What are usually the first signs of lupus

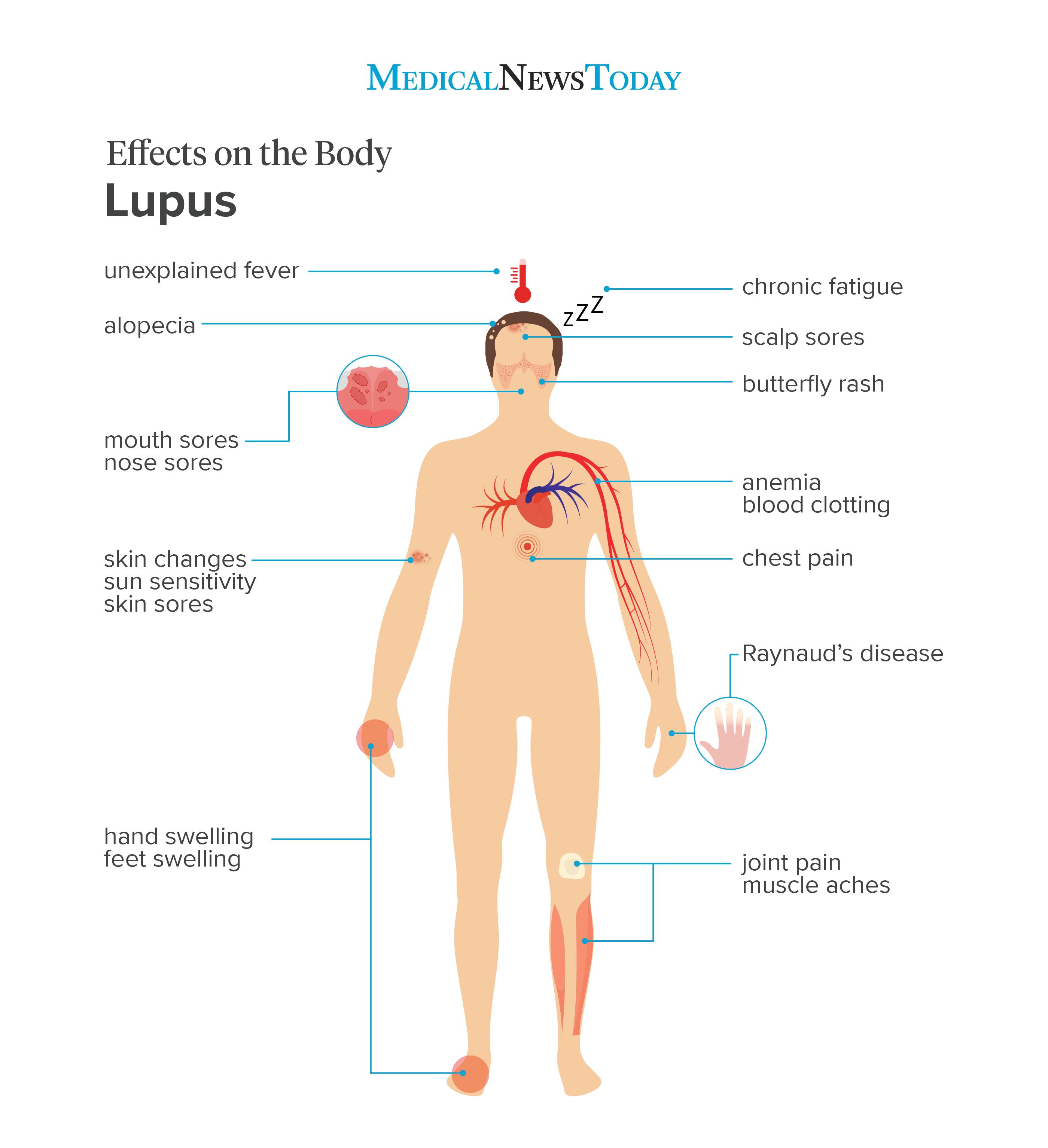
Lupus is an autoimmune disorder that can affect many different parts of the body. It can cause a wide range of symptoms, from mild to severe. The first signs of lupus can vary from person to person, but there are some common symptoms that are often seen early on.
