish it: a disease with no cure.
Diseases with No Known Cure
There is no single disease that definitively has "no cure." The term "cure" itself is complex and can mean different things depending on the context. Some diseases might lack a cure that completely eradicates the disease, but treatments can effectively manage symptoms and improve quality of life significantly. Others might have cures for certain manifestations but not others. The landscape of medical science is constantly evolving, with new treatments and potential cures being researched and developed all the time. However, certain diseases currently lack a cure that leads to complete eradication or remission.
What Defines a "Cure"?
The definition of a "cure" is fluid and depends on the specific disease. For some conditions, like bacterial infections, a cure might mean the complete elimination of the infectious agent. For chronic diseases like HIV or type 1 diabetes, a "cure" could imply achieving sustained remission without the need for ongoing treatment to manage the disease's symptoms. Often, a more realistic goal than a complete cure is effective disease management to improve the patient's quality of life and extend their lifespan.
Examples of Diseases with No Known Cure: Huntington's Disease
Huntington's disease (HD) is a neurodegenerative genetic disorder that causes the progressive breakdown of nerve cells in the brain. Currently, there is no cure for HD. Treatment focuses on managing symptoms, such as chorea (uncontrollable movements), cognitive decline, and psychiatric symptoms. Research is ongoing, exploring potential therapies like gene editing and neuroprotective agents.
Examples of Diseases with No Known Cure: Alzheimer's Disease
Alzheimer's disease is a progressive neurodegenerative disorder that leads to memory loss and cognitive decline. There's currently no cure for Alzheimer's, but several medications can temporarily slow the progression of symptoms. Research is focusing on identifying the underlying causes of the disease and developing therapies that can prevent or reverse its progression.
Examples of Diseases with No Known Cure: Certain Types of Cancer
While significant progress has been made in cancer treatment, some types of cancer remain incurable. The success of cancer treatment depends on various factors, including the type and stage of cancer, the patient's overall health, and the response to treatment. While some cancers can be treated successfully, others may have no definitive cure, although therapies can prolong life and improve the patient's quality of life. Research continues to focus on developing more targeted and effective cancer therapies.
Examples of Diseases with No Known Cure: Prion Diseases
Prion diseases, such as Creutzfeldt-Jakob disease (CJD), are fatal neurodegenerative disorders caused by misfolded proteins. These diseases are notoriously difficult to treat, and currently there are no known cures. Research is ongoing to understand the mechanisms of prion diseases and to develop potential therapeutic strategies.
| Disease | Current Status | Treatment Focus |
|---|---|---|
| Huntington's Disease | No cure; research ongoing | Symptom management |
| Alzheimer's Disease | No cure; research ongoing | Slowing disease progression |
| Certain Cancers | Curable in some cases; incurable in others | Targeted therapies, surgery, chemotherapy, radiation |
| Prion Diseases | No cure | Supportive care |
| Type 1 Diabetes | No cure; research ongoing | Insulin therapy, blood sugar management |
https://youtube.com/watch?v=CFagZYXlfcM%26t%3D258s
What rare disease has no cure?

There are many rare diseases with no known cure. The specific disease that qualifies as "rare" varies by region and definition (often involving prevalence rates below a certain threshold). It's important to understand that research is constantly ongoing, and what is considered incurable today may have treatments or cures in the future. Some examples of rare diseases currently lacking a cure include progeria, Batten disease, and Huntington's disease, among countless others. The lack of a cure often stems from the complexity of the disease's underlying mechanisms, limited research funding, and the small patient populations making clinical trials challenging.
Rare Diseases: Challenges in Research and Treatment
One of the biggest hurdles in finding cures for rare diseases is the limited research funding available. Because these conditions affect relatively few people, pharmaceutical companies are often less incentivized to invest in expensive research and development. This lack of funding translates directly into fewer clinical trials and slower progress in understanding the disease's pathogenesis and potential therapeutic targets. This also impacts the development of diagnostic tools, leading to further delays in treatment.
