What is the hardest chronic illness to live with

In the realm of chronic illnesses, where relentless battles are fought day after day, the question of which ailment stands as the most formidable opponent has plagued medical professionals and patients alike. While each condition carries its own unique set of challenges, the arduous path of those afflicted with the most severe and debilitating chronic illnesses can be unfathomably arduous. In this article, we delve into the depths of the most difficult chronic illness to live with, examining its insidious symptoms, relentless nature, and profound impact on the lives of those who face it bravely.
What Makes a Chronic Illness "The Hardest"?
There's no single answer to the question "What is the hardest chronic illness to live with?" The experience of chronic illness is deeply personal and subjective. What one person finds debilitating, another might manage relatively well. Severity, symptoms, available treatments, support systems, and individual coping mechanisms all play a significant role. Instead of ranking illnesses, it's more helpful to understand the factors that contribute to the immense challenges faced by individuals with chronic conditions. The "hardest" illness is often the one that most profoundly impacts a person's physical, mental, emotional, and social well-being.
The Impact of Pain
Chronic pain is a defining feature of many debilitating illnesses. Conditions like fibromyalgia, complex regional pain syndrome (CRPS), and endometriosis can cause unrelenting, often intractable pain that significantly interferes with daily life. This pain is not only physically debilitating but can also lead to depression, anxiety, and social isolation. The constant struggle to manage pain, combined with the lack of effective treatment for some, creates a significant burden for those affected.
Cognitive Impairment and "Brain Fog"
Many chronic illnesses, including multiple sclerosis (MS), lupus, Lyme disease, and long COVID, cause significant cognitive impairment often referred to as "brain fog." This can manifest as difficulty with memory, concentration, processing information, and decision-making. The impact on daily life is substantial, affecting work, relationships, and personal well-being. The invisible nature of cognitive impairment can also lead to feelings of invalidation and frustration, as symptoms are often difficult for others to understand.
The Burden of Unpredictable Symptoms
The unpredictability of symptoms is a major challenge for many people with chronic illnesses. Conditions like Crohn's disease, ulcerative colitis, and cystic fibrosis can involve unpredictable flare-ups that require immediate medical attention and significantly impact quality of life. This unpredictability makes planning and maintaining a sense of normalcy extremely difficult. The constant uncertainty can lead to anxiety and a sense of loss of control.
The Social and Economic Impact
Chronic illness often has a profound impact on a person's social and economic life. The need for frequent medical appointments, treatments, and potential periods of disability can lead to financial strain. Social isolation is also common, as individuals may struggle to participate in activities they once enjoyed. The stigma surrounding certain illnesses can further complicate matters, leading to feelings of shame and isolation.
Impact on Mental Health
Mental health challenges are frequently associated with chronic illness. Depression, anxiety, and post-traumatic stress disorder (PTSD) are common co-occurring conditions. The constant struggle with physical symptoms, uncertainty about the future, and social isolation can take a significant toll on mental well-being. Access to adequate mental healthcare is crucial, but often difficult to obtain.