What are the Initial Symptoms of Lupus?
Lupus is a complex autoimmune disease, meaning the body's immune system mistakenly attacks its own tissues and organs. Because of this complexity, the early signs of lupus can be incredibly varied and often mimic other illnesses, making diagnosis challenging. There's no single "first sign," and symptoms can appear gradually or suddenly. Many individuals experience a range of symptoms before a diagnosis, often leading to delays in receiving proper care. It's crucial to note that experiencing some of these symptoms doesn't automatically mean you have lupus; a proper diagnosis requires medical evaluation.
Fatigue and Malaise
Fatigue is arguably one of the most common initial symptoms. It's not just tiredness; it's an overwhelming exhaustion that persists despite rest. This debilitating fatigue can significantly impact daily activities and quality of life. Associated with this is a general feeling of malaise – a vague feeling of discomfort, illness, or unease that's difficult to pinpoint.
Joint Pain and Swelling (Arthralgia)
Many people with lupus experience joint pain (arthralgia) and swelling, often affecting multiple joints simultaneously. This pain can range from mild discomfort to severe, debilitating inflammation. The joints most commonly affected are those in the hands, wrists, and knees. The symptoms often improve with rest, but activity can exacerbate them. Important to distinguish from arthritis, Lupus-related joint pain generally doesn't cause permanent joint damage, although long-term inflammation can.
Skin Rashes (Malar Rash or Butterfly Rash)
A characteristic sign, though not always present, is a malar rash, often called a "butterfly rash" because of its shape across the cheeks and bridge of the nose. This rash is typically red, flat, and may be slightly raised. However, lupus rashes can manifest in various ways, including discoid lupus (raised, scaly patches), photosensitivity (skin sensitivity to sunlight), and other types of rashes that appear elsewhere on the body.
Fever
Low-grade fever is another common early sign. This fever is often unexplained, meaning there's no apparent infection or other cause. It can come and go, making it difficult to diagnose if other symptoms aren't present. The fever itself is typically not high, but it can be persistent and contribute to the overall feeling of malaise and fatigue.
Swollen Lymph Nodes and Headaches
Swollen lymph nodes, often found in the neck or armpits, can occur. These swellings are a result of the immune system's overactivity. Frequent or severe headaches are also reported by many individuals with early-stage lupus. These headaches can be persistent, and their intensity may vary.
| Symptom | Description | Significance |
|---|---|---|
| Fatigue | Overwhelming exhaustion despite rest | One of the most common initial symptoms |
| Joint pain (arthralgia) and swelling | Pain and swelling in multiple joints | Often affects hands, wrists, and knees |
| Malar rash ("butterfly rash") | Red, flat rash across cheeks and nose | Characteristic, but not always present |
| Low-grade fever | Unexplained, persistent low fever | Can be intermittent and difficult to diagnose |
| Swollen lymph nodes and headaches | Swollen lymph nodes and frequent headaches | Result of immune system overactivity |
https://youtube.com/watch?v=10-early-signs
What are the Initial Symptoms of Lupus?
Lupus is a complex autoimmune disease, meaning the body's immune system mistakenly attacks its own tissues and organs. Because of this complexity, the early signs of lupus can be incredibly varied and often mimic other illnesses, making diagnosis challenging. There's no single "first sign," and symptoms can appear gradually or suddenly. Many individuals experience a range of symptoms before a diagnosis, often leading to delays in receiving proper care. It's crucial to note that experiencing some of these symptoms doesn't automatically mean you have lupus; a proper diagnosis requires medical evaluation.
Fatigue and Malaise
Fatigue is arguably one of the most common initial symptoms. It's not just tiredness; it's an overwhelming exhaustion that persists despite rest. This debilitating fatigue can significantly impact daily activities and quality of life. Associated with this is a general feeling of malaise – a vague feeling of discomfort, illness, or unease that's difficult to pinpoint.