- Insufficient funding leads to limited research opportunities.
- Small patient populations make clinical trials difficult to conduct.
- Lack of awareness hinders recruitment for research studies.
Progeria: A Premature Aging Disease
Progeria (Hutchinson-Gilford progeria syndrome) is a genetic disorder causing premature aging in children. Affected individuals experience rapid aging, typically dying in their teens or early twenties. There is no cure for progeria, and current treatments focus on managing symptoms and improving quality of life. While research has yielded some promising avenues, such as lonafarnib, a farnesyltransferase inhibitor, which shows some efficacy in slowing the progression of the disease, it is not a cure.
- Accelerated aging is the hallmark of progeria.
- Genetic mutation in the LMNA gene is the underlying cause.
- Treatment focuses on symptom management, not a cure.
Batten Disease: A Degenerative Neurological Disorder
Batten disease, or neuronal ceroid lipofuscinoses (NCLs), is a group of rare, inherited neurodegenerative disorders that primarily affect children. The diseases cause progressive vision loss, seizures, loss of motor skills, and cognitive decline. There is no cure for Batten disease, and treatments are largely supportive, aimed at managing symptoms and improving quality of life. Research focuses on gene therapy and other approaches to address the underlying genetic defects.
- Progressive neurodegeneration leads to severe disability.
- Multiple subtypes exist, each with varying severity and symptoms.
- Current treatments are palliative, focusing on symptom management.
Huntington's Disease: A Neurodegenerative Disorder
Huntington's disease is a progressive, inherited neurodegenerative disorder affecting the brain. The disease typically begins in adulthood and causes uncontrolled movements, cognitive decline, and psychiatric problems. Currently, there is no cure for Huntington's disease. While treatments are available to manage symptoms, they do not halt or reverse the progression of the disease. Ongoing research explores various avenues, including gene silencing therapies, to potentially slow or prevent disease progression.
- Progressive neurological damage leads to irreversible disability.
- Autosomal dominant inheritance means a single copy of the mutated gene causes the disease.
- Research focuses on gene therapy and other disease-modifying approaches.
Rare Diseases: The Importance of Continued Research
The absence of a cure for many rare diseases underscores the critical need for continued research and investment in this area. Advances in genetics, genomics, and other fields hold immense promise for developing new treatments and ultimately cures for these debilitating conditions. Collaborative efforts between researchers, clinicians, patient advocacy groups, and funding agencies are essential to accelerate progress and improve the lives of individuals affected by rare diseases. Increased awareness and funding are crucial for future breakthroughs.
- Continued research is essential for developing new treatments and cures.
- Collaboration among stakeholders is crucial for progress.
- Increased funding and awareness are vital to support research efforts.
What's the worst chronic disease?
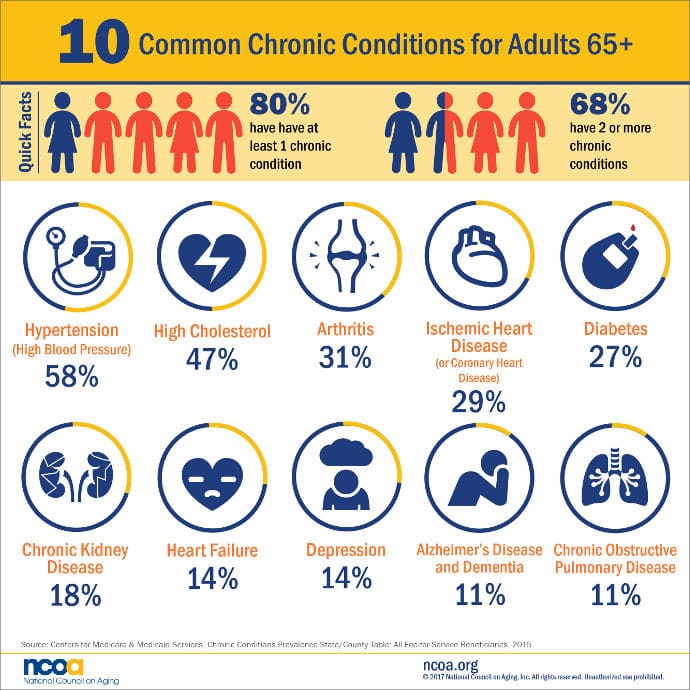
There is no single "worst" chronic disease. The impact of a chronic disease depends heavily on several factors, including the individual's specific circumstances, the severity of the disease, available treatments, and access to healthcare. Some diseases cause significantly more disability and death globally than others, but the subjective experience of "worst" is highly personal. Different diseases affect different people in profoundly different ways.
