What deficiency causes mouth sores

Experiencing mouth sores can be an uncomfortable and painful inconvenience. Understanding the underlying cause of these lesions is crucial for effective treatment and prevention. One potential factor that may contribute to mouth sores is a deficiency in certain vitamins and minerals. This article aims to explore the connection between nutritional deficiencies and mouth sores, identifying the specific nutrients that may be lacking and discussing the implications for individuals seeking relief from this common ailment.
What Nutritional Deficiencies Can Cause Mouth Sores?
Mouth sores, also known as aphthous ulcers or canker sores, can be a pesky and painful problem. While many factors can contribute to their development, certain nutritional deficiencies are often implicated. Let's explore some of the key deficiencies linked to mouth sores.
Vitamin B12 Deficiency
Vitamin B12 plays a crucial role in cell growth and development, including the maintenance of healthy mucous membranes in the mouth. A deficiency can lead to various symptoms, including mouth sores. The body needs B12 to produce red blood cells, and a shortage can result in anemia and potentially lesions in the mouth. This deficiency is more common in vegetarians, vegans, and older adults who may have difficulty absorbing B12 from food. Symptoms can be subtle initially, often manifesting as fatigue and weakness before progressing to more noticeable signs like mouth sores.
Iron Deficiency
Iron is essential for red blood cell production. An iron deficiency, leading to anemia, can manifest as mouth sores alongside fatigue, weakness, and pale skin. The connection between iron and mouth sores is thought to be related to the impact iron has on the immune system and the body's ability to repair damaged tissues. Iron deficiency is common, particularly among women of childbearing age and individuals with poor diets. It is important to note that not all mouth sores are caused by iron deficiency. Other factors, including stress and trauma, can also play a role.
Folic Acid Deficiency
Folic acid, a B vitamin, is vital for cell growth and development. Similar to B12 and iron deficiencies, a folic acid deficiency can lead to mouth sores as a consequence of impaired cell renewal in the oral mucosa. This deficiency can cause anemia, and may also contribute to other symptoms like fatigue and neurological problems. Pregnant women are often advised to ensure adequate folic acid intake to prevent neural tube defects in the developing fetus, and an adequate intake is also beneficial for preventing oral issues.
Zinc Deficiency
Zinc plays a significant role in immune function and wound healing. A zinc deficiency can impair the body's ability to fight off infections and repair damaged tissues, leading to the development of mouth sores. Zinc is crucial for maintaining the integrity of the skin and mucous membranes, and its lack can increase vulnerability to infections and slow down the healing process. This deficiency can manifest in various ways, and mouth sores are just one potential symptom.
Vitamin C Deficiency
While less directly linked than other deficiencies, vitamin C, a powerful antioxidant, plays a role in collagen production. Vitamin C deficiency, or scurvy, can result in weakened blood vessels and impaired wound healing, potentially contributing to mouth sores and other symptoms like bleeding gums and skin bruising. While less common in developed countries due to widespread access to fruits and vegetables, severe vitamin C deficiency can have substantial health consequences, affecting the entire body’s ability to repair itself.
| Deficiency | Symptoms | Other potential symptoms |
|---|---|---|
| Vitamin B12 | Mouth sores, fatigue | Anemia, neurological problems |
| Iron | Mouth sores, fatigue, weakness | Anemia, pale skin |
| Folic Acid | Mouth sores, fatigue | Anemia, neurological problems |
| Zinc | Mouth sores, impaired wound healing | Weakened immune system |
| Vitamin C | Potentially contributes to mouth sores | Bleeding gums, skin bruising (scurvy) |
What Nutritional Deficiencies Can Cause Mouth Sores?
Mouth sores, also known as aphthous ulcers or canker sores, can be a pesky and painful problem. While many factors can contribute to their development, certain nutritional deficiencies are often implicated. Let's explore some of the key deficiencies linked to mouth sores.