Joint Pain and Swelling (Arthralgia)
Many people with lupus experience joint pain (arthralgia) and swelling, often affecting multiple joints simultaneously. This pain can range from mild discomfort to severe, debilitating inflammation. The joints most commonly affected are those in the hands, wrists, and knees. The symptoms often improve with rest, but activity can exacerbate them. Important to distinguish from arthritis, Lupus-related joint pain generally doesn't cause permanent joint damage, although long-term inflammation can.
Skin Rashes (Malar Rash or Butterfly Rash)
A characteristic sign, though not always present, is a malar rash, often called a "butterfly rash" because of its shape across the cheeks and bridge of the nose. This rash is typically red, flat, and may be slightly raised. However, lupus rashes can manifest in various ways, including discoid lupus (raised, scaly patches), photosensitivity (skin sensitivity to sunlight), and other types of rashes that appear elsewhere on the body.
Fever
Low-grade fever is another common early sign. This fever is often unexplained, meaning there's no apparent infection or other cause. It can come and go, making it difficult to diagnose if other symptoms aren't present. The fever itself is typically not high, but it can be persistent and contribute to the overall feeling of malaise and fatigue.
Swollen Lymph Nodes and Headaches
Swollen lymph nodes, often found in the neck or armpits, can occur. These swellings are a result of the immune system's overactivity. Frequent or severe headaches are also reported by many individuals with early-stage lupus. These headaches can be persistent, and their intensity may vary.
| Symptom | Description | Significance |
|---|---|---|
| Fatigue | Overwhelming exhaustion despite rest | One of the most common initial symptoms |
| Joint pain (arthralgia) and swelling | Pain and swelling in multiple joints | Often affects hands, wrists, and knees |
| Malar rash ("butterfly rash") | Red, flat rash across cheeks and nose | Characteristic, but not always present |
| Low-grade fever | Unexplained, persistent low fever | Can be intermittent and difficult to diagnose |
| Swollen lymph nodes and headaches | Swollen lymph nodes and frequent headaches | Result of immune system overactivity |
What are the warning signs of lupus?
Lupus is a chronic autoimmune disease where the body's immune system attacks its own tissues and organs. Because it can affect many different parts of the body, lupus symptoms vary widely from person to person and can come and go. There's no single test to diagnose lupus; diagnosis often involves a combination of physical examination, medical history, blood tests, and sometimes biopsies. Early recognition of warning signs is crucial for timely diagnosis and management of the disease to prevent long-term complications.
Skin Manifestations of Lupus
Skin problems are common in lupus. The characteristic rash, often described as a butterfly-shaped rash across the cheeks and bridge of the nose, is a hallmark sign, but not all lupus patients develop this. Other skin manifestations can include:
- Discoid lupus: Thick, scaly, red patches that can scar.
- Photosensitivity: Extreme sensitivity to sunlight, resulting in skin rashes or worsening of existing rashes.
- Other rashes: Various rashes may appear on other parts of the body, often triggered by sun exposure or infection.
Joint Pain and Inflammation
Musculoskeletal problems are prevalent in lupus. Many patients experience persistent pain, stiffness, and swelling in their joints, especially in the hands, wrists, and knees. This is often referred to as lupus arthritis. The symptoms can be quite debilitating:
- Arthritis: Joint pain, swelling, and inflammation.
- Fatigue: Severe tiredness that doesn't improve with rest.
- Myalgia: Muscle pain and aches.
Fatigue and Fever
Feeling constantly tired, even after a full night's sleep, is a very common symptom of lupus. This fatigue can be profound and significantly impact daily activities. Low-grade fevers can also occur frequently, sometimes without any other apparent cause:
- Unexplained fatigue: Persistent tiredness that is not relieved by rest.
- Low-grade fever: A temperature slightly above normal, often intermittent.
- Malaise: A general feeling of discomfort, illness, or unease.