Defining "Worst": Subjectivity and Individual Experience
The question of the "worst" chronic disease is inherently subjective. What constitutes "worst" varies dramatically depending on individual factors such as age, overall health, support systems, and access to medical care. A disease might be considered "worse" for one person due to its impact on their quality of life, while another might prioritize life expectancy. There's no objective scale to measure the overall suffering caused by different conditions. For instance, a debilitating autoimmune disease might be deemed "worse" by one individual than a chronic respiratory condition by another, despite potentially different mortality rates.
- Severity of symptoms: Pain, fatigue, and cognitive impairment can vary greatly.
- Impact on daily life: Some diseases severely limit activities of daily living, while others allow for a more normal lifestyle.
- Treatment burden: The intensity and invasiveness of treatments significantly affect quality of life.
Global Burden of Disease: Considering Mortality and Morbidity
From a public health perspective, assessing the "worst" chronic disease often involves examining the global burden of disease. This approach focuses on metrics such as mortality (death rates) and morbidity (illness rates). Cardiovascular diseases, including heart disease and stroke, consistently rank among the leading causes of death worldwide. Similarly, cancer encompasses a broad range of diseases with high mortality rates and significant long-term consequences. These diseases, due to their prevalence and impact on global health, might be considered contenders for "worst" based on these metrics. However, this analysis lacks the nuance of individual experiences.
- Cardiovascular disease: High mortality rates and significant disability.
- Cancer: Diverse range of cancers, many with high mortality and significant treatment side effects.
- Chronic respiratory diseases: Significant morbidity, impacting quality of life and longevity.
Impact on Quality of Life: Beyond Mortality Rates
The impact of a chronic disease extends far beyond mortality. Quality of life is significantly affected by the degree of disability, pain, and emotional distress a condition inflicts. Diseases such as Alzheimer's disease and other forms of dementia impose immense burdens on both patients and their caregivers. The progressive nature of cognitive decline and loss of independence dramatically reduces quality of life, although the mortality rate itself might not be as high as some other conditions. Similarly, chronic pain conditions can severely impact a person’s ability to work, socialize, and enjoy life, even without posing an immediate threat to life.
- Neurodegenerative diseases: Significant cognitive and functional decline.
- Chronic pain conditions: Debilitating pain impacting daily activities.
- Mental health disorders: Significant impact on overall well-being and daily functioning.
Cost of Care: Economic and Societal Burden
The economic burden of chronic diseases is substantial, both for individuals and healthcare systems. The cost of medications, treatments, long-term care, and lost productivity due to illness contribute significantly to healthcare expenditures. Diseases requiring extensive and long-term care, such as advanced cancer, multiple sclerosis, and end-stage renal disease, place a considerable strain on resources. This economic aspect contributes to the discussion of which diseases are "worst" from a societal perspective, as it impacts healthcare systems and resource allocation.
- High-cost treatments: Many chronic diseases require expensive medications and therapies.
- Long-term care needs: Many chronic conditions require significant long-term care, increasing costs.
- Lost productivity: Illness and disability resulting from chronic diseases reduce workforce participation.