| Chronic Illness | Key Challenges |
|---|---|
| Fibromyalgia | Intractable pain, fatigue, sleep disturbances, cognitive impairment |
| Multiple Sclerosis (MS) | Neurological dysfunction, cognitive impairment, fatigue, unpredictable symptoms |
| Crohn's Disease | Gastrointestinal pain, inflammation, unpredictable flare-ups, nutritional deficiencies |
| Lupus | Autoimmune inflammation affecting multiple organs, fatigue, pain, cognitive impairment |
| Cystic Fibrosis | Respiratory complications, pancreatic insufficiency, frequent infections, need for extensive medical care |
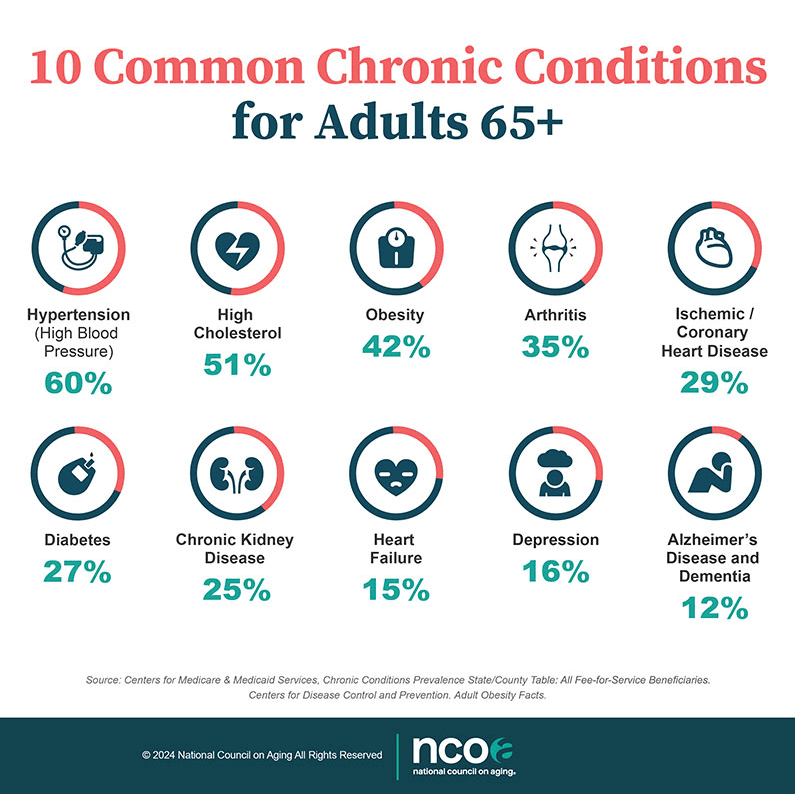
What is the deadliest chronic disease?

Determining the single "deadliest" chronic disease is difficult because mortality rates vary significantly by region, age group, and access to healthcare. However, ischaemic heart disease (IHD), often referred to as coronary artery disease, consistently ranks among the leading causes of death globally. While other chronic diseases like cancer claim many lives, IHD's pervasive nature and high mortality rate make it a strong contender for the deadliest.
What is Ischemic Heart Disease (IHD)?
Ischemic heart disease occurs when the blood flow to the heart muscle is reduced, primarily due to the buildup of plaque in the coronary arteries. This plaque, composed of cholesterol, fat, and other substances, narrows the arteries, restricting the oxygen-rich blood supply to the heart. The reduced blood flow can lead to chest pain (angina), shortness of breath, and ultimately, a heart attack (myocardial infarction) or heart failure. The severity and impact of IHD vary greatly depending on several factors.
- Severity of Artery Blockage: The extent to which the arteries are narrowed directly affects the blood flow to the heart.
- Location of Blockage: Blockages in major arteries have more significant consequences than blockages in smaller arteries.
- Individual Risk Factors: Pre-existing conditions such as high blood pressure, high cholesterol, diabetes, and smoking can exacerbate the risk and severity of IHD.
Risk Factors for Ischemic Heart Disease
Many factors contribute to the development of IHD. These risk factors can be broadly categorized as modifiable (those that can be changed through lifestyle choices) and non-modifiable (those that cannot be altered). Understanding and managing these factors is crucial in preventing or mitigating the severity of IHD.
- Modifiable Risk Factors: High blood pressure, high cholesterol, smoking, physical inactivity, unhealthy diet, obesity, and excessive alcohol consumption.
- Non-Modifiable Risk Factors: Age, family history of heart disease, and gender (men are at higher risk than women).
- Other Contributing Factors: Stress, diabetes, and certain medical conditions can also increase the risk of IHD.
Symptoms of Ischemic Heart Disease
The symptoms of IHD can vary widely, ranging from mild discomfort to severe chest pain. Recognizing these symptoms is crucial for seeking timely medical attention. While some individuals experience classic symptoms, others may exhibit less obvious signs.
- Chest Pain (Angina): Often described as pressure, tightness, squeezing, or pain in the chest, sometimes radiating to the jaw, neck, arms, or back.
- Shortness of Breath: Difficulty breathing, especially during physical exertion.
- Other Symptoms: Lightheadedness, dizziness, nausea, sweating, fatigue, and heart palpitations.
Treatment and Prevention of Ischemic Heart Disease
Treatment for IHD focuses on improving blood flow to the heart and managing risk factors. Preventive measures emphasize lifestyle changes and medical interventions to reduce the risk of developing IHD.
- Medications: Aspirin, statins (to lower cholesterol), beta-blockers (to slow heart rate), ACE inhibitors (to lower blood pressure).