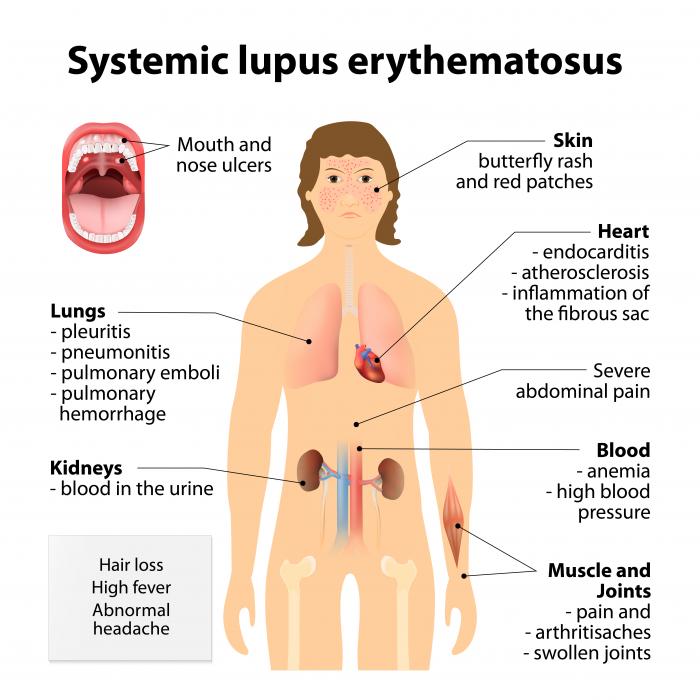
Kidney Problems (Lupus Nephritis)
Lupus can affect the kidneys, leading to lupus nephritis, a serious complication. This condition can cause inflammation and damage to the kidneys, potentially leading to kidney failure if left untreated. Early detection is crucial:
- Protein in the urine (proteinuria): Detected through urine tests.
- High blood pressure (hypertension): A common consequence of kidney damage.
- Swelling in the legs, feet, or ankles (edema): Due to fluid retention.
Other Systemic Symptoms
Lupus can impact various organ systems, leading to a wide range of symptoms. These symptoms often overlap with other illnesses, making diagnosis more challenging. It's crucial to consult a doctor if you experience persistent or unusual symptoms:
- Chest pain (pleuritis or pericarditis): Inflammation of the lining of the lungs or heart.
- Neurological symptoms: Headaches, seizures, cognitive difficulties.
- Anemia: Low red blood cell count.
What does undiagnosed lupus look like?
Undiagnosed lupus presents a significant challenge because its symptoms are incredibly varied and often mimic other illnesses. There isn't a single, definitive presentation. Instead, individuals experience a constellation of symptoms that can change in intensity and type over time. This makes diagnosis difficult and often leads to significant delays. The symptoms can range from mild to severe, and the pattern of symptoms varies greatly from person to person. The lack of a specific, consistent presentation is a hallmark of undiagnosed lupus. Many patients experience a gradual onset of symptoms, making it difficult to pinpoint a specific starting point. This often leads to frustration for both the patient and their healthcare provider as they attempt to find an explanation for their deteriorating health.
Symptoms Mimicking Other Illnesses
One of the most frustrating aspects of undiagnosed lupus is its ability to mimic other conditions. Many patients initially seek treatment for what seems like a common ailment, only to find that the symptoms persist and worsen. This often leads to a long and arduous diagnostic journey involving multiple specialists and numerous tests. The chameleon-like nature of lupus symptoms can significantly delay diagnosis.
- Fatigue: This is a pervasive symptom, often dismissed as stress or lifestyle factors.
- Joint pain (arthralgia) and swelling (arthritis): Frequently mistaken for rheumatoid arthritis or other musculoskeletal conditions.
- Skin rashes (malar rash, discoid rash): These can be mistaken for other skin conditions, making identification challenging.
Fluctuating Symptoms and Relapses
Another characteristic of undiagnosed lupus is the fluctuating nature of its symptoms. Patients may experience periods of remission where symptoms improve or even disappear, followed by periods of relapse where symptoms return with increased severity. This unpredictable pattern of symptom flare-ups and remissions makes it difficult to establish a clear diagnosis. This waxing and waning of symptoms can lead to misdiagnosis or dismissal of the condition altogether.
- Periods of intense symptom activity followed by periods of relative well-being.
- Symptoms that can vary in location and severity from one day to the next.
- Difficulty in predicting when a flare-up might occur.
Impact on Organ Systems
Lupus is a systemic autoimmune disease, meaning it can affect multiple organ systems in the body. Undiagnosed lupus can lead to significant damage to vital organs if left untreated. Early detection and management are crucial to preventing organ damage. This highlights the importance of seeking medical attention when experiencing persistent and unexplained symptoms.