Vitamin B12 Deficiency
Vitamin B12 plays a crucial role in cell growth and development, including the maintenance of healthy mucous membranes in the mouth. A deficiency can lead to various symptoms, including mouth sores. The body needs B12 to produce red blood cells, and a shortage can result in anemia and potentially lesions in the mouth. This deficiency is more common in vegetarians, vegans, and older adults who may have difficulty absorbing B12 from food. Symptoms can be subtle initially, often manifesting as fatigue and weakness before progressing to more noticeable signs like mouth sores.
Iron Deficiency
Iron is essential for red blood cell production. An iron deficiency, leading to anemia, can manifest as mouth sores alongside fatigue, weakness, and pale skin. The connection between iron and mouth sores is thought to be related to the impact iron has on the immune system and the body's ability to repair damaged tissues. Iron deficiency is common, particularly among women of childbearing age and individuals with poor diets. It is important to note that not all mouth sores are caused by iron deficiency. Other factors, including stress and trauma, can also play a role.
Folic Acid Deficiency
Folic acid, a B vitamin, is vital for cell growth and development. Similar to B12 and iron deficiencies, a folic acid deficiency can lead to mouth sores as a consequence of impaired cell renewal in the oral mucosa. This deficiency can cause anemia, and may also contribute to other symptoms like fatigue and neurological problems. Pregnant women are often advised to ensure adequate folic acid intake to prevent neural tube defects in the developing fetus, and an adequate intake is also beneficial for preventing oral issues.
Zinc Deficiency
Zinc plays a significant role in immune function and wound healing. A zinc deficiency can impair the body's ability to fight off infections and repair damaged tissues, leading to the development of mouth sores. Zinc is crucial for maintaining the integrity of the skin and mucous membranes, and its lack can increase vulnerability to infections and slow down the healing process. This deficiency can manifest in various ways, and mouth sores are just one potential symptom.
Vitamin C Deficiency
While less directly linked than other deficiencies, vitamin C, a powerful antioxidant, plays a role in collagen production. Vitamin C deficiency, or scurvy, can result in weakened blood vessels and impaired wound healing, potentially contributing to mouth sores and other symptoms like bleeding gums and skin bruising. While less common in developed countries due to widespread access to fruits and vegetables, severe vitamin C deficiency can have substantial health consequences, affecting the entire body’s ability to repair itself.
| Deficiency | Symptoms | Other potential symptoms |
|---|---|---|
| Vitamin B12 | Mouth sores, fatigue | Anemia, neurological problems |
| Iron | Mouth sores, fatigue, weakness | Anemia, pale skin |
| Folic Acid | Mouth sores, fatigue | Anemia, neurological problems |
| Zinc | Mouth sores, impaired wound healing | Weakened immune system |
| Vitamin C | Potentially contributes to mouth sores | Bleeding gums, skin bruising (scurvy) |
What vitamins are you lacking if you have mouth sores?

Mouth sores, also known as aphthous ulcers or canker sores, can be a sign of several nutritional deficiencies. While many factors contribute to their development, deficiencies in certain vitamins and minerals are frequently implicated. The most commonly associated vitamins are B vitamins, particularly B12, B6, and B9 (folate), and iron. A deficiency in zinc can also play a role. It's important to note that mouth sores can have many causes, and a deficiency isn't always the culprit. Other factors include stress, injury, certain medications, and underlying medical conditions. If you experience recurring or severe mouth sores, consulting a doctor or registered dietitian is crucial for proper diagnosis and treatment.
Vitamin B12 Deficiency and Mouth Sores
Vitamin B12 is crucial for DNA synthesis, red blood cell formation, and neurological function. A deficiency can manifest in various ways, including mouth sores. A lack of B12 interferes with cell growth and repair, leading to the formation of painful ulcers in the mouth. Other symptoms of B12 deficiency can include fatigue, weakness, and neurological problems. It's often found in animal products and supplementation might be needed for vegans or vegetarians.
- Symptoms: Mouth sores, fatigue, weakness, numbness in extremities, anemia.
- Sources: Meat, poultry, fish, eggs, dairy products, fortified cereals.
- Treatment: B12 supplements, dietary changes.