Rare Diseases: The Unseen Burden
While common chronic diseases like heart disease and cancer receive significant research funding and public attention, a vast number of rare diseases inflict substantial suffering on affected individuals and families. These conditions often lack effective treatments and are characterized by significant physical and emotional challenges. The rarity of these diseases makes it difficult to collect comprehensive data on their impact, but the experience of those living with them is often profoundly challenging. The lack of research funding and awareness often exacerbates their impact, highlighting the complex challenges in determining the “worst” chronic disease.
- Lack of effective treatments: Many rare diseases have limited or no effective treatments.
- Diagnostic challenges: Diagnosing rare diseases can be difficult and time-consuming.
- Limited research funding: Less research funding for rare diseases compared to common conditions.
Which disease agent has no cure?
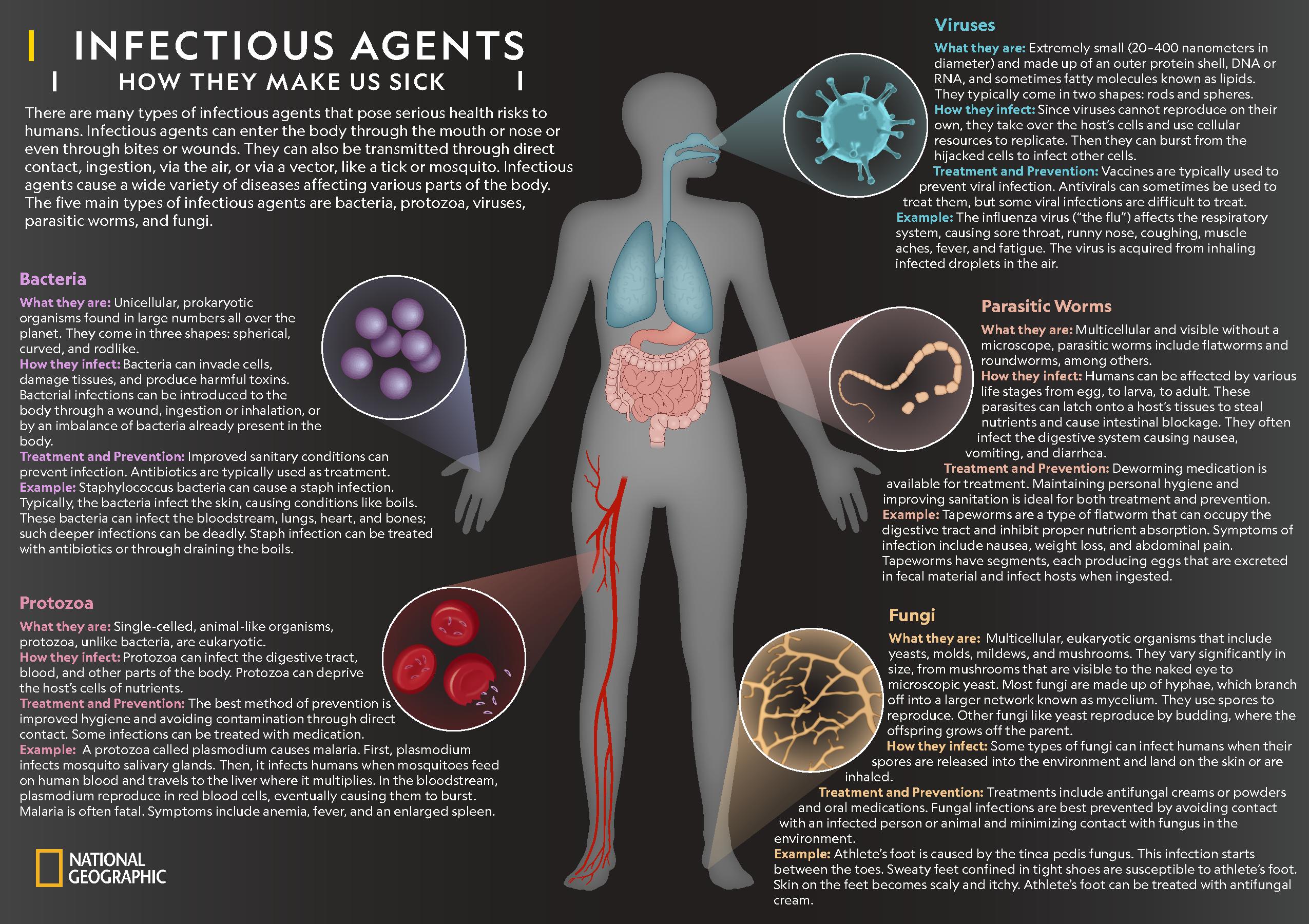
There is no single disease agent that definitively has nocure. Many diseases, particularly those caused by prions, certain viruses, and some genetic conditions, currently lack cures. However, "no cure" often means there's no treatment that completely eradicates the disease agent or restores the body to its pre-disease state. Instead, treatments focus on managing symptoms, slowing disease progression, or improving quality of life. The landscape of medicine is constantly evolving, with ongoing research aiming to find cures for diseases currently considered incurable. Therefore, stating that a specific agent has absolutely nocure is an oversimplification.
Prion Diseases: An Incurable Class
Prion diseases, such as Creutzfeldt-Jakob disease (CJD) and bovine spongiform encephalopathy (BSE, or "mad cow disease"), are caused by misfolded proteins (prions) that accumulate in the brain, leading to fatal neurodegenerative disorders. Currently, there is no effective cure for prion diseases. Treatments focus on managing symptoms and providing palliative care to improve the patient's quality of life.
- Lack of effective treatments: The unique nature of prions, their resistance to degradation, and their ability to induce misfolding in other proteins make them difficult targets for therapeutic interventions.