- Procedures: Angioplasty (to open blocked arteries), coronary artery bypass grafting (CABG) surgery (to bypass blocked arteries).
- Lifestyle Changes: Adopting a healthy diet, increasing physical activity, quitting smoking, managing stress, and maintaining a healthy weight.
Global Impact and Mortality
Ischemic heart disease represents a significant global health burden, contributing to a substantial number of deaths worldwide each year. The impact of IHD varies across different regions and populations, influenced by factors such as access to healthcare, socioeconomic status, and lifestyle habits. Reducing its global mortality requires concerted efforts in prevention, early detection, and effective treatment.
- High Mortality Rates: IHD remains a leading cause of death globally, accounting for a substantial percentage of cardiovascular-related fatalities.
- Socioeconomic Disparities: Access to healthcare and preventive measures often varies, leading to disparities in IHD incidence and mortality rates across different populations.
- Public Health Initiatives: Global initiatives focusing on promoting heart-healthy lifestyles and improving access to healthcare are crucial in addressing the global impact of IHD.
What is the most feared health condition?

There isn't a single definitive answer to what the mostfeared health condition is, as fear is subjective and varies greatly depending on individual experiences, cultural background, and personal perspectives. However, cancer consistently ranks highly in surveys and studies exploring health anxieties. This is likely due to a confluence of factors including its high prevalence, often aggressive nature, complex treatments, and significant impact on quality of life and life expectancy. Other conditions like dementia and heart disease also frequently appear near the top of these lists, reflecting different facets of fear related to cognitive decline and sudden death, respectively. The fear isn't just about the condition itself but also includes the implications: the impact on family, financial burden, and loss of independence.
Fear of Cancer
Cancer is often cited as the most feared health condition due to its high mortality rate and the often grueling and invasive treatments required. The potential for long-term suffering, disfigurement, and the emotional toll on patients and their families contribute to its widespread fear. The sheer variety of cancers, each with its unique challenges and prognosis, adds another layer of complexity to the anxiety.
- High mortality rates: Many types of cancer have high mortality rates, meaning a significant chance of death.
- Aggressive treatments: Chemotherapy, radiation, and surgery can be physically and emotionally draining.
- Impact on quality of life: Cancer and its treatments can significantly impair a person's ability to live a normal life.
Fear of Dementia
Dementia, particularly Alzheimer's disease, is another leading contender for the most feared condition. The fear stems from the progressive and irreversible loss of cognitive function, leading to a decline in memory, personality, and eventually, basic abilities like self-care. Witnessing a loved one suffer from dementia is devastating, adding to the widespread fear surrounding this condition. The uncertainty surrounding its onset and progression, and the lack of a cure, significantly contribute to anxiety.
- Progressive cognitive decline: Dementia leads to a gradual loss of memory, thinking abilities, and judgment.
- Loss of independence: Individuals with dementia often require significant care and support, losing their autonomy.
- Emotional toll on caregivers: Caring for someone with dementia can be physically and emotionally exhausting.
Fear of Heart Disease
Heart disease encompasses a range of conditions that affect the heart, including heart attacks and strokes. The fear associated with heart disease often centers on the potential for sudden death or disability. The often unpredictable nature of heart attacks and the potential for long-term complications contribute to the widespread anxiety. The fact that heart disease is often linked to lifestyle factors adds a layer of self-blame and guilt to the fear experienced by many.
- Sudden death risk: Heart attacks and strokes can cause sudden and unexpected death.
- Long-term disability: Heart disease can lead to significant long-term disabilities, impacting quality of life.
- Lifestyle factors: Many heart diseases are linked to lifestyle choices, causing some individuals to feel responsible for their condition.
Fear of Disability
The fear of acquiring a disability, whether physical or mental, is deeply rooted in anxieties about loss of independence, reduced quality of life, and societal stigma. The potential need for extensive care, financial strain, and social isolation associated with disability significantly contributes to widespread fear. The unpredictable nature of many disabling conditions, and the possibility of becoming a burden on family and friends, exacerbates this anxiety.
- Loss of independence: Disabilities can severely limit an individual's ability to perform daily tasks.
- Financial burden: The cost of medical care, assistive devices, and adaptive home modifications can be substantial.
- Social stigma: People with disabilities may face prejudice and discrimination.