Folate (Vitamin B9) Deficiency and Mouth Sores
Folate is essential for cell growth and development. Deficiency in folate can significantly impact the health of the oral mucosa, increasing the susceptibility to mouth sores. This vitamin plays a key role in cell regeneration and repair. A lack of folate can also lead to anemia and other health problems.
- Symptoms: Mouth sores, fatigue, anemia, pale skin.
- Sources: Leafy green vegetables, legumes, citrus fruits, fortified grains.
- Treatment: Folate supplements, dietary changes.
Vitamin B6 Deficiency and Mouth Sores
Vitamin B6 is involved in numerous metabolic processes, including the formation of red blood cells. While less directly linked to mouth sores than B12 and folate, a significant deficiency in B6 can contribute to oral health problems. It supports immune function which may indirectly affect the healing process of mouth sores.
- Symptoms: Mouth sores (less common than with B12 or folate deficiency), fatigue, weakness, depression, skin rashes.
- Sources: Chicken, fish, bananas, potatoes, chickpeas.
- Treatment: B6 supplements, dietary changes.
Iron Deficiency and Mouth Sores
Iron is vital for carrying oxygen throughout the body. Iron deficiency anemia can lead to various oral manifestations, including mouth sores. The lack of sufficient oxygen supply to the tissues impairs healing and can make the mouth more prone to ulceration.
- Symptoms: Mouth sores, fatigue, weakness, pale skin, shortness of breath.
- Sources: Red meat, spinach, beans, lentils, fortified cereals.
- Treatment: Iron supplements, dietary changes.
Zinc Deficiency and Mouth Sores
Zinc is a mineral essential for wound healing and immune function. A zinc deficiency can impair the body's ability to repair damaged tissues, potentially leading to prolonged or recurring mouth sores. Zinc plays a crucial role in cell growth and immune responses that help combat infections that could worsen mouth sores.
- Symptoms: Mouth sores, impaired wound healing, weakened immune system, hair loss.
- Sources: Oysters, red meat, beans, nuts, seeds.
- Treatment: Zinc supplements, dietary changes.
Why am I suddenly getting mouth sores?

Why Am I Suddenly Getting Mouth Sores?
The sudden appearance of mouth sores, medically known as aphthous ulcers or canker sores, can be frustrating and painful. There isn't one single cause, and often it's a combination of factors that trigger their development. Possible culprits range from minor irritations to underlying medical conditions. Determining the exact reason requires consideration of your individual circumstances and medical history. A visit to a dentist or doctor is advisable if the sores are severe, persistent, or accompanied by other symptoms.
Stress and Anxiety
Stress and anxiety are frequently cited triggers for mouth sores. When you're stressed, your immune system can be weakened, making you more susceptible to infections and inflammation, including the development of canker sores. Managing stress through techniques like exercise, meditation, or yoga can potentially reduce their occurrence.
- Stress hormones: Elevated cortisol levels can directly impact the mouth's mucosal lining.
- Weakened immunity: Chronic stress compromises the immune system's ability to fight off minor infections.
- Increased inflammation: Stress can promote systemic inflammation, contributing to sore development.
Nutritional Deficiencies
Dietary deficiencies, particularly in certain vitamins and minerals, can play a significant role. A lack of iron, vitamin B12, or folate, for example, can lead to a higher incidence of mouth sores. Ensuring you have a balanced diet rich in these nutrients is crucial.
- Iron deficiency anemia: Often associated with fatigue and pale skin, this deficiency can manifest as mouth sores.
- Vitamin B12 deficiency: Can cause anemia and neurological symptoms, alongside mouth sores.
- Folate deficiency: Essential for cell growth and development; deficiency can contribute to various health issues, including oral lesions.
Injury or Irritation
Physical trauma to the mouth is a common cause. This can include accidental biting of the cheek or tongue, ill-fitting dentures, or even harsh brushing. Avoiding these irritants and practicing gentle oral hygiene can help prevent future outbreaks.
- Accidental biting: A frequent cause of minor mouth sores that usually heal quickly.
- Dental work: Procedures like fillings or extractions can sometimes lead to temporary sores.