- Progressive neurological damage: The damage caused by prions in the brain is irreversible and progressive, leading to significant neurological dysfunction and ultimately death.
- Diagnostic challenges: Diagnosing prion diseases can be challenging, often requiring post-mortem analysis, which limits the ability to initiate timely intervention.
HIV/AIDS: Managing, Not Curing
Human immunodeficiency virus (HIV), which causes acquired immunodeficiency syndrome (AIDS), is a retrovirus that attacks the immune system. While there is no cure for HIV, antiretroviral therapy (ART) can effectively suppress viral replication, preventing disease progression and extending lifespan. However, HIV remains latent within the body, and discontinuation of ART leads to viral rebound.
- Viral latency: HIV integrates its genetic material into the host's DNA, forming latent reservoirs that are difficult to eliminate with current therapies.
- Evolution of drug resistance: HIV is prone to mutations, leading to the development of drug-resistant strains that can compromise the effectiveness of ART.
- Challenges in eradication: Completely eradicating HIV from the body requires overcoming significant immunological and virological hurdles.
Certain Cancers: Treatment-Dependent Outcomes
Many cancers are currently incurable, although significant advances in treatment have improved survival rates and quality of life for many patients. The term "incurable" in this context means that the cancer cannot be completely eradicated, and the disease may eventually recur. Treatments aim to control cancer growth, prevent metastasis, and extend life expectancy.
- Tumor heterogeneity: Cancer cells are highly diverse, making it difficult to develop treatments that target all cancerous cells effectively.
- Metastasis: The spread of cancer cells to other parts of the body makes complete eradication challenging.
- Development of drug resistance: Cancer cells can develop resistance to chemotherapy and other treatments, limiting the effectiveness of therapy.
Genetic Diseases: No Universal Cure
Many genetic disorders, caused by mutations in an individual's DNA, lack a cure as the underlying genetic defect is permanent. Treatments may focus on managing symptoms, providing supportive care, or gene therapy which is still in its early stages of development for most diseases.