- Kidney involvement (lupus nephritis): Can lead to kidney failure if untreated.
- Lung problems (pleuritis, pneumonitis): May cause shortness of breath and chest pain.
- Heart problems (pericarditis, myocarditis): Can lead to heart inflammation and irregular heartbeat.
Neurological Manifestations
Many individuals with lupus experience neurological symptoms that can range from mild to severe. These symptoms can be quite debilitating and significantly impact daily life. The neurological manifestations of lupus can be easily overlooked or attributed to other causes, further delaying diagnosis. Prompt and comprehensive evaluation is crucial to differentiate these symptoms from other neurological disorders.
- Headaches, often severe and persistent.
- Cognitive dysfunction ("brain fog"), affecting memory, concentration, and processing speed.
- Seizures or stroke in severe cases.
Diagnostic Delays and Frustration
The multifaceted nature of lupus symptoms often leads to significant delays in diagnosis. Patients may visit multiple healthcare professionals, undergo numerous tests, and still remain undiagnosed for years. This prolonged period of uncertainty can be extremely frustrating and emotionally taxing for patients. The lack of a definitive diagnostic test adds to the challenge, necessitating a thorough evaluation and consideration of various symptoms and risk factors.
- Multiple consultations with different specialists.
- Extensive testing, including blood tests, imaging studies, and biopsies.
- Significant emotional distress from the uncertainty and prolonged search for answers.
How long can you have lupus without knowing?
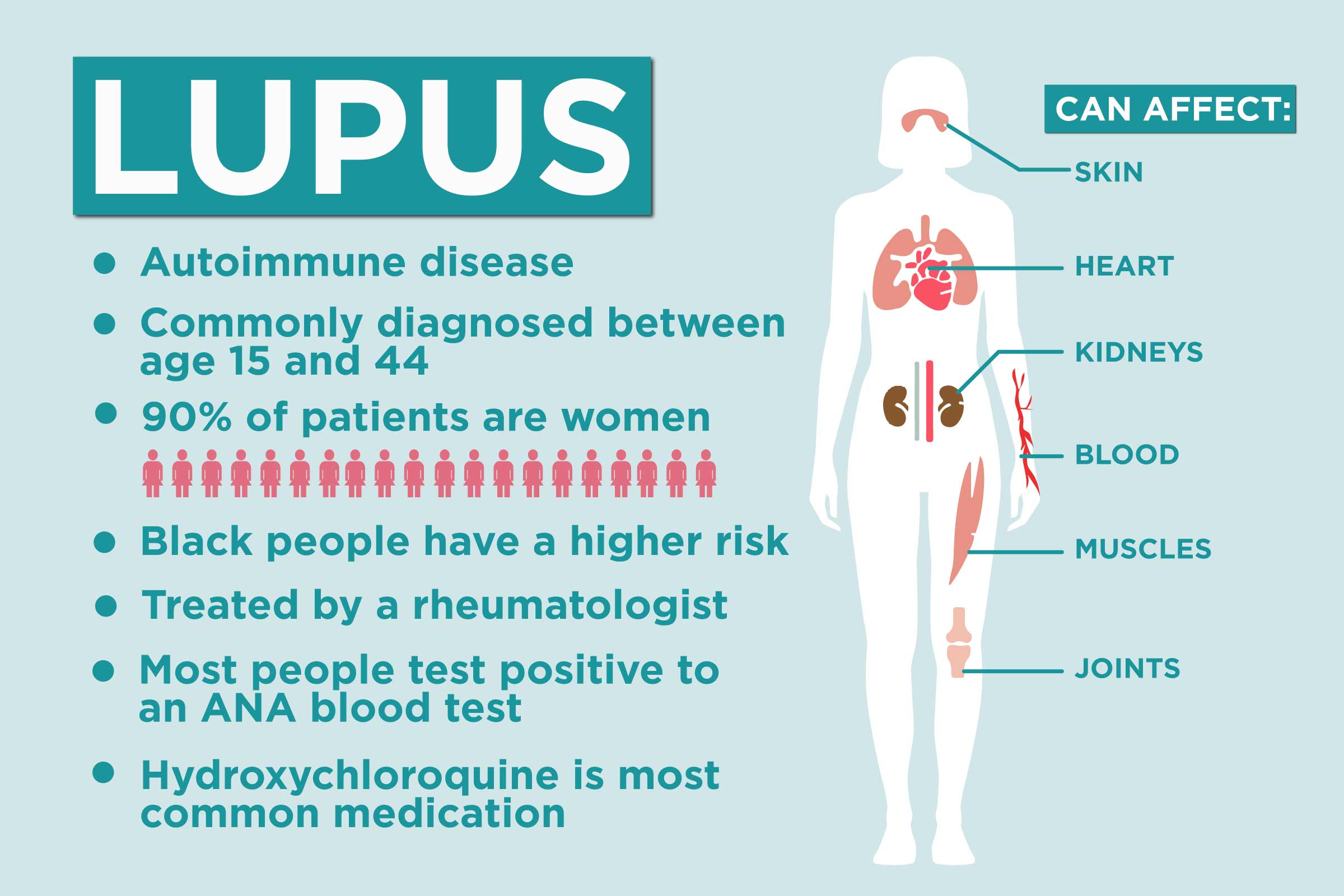
The length of time someone can have lupus without knowing varies greatly. It depends on several factors including the severity of the disease, the specific symptoms experienced, and the individual's access to healthcare. Some individuals may experience mild, intermittent symptoms that are easily dismissed or attributed to other conditions. Others may experience a more aggressive form of the disease with more noticeable and debilitating symptoms. There is no set timeframe. Some people may live with undiagnosed lupus for months, while others may go years, even decades, before receiving a diagnosis. The key is that lupus is a highly variable disease, and its presentation can be very different from person to person.