- Aggressive brushing: Using a hard-bristled toothbrush or brushing too vigorously can irritate the gums and inner cheeks.
Viral or Bacterial Infections
While canker sores are not directly caused by viruses or bacteria, certain infections can weaken the immune system, making you more prone to them. Conditions like herpes simplex virus (HSV) can cause oral herpes (cold sores), which are distinct from canker sores but can appear similarly. Good oral hygiene helps to minimize the risk of these infections.
- Herpes simplex virus (HSV): Causes cold sores, which often appear on the lips and differ from canker sores.
- Bacterial infections: While less common, certain bacterial infections can weaken the mouth's defenses.
- Weakened immune system: Underlying illnesses can make individuals more susceptible to both infections and mouth sores.
Certain Medications
Some medications, as a side effect, can increase the likelihood of developing mouth sores. Certain chemotherapy drugs and even some commonly prescribed medications can contribute to the problem. If you suspect medication is a contributing factor, consult your doctor or pharmacist.
- Chemotherapy: Often causes mucositis, a painful inflammation of the mucous membranes in the mouth.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): May sometimes be associated with increased mouth sore incidence.
- Other medications: A few other medications have been anecdotally linked to increased mouth sore occurrences.
What are the symptoms of B12 deficiency in the mouth?
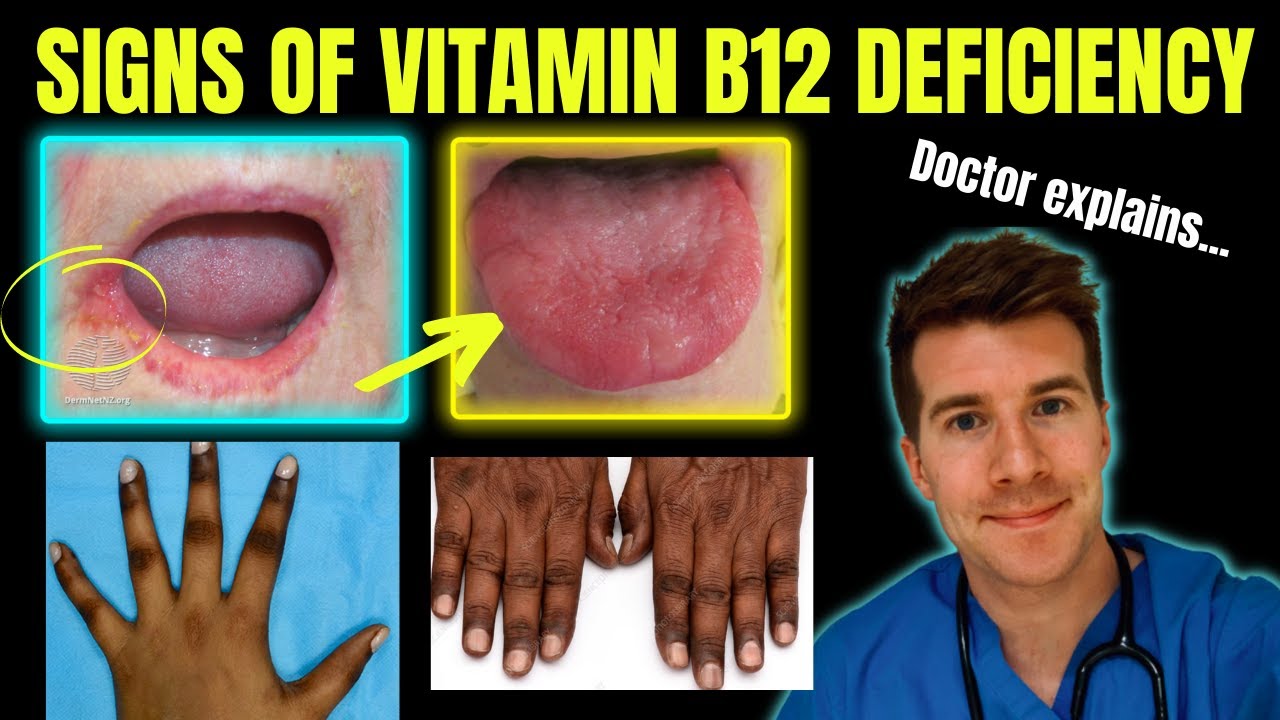
While B12 deficiency primarily affects the nervous and hematopoietic systems, it can manifest in the mouth as well, although these oral manifestations are often subtle and can be easily overlooked or attributed to other causes. The most common oral symptom is glossitis, an inflammation of the tongue. This can present as a smooth, red, and often sore tongue, sometimes with a burning sensation. Other less common symptoms might include dryness of the mouth (xerostomia) and an altered sense of taste (dysgeusia). It's crucial to note that these oral symptoms alone are not diagnostic of B12 deficiency and should be considered in conjunction with other symptoms and blood tests.