- Permanent genetic alteration: The genetic basis of many disorders makes it challenging to reverse the underlying cause.
- Pleiotropy: Many genes have multiple effects on the body, making it challenging to target a single gene without causing unwanted side effects.
- Limited therapeutic options: Treatment options for genetic disorders are often limited, and many disorders lack effective therapies.
Neurodegenerative Diseases: Slowing Progression, Not Curing
Neurodegenerative diseases, such as Alzheimer's disease and Parkinson's disease, involve the progressive loss of structure or function of neurons. While there is no cure for most neurodegenerative diseases, treatments are aimed at slowing disease progression and managing symptoms. Research continues to explore potential therapies, but a cure remains elusive.
- Complex pathogenesis: The causes and mechanisms of neurodegenerative diseases are complex and not fully understood, making it difficult to develop effective therapies.
- Irreversible neuronal damage: The damage caused by neurodegenerative diseases is often irreversible, leading to progressive decline in neurological function.
- Challenges in drug delivery: Delivering drugs effectively to the brain to target affected neurons can be challenging.
What is an incurable disease called?
An incurable disease is called an incurable disease, or sometimes a terminal illness if it is expected to lead to death. There isn't a single, universally accepted alternative term. The specific terminology used often depends on the context, the specific disease, and the stage of the disease's progression. Sometimes, the focus is on the specific symptoms or the affected organ system (e.g., "neurodegenerative disease"). Other times, the term might emphasize the lack of effective treatment (e.g., "untreatable condition").
Terminology Used for Incurable Diseases
The language surrounding incurable diseases is carefully chosen, reflecting the complexity of the situation. Sometimes, terms like "chronic" are used, indicating a long-lasting condition but not necessarily fatal. However, many chronic conditions lack a cure. The use of "terminal" is often reserved for illnesses with a clearly defined end stage leading to death, but even this is nuanced, as the progression can be unpredictable. Precise language is crucial for patient understanding and medical communication.
- Chronic: A long-lasting condition that may or may not be fatal.
- Terminal: A disease expected to lead to death.
- Untreatable: Emphasizes the lack of effective treatment options.
Examples of Incurable Diseases
Many diseases are considered incurable, though research continues to improve management and quality of life. Some prominent examples include certain types of cancer, Alzheimer's disease, Huntington's disease, and HIV/AIDS. The lack of a cure doesn't always equate to a lack of treatment. Management often focuses on slowing progression, managing symptoms, and improving the patient's overall well-being.
- Cancer: Many types of cancer are incurable, though treatments can significantly extend life and improve quality of life.
- Alzheimer's Disease: A progressive neurodegenerative disease with no known cure.
- HIV/AIDS: While not curable, effective antiretroviral therapy (ART) can manage the disease and prevent transmission.
The Impact of "Incurable" on Patients and Families
The diagnosis of an incurable disease can have a profound impact on patients and their families. It triggers a wide range of emotions, including grief, fear, anxiety, and uncertainty. Open and honest communication between medical professionals, patients, and families is essential. The focus shifts from cure to effective management, symptom control, and palliative care if necessary.
- Grief and Loss: Anticipatory grief is common.
- Anxiety and Fear: Uncertainty about the future can be overwhelming.
- Emotional Support: Strong support systems are crucial for coping.
Research and Hope for Incurable Diseases
While many diseases are currently considered incurable, ongoing medical research offers hope. Scientists constantly strive to understand the underlying mechanisms of disease and develop new treatments. Advances in gene therapy, immunotherapy, and personalized medicine provide new avenues for potentially curing or effectively managing once-incurable conditions.
- Gene Therapy: Aims to correct genetic defects underlying some diseases.
- Immunotherapy: Harnessing the power of the immune system to fight disease.
- Personalized Medicine: Tailoring treatments to individual patients' genetic makeup.