Fear of Chronic Pain
Chronic pain, lasting for more than three months, is a debilitating condition that can severely impact quality of life. The persistent suffering and lack of effective treatment options for many types of chronic pain contribute to significant fear. The potential for long-term disability, the emotional toll, and the disruption of daily life make it a source of considerable anxiety for many individuals. The often subjective nature of pain makes it challenging to diagnose and treat effectively, further fueling this fear.
- Persistent suffering: Chronic pain is characterized by ongoing discomfort that can be debilitating.
- Treatment challenges: Finding effective pain management can be difficult and frustrating.
- Impact on daily life: Chronic pain can drastically disrupt daily activities, relationships, and overall well-being.
What chronic disease has no cure?
Many chronic diseases currently have no cure, meaning there is no treatment that will completely eliminate the disease and restore the body to a state of health before the onset of the disease. The progression of the disease may be managed, symptoms alleviated, and complications prevented or delayed, but the underlying condition persists. Examples include, but are not limited to, Alzheimer's disease, HIV/AIDS (though highly manageable with medication), multiple sclerosis, type 1 diabetes, and Huntington's disease. The specific disease considered to have "no cure" can depend on the specific definition of "cure" and ongoing research advancements.
What are some examples of incurable chronic diseases?
Several chronic diseases fall into the category of incurable. While treatments exist to improve quality of life and manage symptoms, these diseases are considered to be lifelong conditions. Effective management often involves a combination of therapies and lifestyle adjustments. Some notable examples include:
- Alzheimer's disease: A progressive neurodegenerative disorder characterized by memory loss, cognitive decline, and behavioral changes. Currently, there's no cure, but treatments aim to slow disease progression and manage symptoms.
- HIV/AIDS: While antiretroviral therapy (ART) can effectively suppress the virus and prevent disease progression, it doesn't eradicate the virus from the body. Therefore, it remains an incurable chronic disease.
- Multiple sclerosis (MS): An autoimmune disease affecting the central nervous system. There is no cure, but disease-modifying therapies can help manage symptoms and slow progression.
How are incurable chronic diseases managed?
Even without a cure, effective management of incurable chronic diseases is possible through various approaches. The primary goal is to improve the patient's quality of life, reduce symptoms, and prevent or delay complications. This often involves a multi-faceted approach:
- Medication: Drugs can target specific disease mechanisms or manage symptoms.
- Lifestyle modifications: Changes in diet, exercise, and stress management can significantly impact disease progression and symptom severity.
- Therapy: Physical, occupational, and speech therapy can aid in managing symptoms and improving functional abilities.
What is the difference between a chronic disease and an acute disease?
The key distinction lies in the duration and severity of the illness. Acute diseases have a relatively short duration and often resolve completely. Examples include the common cold or influenza. In contrast, chronic diseases are long-lasting, often persisting for years or even a lifetime, and usually have no cure. They may involve periods of remission and exacerbation (worsening of symptoms).
- Acute diseases typically have a clear onset and resolution.
- Chronic diseases gradually develop and have no known cure, though symptoms can be managed.
- Acute diseases usually respond well to treatment, leading to complete recovery; chronic diseases require ongoing management.
What is the impact of incurable chronic diseases on individuals and society?
Incurable chronic diseases profoundly impact individuals, their families, and society as a whole. The long-term nature of these conditions often leads to significant physical, emotional, and financial burdens.
- Individual impact: Reduced quality of life, limitations in daily activities, emotional distress, and increased healthcare costs.
- Family impact: Increased caregiving responsibilities, emotional strain, and financial burden.
- Societal impact: Reduced workforce productivity, increased healthcare expenditures, and strain on social support systems.
What is the role of research in addressing incurable chronic diseases?
Ongoing research plays a vital role in improving the management and understanding of incurable chronic diseases. While a cure may not always be possible, research efforts focus on several crucial areas:
- Identifying disease mechanisms: Understanding the underlying causes of the disease can lead to more effective treatment strategies.
- Developing new therapies: Research continually explores novel therapeutic approaches, including gene therapy and immunotherapy.
- Improving disease management: Research focuses on developing better ways to manage symptoms and improve patients' quality of life.
What is considered a fatal chronic condition?
A fatal chronic condition is a long-lasting health problem that ultimately leads to death. It's characterized by a slow progression of symptoms and a gradual decline in health over an extended period. Unlike acute conditions which have a rapid onset and relatively short duration, chronic conditions are persistent and often incurable, although their progression may be managed through treatment. The definition doesn't necessarily specify a specific timeframe for the condition's duration before it becomes fatal; the crucial element is the inevitable and terminal nature of the illness.