1. Glossitis: The Hallmark Sign
Glossitis, characterized by inflammation and soreness of the tongue, is the most frequently reported oral manifestation of vitamin B12 deficiency. The tongue's surface loses its normal bumpy texture, becoming smooth and shiny. This is due to atrophy of the papillae, the small projections that give the tongue its characteristic rough appearance. The color often changes to a deep red or beefy red. Patients may experience discomfort, pain, and even burning sensations, especially when consuming spicy or acidic foods.
- Smooth, shiny tongue: Loss of papillae creates a slick appearance.
- Red or beefy red discoloration: Inflammation causes a change in the tongue's color.
- Pain and burning sensation: Inflammation leads to discomfort, particularly when eating certain foods.
2. Xerostomia: Dry Mouth
Dry mouth, or xerostomia, is another potential oral symptom associated with B12 deficiency. While not exclusive to B12 deficiency, it can occur as a result of the nutritional deficiency's impact on salivary gland function. The reduced saliva production can lead to discomfort, difficulty swallowing, and an increased risk of oral infections. The dryness can make speaking and eating more challenging, further impacting the individual's quality of life. This symptom is often less prominent than glossitis.
- Reduced saliva production: Leading to a persistently dry feeling in the mouth.
- Difficulty swallowing: Dryness makes it harder to move food around the mouth.
- Increased risk of oral infections: Saliva provides a natural defense against infections.
3. Dysgeusia: Altered Taste
Dysgeusia, or a change in taste perception, can be another subtle oral manifestation. Individuals may experience a decreased ability to taste certain flavors, a distortion of taste, or even a metallic or unpleasant taste in the mouth. This altered taste perception can lead to reduced appetite and dietary changes, further exacerbating the B12 deficiency. The exact mechanism linking B12 deficiency to dysgeusia remains unclear but it is believed to relate to the deficiency's effect on nerve function.
- Decreased taste sensitivity: Foods may seem blander or less flavorful.
- Taste distortion: Familiar flavors may taste different or unfamiliar.
- Metallic or unpleasant taste: A persistent abnormal taste in the mouth.
4. Oral Ulcers or Stomatitis: Less Common Manifestations
Although less frequently reported, some individuals with severe B12 deficiency may experience oral ulcers or stomatitis. These are painful sores or inflammation in the mouth. The underlying mechanisms are not fully understood, but they may be linked to the impaired immune function often seen in severe B12 deficiency, leaving the oral mucosa more susceptible to inflammation and ulceration. These are often more indicative of a severe, long-standing deficiency.
- Painful sores or lesions: In the lining of the mouth.
- Inflammation of the oral mucosa: Leading to redness and swelling.
- Impaired immune response: Contributing to increased susceptibility to infection.
5. Delayed Healing: A Potential Sign
Individuals with B12 deficiency may experience delayed healing of oral wounds or lesions. This is due to the critical role B12 plays in cell growth and repair. Any injuries to the mouth, such as minor cuts or abrasions, may take longer to heal than usual. This slower healing process might not be immediately noticed but can be a contributing factor to persistent oral discomfort or infection in B12 deficient patients.
- Slow wound healing: Minor injuries take longer to recover.