Ethical and Social Considerations
The concept of "incurable" raises important ethical and social questions. Access to palliative care, end-of-life decisions, and resource allocation in the healthcare system are all complex issues. Discussions about advance directives, living wills, and informed consent become increasingly critical.
- Access to Palliative Care: Ensuring everyone has access to pain management and end-of-life care.
- End-of-Life Decisions: Supporting patients and families in making informed choices.
- Resource Allocation: Fair and equitable distribution of healthcare resources.
What diseases have no cure?
There is no single, simple answer to this question, as the concept of a "cure" can be nuanced. Some diseases, like HIV, are currently incurable in the sense that the virus cannot be completely eradicated from the body. However, with effective antiretroviral therapy (ART), the virus can be suppressed to undetectable levels, preventing disease progression and transmission. This means individuals living with HIV can lead long and healthy lives. Similarly, chronic diseases like type 1 diabetes and certain forms of heart disease don't have a "cure" in the sense of reversing the underlying condition. However, effective management strategies exist, such as insulin therapy for diabetes and lifestyle modifications and medication for heart disease, significantly improving quality of life and lifespan. The research landscape is constantly evolving, with ongoing efforts to develop more effective treatments and potential cures for conditions that are currently considered incurable. Ultimately, it's important to distinguish between diseases lacking a cure and diseases that are effectively manageable and treatable, leading to a high quality of life.
Are there any genetic diseases with no cure?
Many genetic disorders currently lack a cure. These conditions are caused by mutations in an individual's genes, leading to a variety of health problems. Some examples include Huntington's disease, cystic fibrosis, and sickle cell anemia. While there is no cure for these conditions, significant progress is being made in gene therapy, offering potential avenues for future treatments. Gene therapy aims to modify or replace faulty genes to alleviate the symptoms or underlying cause of the disease. For some genetic disorders, symptomatic treatments are available to manage symptoms and improve quality of life. For example, individuals with cystic fibrosis can benefit from therapies to clear mucus from their lungs and prevent infections. The development of gene editing technologies, such as CRISPR, is revolutionizing genetic disease research and holds immense promise for creating cures in the future. However, the complexity of genetic disorders and the ethical implications surrounding gene editing require careful consideration.
What about neurodegenerative diseases? Do they have cures?
Unfortunately, most neurodegenerative diseases, such as Alzheimer's disease and Parkinson's disease, currently lack a cure. These conditions involve the progressive degeneration of nerve cells in the brain, leading to a decline in cognitive function, motor skills, and other neurological abilities. While there are treatments available to manage symptoms and slow the progression of the disease, these do not reverse the underlying damage to the brain. Research into the causes and mechanisms of neurodegenerative diseases is ongoing, with numerous research teams exploring various therapeutic strategies. This includes developing drugs that target the underlying disease processes, such as amyloid plaques in Alzheimer's disease, as well as exploring potential therapeutic interventions such as gene therapy and stem cell transplantation. However, the complexity of these diseases, and the challenges in developing effective therapies that cross the blood-brain barrier, make the search for a cure incredibly difficult and time-consuming.
Is it possible to develop a cure for all diseases?
While the ultimate goal of medical research is to find cures for all diseases, it's currently unrealistic to suggest this will happen universally. The diversity of diseases and their complexities present significant challenges. Some diseases are caused by simple genetic mutations that may be easier to target with gene therapy or other precision medicine approaches. However, many diseases result from complex interactions between genes, environment, and lifestyle factors, making it significantly harder to identify effective therapeutic targets. Additionally, emerging infectious diseases, such as novel viruses and antibiotic-resistant bacteria, constantly pose new challenges that necessitate ongoing research and development efforts. Nevertheless, scientific advancements continuously improve our understanding of disease mechanisms, leading to the development of new treatments and therapies for conditions that were previously incurable. The path towards cures is a continuous journey, characterized by ongoing research and innovation.
Deja una respuesta