What are some examples of fatal chronic conditions?
Many conditions can be classified as fatal chronic conditions, depending on the individual's health and response to treatment. Some prominent examples include various forms of cancer, heart failure, chronic obstructive pulmonary disease (COPD), kidney failure, and advanced forms of Alzheimer's disease. The prognosis and timeline for these conditions vary significantly depending on factors such as the stage of the disease, the individual's overall health, and the effectiveness of available treatments.
- Cancer: Various types of cancer can be fatal if left untreated or if treatment is unsuccessful. The prognosis depends greatly on the type of cancer, its stage, and the individual's response to therapy.
- Heart Failure: This condition occurs when the heart cannot pump enough blood to meet the body's needs. It's often a progressive condition that can lead to death if not managed effectively.
- Chronic Obstructive Pulmonary Disease (COPD): COPD encompasses conditions like emphysema and chronic bronchitis, causing progressive airflow limitation and respiratory failure. It is a leading cause of death worldwide.
How are fatal chronic conditions diagnosed?
Diagnosis of fatal chronic conditions typically involves a combination of methods. This includes a thorough medical history review, physical examination, and various diagnostic tests. These tests might range from blood tests and imaging scans (like X-rays, CT scans, or MRIs) to specialized procedures like biopsies or endoscopies. Early diagnosis is crucial for maximizing the effectiveness of treatment and improving quality of life. Early detection and intervention are often key factors in determining the overall prognosis.
- Medical History: Detailed information about symptoms, family history, and lifestyle factors.
- Physical Examination: Assessment of vital signs, auscultation (listening to the lungs and heart), and palpation (feeling for abnormalities).
- Diagnostic Tests: Blood tests, imaging studies, and other specialized procedures to confirm the diagnosis and assess the severity of the condition.
What are the treatment options for fatal chronic conditions?
Treatment options for fatal chronic conditions depend entirely on the specific disease and its stage. They may include medications, surgery, radiation therapy, chemotherapy, palliative care, and lifestyle modifications. The goal of treatment is often to manage symptoms, slow disease progression, improve quality of life, and extend lifespan as much as possible. The emphasis often shifts towards palliative care in the later stages, focusing on comfort and pain management.
- Medication: To manage symptoms, slow disease progression, or target specific disease mechanisms.
- Surgery: In some cases, surgical intervention may be necessary to remove tumors, correct structural abnormalities, or improve organ function.
- Other Therapies: Radiation therapy, chemotherapy, and other advanced therapies may be used to treat certain conditions.
How can fatal chronic conditions impact quality of life?
Fatal chronic conditions significantly impact quality of life, both for the individual experiencing the condition and their families. The physical symptoms, limitations in daily activities, and emotional toll can be substantial. Financial burdens, social isolation, and emotional distress are common consequences. Access to appropriate medical care, support systems, and palliative care are vital in managing these impacts.
- Physical Limitations: Reduced mobility, pain, fatigue, and other physical symptoms.
- Emotional Distress: Anxiety, depression, and feelings of helplessness.
- Social and Economic Impacts: Loss of income, reduced social interaction, and increased reliance on caregivers.
What is the role of palliative care in managing fatal chronic conditions?
Palliative care plays a crucial role in managing fatal chronic conditions, especially in the later stages of the illness. It focuses on improving the quality of life for patients and their families by providing comfort and support. It addresses not only the physical symptoms but also the emotional, social, and spiritual needs of patients and their loved ones. Palliative care is not about hastening death, but about improving the patient's remaining time by managing pain, reducing other distressing symptoms, and ensuring a peaceful and dignified end-of-life experience.
- Pain and Symptom Management: Using medications and other therapies to control pain, nausea, shortness of breath, and other distressing symptoms.
- Emotional and Spiritual Support: Providing counseling, spiritual guidance, and emotional support to patients and their families.
- Practical Assistance: Helping with tasks such as coordinating care, managing medications, and providing resources for family caregivers.
What makes a chronic illness "hardest" to live with?