- Increased susceptibility to infection: Impairments in tissue repair increases infection risk.
- Persistent oral discomfort: Linked to slow healing and potential infection.
What vitamins are good for mouth ulcers?

While no single vitamin magically cures mouth ulcers (also known as aphthous ulcers or canker sores), several vitamins play crucial roles in maintaining healthy oral mucosa and can help promote healing. A deficiency in certain vitamins can increase your susceptibility to mouth ulcers, making supplementation potentially beneficial for some individuals. It's important to note that treating the underlying cause of the ulcers is essential; vitamins are supportive, not a primary treatment.
The Role of Vitamin B12 in Mouth Ulcer Healing
Vitamin B12 plays a vital role in cell growth and development, including the cells lining your mouth. A deficiency can lead to various problems, including mouth sores. Sufficient B12 levels are crucial for maintaining healthy oral tissues and speeding up the healing process. Supplementation might be beneficial if you suspect a deficiency, but it should be done under the guidance of a healthcare professional.
- Supports cell regeneration in the oral mucosa.
- Reduces inflammation, potentially easing discomfort.
- Aids in the production of red blood cells, improving oxygen delivery to the ulcer site.
Vitamin B Complex and Mouth Ulcers
The B vitamins, particularly B12, B6, and B9 (folic acid), work synergistically to support cell growth and overall oral health. A deficiency in any of these can contribute to increased susceptibility to mouth ulcers. Taking a B-complex vitamin supplement can ensure adequate intake of all these essential nutrients. Consult your doctor before starting any supplements, especially if you are already taking other medications.
- B6 supports immune function, which is crucial for fighting infection.
- Folic acid (B9) is essential for cell division and growth, promoting healing.
- B vitamins work together to ensure healthy tissue formation.
The Importance of Vitamin C for Oral Health
Vitamin C is a powerful antioxidant that plays a vital role in tissue repair and immune function. It aids in collagen production, a protein essential for wound healing. While not a direct cure for mouth ulcers, adequate vitamin C intake can support your body's natural healing processes, making the ulcers heal faster and potentially reducing inflammation. Severe deficiency can lead to scurvy, a condition known to cause gum disease and other oral problems.
- Strengthens blood vessels, improving blood flow to the ulcer.
- Supports immune function to fight infection and reduce inflammation.
- Aids in collagen synthesis which is crucial for tissue repair.
Iron and Mouth Ulcers: A Connection
Iron deficiency anemia is a common cause of several health problems, and mouth ulcers can be one of the symptoms. Iron is a key component of hemoglobin, which carries oxygen throughout the body, including the tissues in your mouth. Low iron levels can impair healing, increasing the duration and severity of mouth ulcers. If you suspect an iron deficiency, it's crucial to address this issue with your healthcare provider.
- Supports red blood cell production, ensuring adequate oxygen delivery to the ulcer site.
- Improves overall tissue health and repair.
- Addressing iron deficiency is crucial for effective mouth ulcer healing.
Zinc's Role in Mouth Ulcer Healing
Zinc is a mineral that's essential for numerous bodily functions, including immune function and cell growth. It plays a crucial role in wound healing and can help to reduce inflammation. While research on zinc's direct effect on mouth ulcers is limited, it's considered a helpful component in overall oral health and wound healing, therefore adequate intake may support faster healing times. A deficiency may slow down the healing process.
- Supports immune system function, helping to fight off infection.
- Promotes wound healing by reducing inflammation and supporting cell regeneration.
- Acts as an antioxidant, protecting cells from damage.
What are the most common vitamin deficiencies that cause mouth sores?