Symptoms Mimicking Other Illnesses
Many lupus symptoms are non-specific, meaning they can be associated with a wide range of other illnesses. This makes it challenging to identify lupus early on. For instance, fatigue, joint pain, and rashes can be symptoms of numerous common conditions. The overlapping symptoms with other conditions often lead to delayed diagnosis. The delay is further complicated by the fact that lupus symptoms often come and go, making it difficult to establish a consistent pattern.
- Fatigue: Can be mistaken for stress, lack of sleep, or anemia.
- Joint pain: Often confused with arthritis or other musculoskeletal disorders.
- Rashes: May be misdiagnosed as allergic reactions or other skin conditions.
The Role of Systemic Symptoms
The presence or absence of systemic symptoms—those affecting multiple organs—greatly influences the time to diagnosis. Individuals with mild or localized lupus may have only skin or joint problems, delaying diagnosis. Conversely, those with more significant systemic involvement, such as kidney or lung problems, are more likely to seek medical attention sooner and receive a faster diagnosis. Systemic lupus erythematosus (SLE), the most common type, involves multiple organ systems and can progress quickly if untreated, underscoring the importance of prompt medical evaluation when experiencing widespread symptoms.
- Kidney involvement (Lupus nephritis): Can cause significant health issues if undetected and untreated.
- Lung involvement (Lupus pneumonitis): Causes shortness of breath and can be life-threatening.
- Neurological involvement: Can lead to headaches, seizures, or cognitive impairment.
Impact of Healthcare Access
Access to quality healthcare plays a crucial role in the time it takes to diagnose lupus. Individuals with limited access to healthcare providers, particularly specialists like rheumatologists, may experience longer delays in diagnosis. Early and accurate diagnosis is paramount for effective management and to prevent the development of serious complications. Furthermore, socioeconomic factors and healthcare disparities can impact both access to care and the quality of care received.
- Delayed specialist referrals: Can significantly prolong the diagnostic process.
- Lack of awareness among primary care physicians: Can lead to missed diagnoses.
- Financial barriers to accessing healthcare: Prevent timely testing and specialist visits.