There's no single answer to what constitutes the "hardest" chronic illness. The experience is deeply personal and subjective, varying significantly based on individual factors. What one person finds overwhelmingly challenging, another might manage relatively well. The "hardest" illness isn't necessarily the one with the highest mortality rate or most visible symptoms. Instead, the severity depends on a complex interplay of factors. Pain levels are a significant contributor; chronic, unrelenting pain can profoundly impact quality of life, leading to depression, anxiety, and isolation. Cognitive impairment, common in conditions like multiple sclerosis or Alzheimer's disease, dramatically alters daily function and independence. The extent of functional limitations is another crucial aspect; illnesses that restrict mobility, dexterity, or basic bodily functions impose a heavy burden. Treatment burden also plays a significant role; some illnesses require intensive, complex, and time-consuming medical management, potentially interfering with work, relationships, and overall well-being. Finally, the psychological impact and the social stigma surrounding certain illnesses cannot be ignored. These factors can affect self-esteem, relationships, and access to support and resources. Ultimately, the "hardest" chronic illness is the one that most significantly impairs a person's ability to live a fulfilling and meaningful life, based on their unique circumstances and personal values.
Are there any chronic illnesses with consistently high levels of reported difficulty?
While individual experiences vary greatly, some chronic illnesses are frequently cited as particularly challenging to live with due to their wide-ranging and debilitating effects. Fibromyalgia, for instance, is characterized by widespread chronic pain, fatigue, and sleep disturbances, often leading to significant disability and impacting every aspect of life. The invisible nature of the illness can also lead to a lack of understanding and support from others. Chronic fatigue syndrome (ME/CFS) shares similar challenges, with debilitating fatigue and other symptoms that severely restrict physical and mental capabilities. The profound and often unpredictable nature of the fatigue makes planning daily activities extremely difficult. Multiple sclerosis (MS) is another condition often mentioned due to its unpredictable progression and the wide array of symptoms it can cause, from sensory disturbances and muscle weakness to cognitive impairment and emotional difficulties. Lupus presents another unique set of difficulties; its systemic nature can affect almost any organ system, resulting in a range of debilitating symptoms that are often difficult to diagnose and treat. The unpredictable nature of flares and remissions makes long-term planning and maintaining a sense of stability a constant struggle. It's important to remember that even within these conditions, individual experiences vary enormously. However, the combination of complex symptoms, unpredictable progression, and often limited effective treatment options frequently leads to significant hardship for those affected.
How does social support influence the experience of living with a chronic illness?
Social support plays a crucial, often underestimated, role in navigating the challenges of chronic illness. Strong social networks provide emotional, practical, and informational support that can significantly impact a person's ability to cope with their condition. Emotional support, from family, friends, and support groups, can help alleviate feelings of isolation, anxiety, and depression. Practical support, such as assistance with daily tasks or childcare, can free up time and energy for self-care and managing the illness. Informational support, including access to reliable information about the illness and available resources, can empower individuals to make informed decisions about their treatment and self-management. Conversely, a lack of social support can exacerbate the challenges of living with a chronic illness. Isolation and feelings of incomprehension can lead to increased stress, depression, and a decline in overall well-being. The stigma associated with certain illnesses can further isolate individuals, preventing them from seeking help or openly discussing their experiences. Therefore, fostering supportive relationships and creating inclusive communities is vital in improving the lives of those living with chronic illnesses. Accessing support groups, connecting with online communities, and engaging in activities that promote social interaction can significantly enhance coping mechanisms and improve quality of life.
What resources are available for people struggling with chronic illness?
A wide range of resources are available to help individuals cope with the challenges of chronic illness. Medical professionals, including doctors, specialists, and therapists, provide crucial medical care and treatment. Support groups, both online and in-person, offer peer support, shared experiences, and practical advice. Therapists and counselors can provide mental health support, helping individuals manage stress, anxiety, depression, and other emotional challenges. Many charities and non-profit organizations dedicate themselves to specific chronic illnesses, offering information, advocacy, and support services. These organizations often provide valuable resources on treatment options, financial assistance, and legal support. Government agencies also play a role in providing support, such as disability benefits and access to healthcare services. Online resources offer a wealth of information, including medical information, forums, and self-help guides. Finally, family and friends can be an invaluable source of support, offering emotional support, practical help, and companionship. It's crucial for individuals with chronic illnesses to actively seek out and utilize these resources, tailoring their approach to their specific needs and preferences. Finding the right combination of support systems and resources can significantly improve the quality of life and enable individuals to live fulfilling lives despite the challenges of their condition.
Deja una respuesta