Mouth sores, also known as aphthous ulcers or canker sores, can be triggered by a variety of factors, and vitamin deficiencies are among them. While not all mouth sores are directly caused by vitamin deficiency, several B vitamins play a crucial role in maintaining the health of the oral mucosa. Vitamin B12 deficiency is a particularly strong suspect, as it's essential for cell growth and repair, including the cells lining the mouth. A deficiency can lead to various symptoms, including mouth sores, alongside other neurological and hematological issues. Similarly, a folate (vitamin B9) deficiency can also contribute to mouth sores. Folate is vital for cell division and DNA synthesis, and a shortage can impact the rapid turnover of cells in the mouth, making them more susceptible to ulceration. Iron deficiency, though not strictly a vitamin deficiency, is also frequently linked to mouth sores. Iron is a key component of hemoglobin, responsible for oxygen transport throughout the body. Low iron levels can lead to impaired cell function and increased susceptibility to infections, including oral infections which manifest as mouth sores. It is important to note that mouth sores stemming from vitamin deficiencies usually appear alongside other symptoms related to the specific deficiency. If you suspect a vitamin deficiency is causing your mouth sores, it is crucial to consult a doctor for proper diagnosis and treatment, rather than self-treating.
Can iron deficiency anemia cause mouth sores?
Yes, iron deficiency anemia is frequently associated with the development of mouth sores. While not every case of mouth sores is caused by iron deficiency, it's a significant contributing factor for many individuals. Iron plays a critical role in the production of red blood cells and the transport of oxygen throughout the body. When iron levels are low, the body's ability to produce healthy cells, including those lining the mouth, is compromised. This impaired cell function makes the oral mucosa more vulnerable to injury and slower to heal, leading to the formation of mouth sores. These sores often appear as small, shallow ulcers that can be painful and may bleed easily. Furthermore, iron deficiency anemia often presents with other symptoms, such as fatigue, weakness, pale skin, and shortness of breath. If you experience mouth sores along with these symptoms, it's vital to seek medical attention. A simple blood test can determine your iron levels and help diagnose iron deficiency anemia. Treatment typically involves iron supplements and dietary adjustments to increase iron intake. Addressing the underlying iron deficiency is crucial not only for healing the mouth sores but also for improving overall health.
Besides vitamins, are there other nutritional deficiencies that can lead to mouth sores?
While vitamin deficiencies are commonly linked to mouth sores, other nutritional deficiencies can also play a role. A deficiency in zinc, for example, can impair the body's immune response and wound healing processes. Since mouth sores represent a type of wound in the oral mucosa, a zinc deficiency can hinder their healing and potentially exacerbate their formation. Vitamin C deficiency (scurvy) is another example. Although less commonly associated with mouth sores alone, severe vitamin C deficiency can cause various oral issues including bleeding gums, and can also increase the susceptibility to infections and inflammation that could ultimately contribute to mouth sores. Moreover, deficiencies in essential fatty acids can affect the integrity of cell membranes, making the oral mucosa more fragile and prone to ulceration. It's important to understand that nutritional deficiencies often occur in combination. For instance, iron deficiency anemia frequently coexists with other deficiencies like folate and vitamin B12. This makes it crucial to have a thorough nutritional assessment if you're experiencing recurrent or persistent mouth sores. It's advisable to consult a healthcare professional or registered dietitian to determine if a broader nutritional imbalance could be contributing to your oral health problems.
How can I tell if my mouth sores are due to a deficiency versus another cause?
Differentiating between mouth sores caused by a deficiency and those caused by other factors can be challenging, and requires professional medical assessment. While vitamin or mineral deficiencies can be a contributing factor, many other things can cause mouth sores, including minor injuries, stress, hormonal changes, certain medications, or infections. Simply having mouth sores doesn't automatically indicate a deficiency. However, several clues might suggest a potential link to nutritional deficiencies. If your mouth sores are recurrent, persistent, and accompanied by other symptoms like fatigue, pallor (pale skin), shortness of breath, or neurological issues, a deficiency is more likely. Also, if your diet is known to be poor in fruits, vegetables, and other nutrient-rich foods, a deficiency is a stronger possibility. Nevertheless, self-diagnosing can be misleading and dangerous. The best way to determine the cause of your mouth sores is to consult a doctor or dentist. They can assess your medical history, perform a physical examination, and possibly order blood tests to check your vitamin, mineral, and iron levels. Early diagnosis and treatment of any underlying deficiency is vital for healing the mouth sores and preventing further health complications.
Deja una respuesta