Variability of Lupus Presentation
Lupus is a highly heterogeneous disease, meaning it can manifest differently in each individual. This variability makes diagnosis challenging, as symptoms can vary widely in type, severity, and frequency. One person might experience predominantly skin rashes, while another might have severe kidney disease. This unpredictable nature makes it difficult to establish a universal timeframe for diagnosis. The diverse range of symptoms necessitates a thorough medical evaluation to correctly identify the condition.
- Mild lupus: May cause only mild fatigue and joint pain.
- Severe lupus: Can lead to life-threatening organ damage.
- Drug-induced lupus: Caused by certain medications, presenting unique challenges.
How does lupus start off?

Lupus is a complex autoimmune disease with a variable presentation, meaning there's no single way it "starts off." The onset can be gradual and subtle, with symptoms developing slowly over time, or it can be sudden and dramatic with a clear trigger event. Often, the initial symptoms are nonspecific and mimic those of other illnesses, making diagnosis challenging. These early symptoms can range from mild fatigue and joint pain to more severe manifestations like rashes and organ involvement. The body's immune system mistakenly attacks its own tissues and organs, causing inflammation and damage. The initial symptoms frequently vary greatly depending on the individual and the specific type of lupus. There is no single definitive test to diagnose lupus, rather a combination of blood tests, physical exams, and possibly imaging studies are needed.
Initial Symptoms: A Kaleidoscope of Possibilities
Early symptoms of lupus are notoriously vague and often overlap with other conditions. This makes early diagnosis difficult. Many individuals initially attribute their symptoms to other, more common ailments, delaying proper medical attention. The symptoms can wax and wane, appearing and disappearing over time, further complicating the picture. This unpredictable nature makes tracking the onset of lupus even more challenging.
- Fatigue: Persistent tiredness that doesn't improve with rest.
- Joint pain (arthralgia): Pain and stiffness in multiple joints, often without significant swelling.
- Skin rashes: The characteristic "butterfly rash" across the face is a common, but not universal, early sign. Other rashes can also occur.
The Role of Genetics and Environment
While the exact cause of lupus remains unknown, it's believed to be a complex interplay of genetic predisposition and environmental triggers. Individuals with a family history of lupus have a higher risk of developing the disease themselves. Environmental factors, such as exposure to sunlight, infections, certain medications, and even stress, can potentially trigger or exacerbate lupus symptoms in genetically susceptible individuals.
- Genetic factors increase susceptibility but don't guarantee disease development.
- Environmental triggers can activate the autoimmune response in those genetically predisposed.
- The interaction between genes and environment is crucial in understanding lupus onset.
Autoimmune Response: The Body Attacking Itself
At the heart of lupus lies a malfunctioning immune system. Instead of targeting foreign invaders like bacteria and viruses, the immune system in lupus mistakenly identifies the body's own tissues as threats. This autoimmune response leads to the production of autoantibodies, which attack various parts of the body, causing inflammation and tissue damage. The severity and location of this damage dictate the specific symptoms experienced by each individual.
- Autoantibodies attack healthy cells and tissues.
- Inflammation is a key consequence of the autoimmune attack.
- The type and location of tissue damage determine symptom presentation.
Diagnostic Challenges: Mimicking Other Illnesses
The nonspecific nature of early lupus symptoms poses a significant challenge to diagnosis. Many of the initial symptoms, such as fatigue, joint pain, and rashes, are common to various other conditions. This can lead to delays in diagnosis, potentially allowing the disease to progress before appropriate treatment is initiated. Accurate diagnosis often requires a comprehensive evaluation involving blood tests, physical examination, and sometimes imaging studies.
- Early symptoms often mimic those of other, more common illnesses.
- Diagnosis can be delayed due to the nonspecific nature of early symptoms.
- A multi-faceted approach is needed to reach an accurate diagnosis.
Subclinical Lupus: The Silent Onset
In some cases, individuals may have subclinical lupus, meaning they have the autoantibodies characteristic of lupus but don't yet experience overt symptoms. This asymptomatic phase may precede the development of noticeable symptoms by months or even years. Identifying subclinical lupus can be challenging, often requiring serological testing for autoantibodies. The transition from subclinical to symptomatic lupus is unpredictable and varies greatly between individuals.
- Autoantibodies are present but clinical symptoms are absent.
- The transition to symptomatic disease can be gradual and unpredictable.
- Identifying subclinical lupus helps in early intervention and management.
What are the most common early symptoms of lupus?
Lupus is notoriously tricky to diagnose because its symptoms are incredibly varied and often mimic other conditions. There isn't one single "first sign," but some of the most frequently reported early symptoms include unexplained fatigue. This fatigue is often profound and debilitating, far exceeding what one would expect from normal tiredness. It's crucial to note that fatigue alone isn't diagnostic of lupus, but it's a very common presenting symptom. Another prevalent early sign is a rash, often described as a butterfly-shaped rash across the face, but it can manifest in other areas of the body as well. This rash can be sensitive to sunlight, a key characteristic. Joint pain and swelling (arthritis) are also common early symptoms, often affecting multiple joints symmetrically. This pain can range from mild discomfort to severe, debilitating inflammation. Many individuals also experience fever, sometimes with no apparent cause, along with swollen lymph nodes. It's important to remember that these symptoms can appear and disappear, making it even more challenging for diagnosis. The insidious onset of symptoms is a hallmark of lupus, often making it difficult to pinpoint a specific starting point. Raynaud's phenomenon, characterized by changes in finger and toe color in response to cold temperatures or stress, is another frequently reported early symptom. Finally, unexplained hair loss can also occur early in the course of the disease. The presence of one or several of these symptoms warrants a visit to a doctor for proper evaluation and testing.
Can lupus symptoms vary significantly from person to person?
Absolutely. One of the most frustrating aspects of lupus is its extreme variability. While the symptoms mentioned above are common, the severity and combination of symptoms can differ dramatically between individuals. Some people experience mild, manageable symptoms, while others face severe and life-threatening complications. This variability is due to several factors, including genetic predisposition, environmental triggers, and the specific autoantibodies present in the body. For example, one person might primarily experience joint pain, while another might predominantly suffer from skin rashes, and yet another might have significant kidney involvement. This heterogeneity makes diagnosis challenging and necessitates a comprehensive evaluation, including blood tests, imaging studies, and a thorough medical history. Moreover, the symptoms can fluctuate over time; periods of remission (where symptoms are minimal or absent) can alternate with flare-ups (periods of increased disease activity). This unpredictable nature underscores the importance of ongoing monitoring and management by a healthcare professional specializing in lupus.
How do I know if my symptoms are lupus-related or something else?
This is a critical question, and only a qualified healthcare professional can provide an accurate diagnosis. Many of the symptoms of lupus overlap with those of other conditions, making self-diagnosis unreliable and potentially dangerous. For example, fatigue can be caused by numerous factors, as can joint pain, rashes, and fevers. Therefore, it's essential to seek medical attention if you're experiencing a combination of unexplained symptoms, especially if they are persistent or worsening. Your doctor will likely conduct a thorough physical examination, review your medical history, and order blood tests to check for specific autoantibodies associated with lupus. Other tests, such as urinalysis (to assess kidney function), imaging studies (like ultrasound or MRI), and biopsy (a small tissue sample) might be necessary depending on your symptoms and the doctor’s assessment. It's crucial to be open and honest with your doctor about all your symptoms, even those that seem unrelated, as this information helps them form a complete picture. Remember, early diagnosis and management are crucial for improving the long-term prognosis for lupus.
Should I be concerned if I experience only one or two of these symptoms?
While experiencing one or two symptoms mentioned doesn't automatically mean you have lupus, it's still important to seek medical advice. These symptoms, particularly when combined or persistent, can indicate a variety of health problems. The presence of even a single unusual symptom warrants a consultation with your doctor to rule out more serious conditions, including lupus. However, don't panic. Many illnesses present with overlapping symptoms, and a thorough medical evaluation is the best way to determine the underlying cause. The goal is to receive a proper diagnosis and develop a treatment plan that addresses your specific health concerns. It’s better to be proactive and address any concerns with a medical professional than to delay seeking help. Your doctor will be able to assess your individual circumstances, considering the duration and intensity of your symptoms, along with your medical history and family history, to determine the next steps. Remember, early detection is key to effective management of many health conditions.
Deja una respuesta