What deficiency causes mouth ulcers
Mouth ulcers are a common and painful problem that can affect people of all ages. They can be caused by a variety of factors, including stress, hormonal changes, and certain medical conditions. One of the most common causes of mouth ulcers is a deficiency of certain vitamins and minerals.
What Nutritional Deficiencies Cause Mouth Ulcers?
Mouth ulcers, also known as aphthous ulcers or canker sores, are small, painful sores that develop inside the mouth. While the exact cause isn't always known, several nutritional deficiencies can contribute to their formation or exacerbate their frequency and severity. A healthy diet rich in various nutrients is crucial for maintaining oral health and reducing the risk of mouth ulcers.
Iron Deficiency
Iron deficiency anemia is a common cause of mouth ulcers. Iron is essential for the production of red blood cells, which carry oxygen throughout the body. When iron levels are low, the body's ability to repair tissues, including the oral mucosa, is compromised. This can lead to the development of mouth ulcers and other symptoms like fatigue, weakness, and pale skin. Ensuring adequate iron intake through a balanced diet, including iron-rich foods like red meat, spinach, and lentils, or through supplementation under a doctor's guidance, can help prevent iron deficiency-related mouth ulcers.
Vitamin B12 Deficiency
Vitamin B12 plays a crucial role in cell growth and development, including the maintenance of healthy oral tissues. A deficiency in vitamin B12 can lead to various symptoms, including mouth ulcers. This vitamin is primarily found in animal products like meat, poultry, fish, and dairy. Vegans and vegetarians are at a higher risk of B12 deficiency and may need to supplement to prevent mouth ulcers and other related health issues. Symptoms of B12 deficiency can be subtle initially and might not include mouth ulcers, but fatigue, numbness, and tingling are common.
Folate Deficiency
Folate, also known as vitamin B9, is another essential B vitamin involved in cell growth and DNA synthesis. A folate deficiency can disrupt the normal repair processes of the body, leading to mouth ulcers. Good sources of folate include leafy green vegetables, legumes, and citrus fruits. Pregnant women are particularly vulnerable to folate deficiency and should ensure adequate intake to prevent neural tube defects and other health complications, including possible mouth ulcer development.
Vitamin C Deficiency
Vitamin C is a powerful antioxidant that plays a vital role in wound healing and immune function. A deficiency in vitamin C can weaken the immune system and impair tissue repair, leading to increased susceptibility to mouth ulcers. This is because vitamin C promotes collagen synthesis, a key component of connective tissue that plays a significant role in wound healing. Eating plenty of fruits and vegetables rich in vitamin C can help prevent deficiency and potential mouth ulcer development.
Zinc Deficiency
Zinc is a mineral essential for various bodily functions, including cell growth, wound healing, and immune response. A zinc deficiency can lead to a weakened immune system, making the body more susceptible to infections and slower to heal injuries, potentially resulting in more frequent or severe mouth ulcers. Zinc is found in various foods, including oysters, red meat, poultry, beans, and nuts. However, individuals with certain medical conditions or those following restrictive diets may require zinc supplementation to prevent deficiency-related issues like mouth ulcers.
| Nutrient Deficiency | Symptoms (Beyond Mouth Ulcers) | Food Sources |
|---|---|---|
| Iron | Fatigue, weakness, pale skin, shortness of breath | Red meat, spinach, lentils, beans |
| Vitamin B12 | Fatigue, weakness, numbness, tingling, pale skin | Meat, poultry, fish, dairy, eggs (supplements for vegans/vegetarians) |
| Folate | Fatigue, weakness, pale skin, shortness of breath | Leafy green vegetables, legumes, citrus fruits |
| Vitamin C | Fatigue, weakness, bleeding gums, easy bruising | Citrus fruits, berries, tomatoes, peppers |
| Zinc | Slow wound healing, hair loss, diarrhea, loss of appetite | Oysters, red meat, poultry, beans, nuts |
What Nutritional Deficiencies Cause Mouth Ulcers?
Mouth ulcers, also known as aphthous ulcers or canker sores, are small, painful sores that develop inside the mouth. While the exact cause isn't always known, several nutritional deficiencies can contribute to their formation or exacerbate their frequency and severity. A healthy diet rich in various nutrients is crucial for maintaining oral health and reducing the risk of mouth ulcers.
Iron Deficiency
Iron deficiency anemia is a common cause of mouth ulcers. Iron is essential for the production of red blood cells, which carry oxygen throughout the body. When iron levels are low, the body's ability to repair tissues, including the oral mucosa, is compromised. This can lead to the development of mouth ulcers and other symptoms like fatigue, weakness, and pale skin. Ensuring adequate iron intake through a balanced diet, including iron-rich foods like red meat, spinach, and lentils, or through supplementation under a doctor's guidance, can help prevent iron deficiency-related mouth ulcers.
Vitamin B12 Deficiency
Vitamin B12 plays a crucial role in cell growth and development, including the maintenance of healthy oral tissues. A deficiency in vitamin B12 can lead to various symptoms, including mouth ulcers. This vitamin is primarily found in animal products like meat, poultry, fish, and dairy. Vegans and vegetarians are at a higher risk of B12 deficiency and may need to supplement to prevent mouth ulcers and other related health issues. Symptoms of B12 deficiency can be subtle initially and might not include mouth ulcers, but fatigue, numbness, and tingling are common.
Folate Deficiency
Folate, also known as vitamin B9, is another essential B vitamin involved in cell growth and DNA synthesis. A folate deficiency can disrupt the normal repair processes of the body, leading to mouth ulcers. Good sources of folate include leafy green vegetables, legumes, and citrus fruits. Pregnant women are particularly vulnerable to folate deficiency and should ensure adequate intake to prevent neural tube defects and other health complications, including possible mouth ulcer development.
Vitamin C Deficiency
Vitamin C is a powerful antioxidant that plays a vital role in wound healing and immune function. A deficiency in vitamin C can weaken the immune system and impair tissue repair, leading to increased susceptibility to mouth ulcers. This is because vitamin C promotes collagen synthesis, a key component of connective tissue that plays a significant role in wound healing. Eating plenty of fruits and vegetables rich in vitamin C can help prevent deficiency and potential mouth ulcer development.
Zinc Deficiency
Zinc is a mineral essential for various bodily functions, including cell growth, wound healing, and immune response. A zinc deficiency can lead to a weakened immune system, making the body more susceptible to infections and slower to heal injuries, potentially resulting in more frequent or severe mouth ulcers. Zinc is found in various foods, including oysters, red meat, poultry, beans, and nuts. However, individuals with certain medical conditions or those following restrictive diets may require zinc supplementation to prevent deficiency-related issues like mouth ulcers.
| Nutrient Deficiency | Symptoms (Beyond Mouth Ulcers) | Food Sources |
|---|---|---|
| Iron | Fatigue, weakness, pale skin, shortness of breath | Red meat, spinach, lentils, beans |
| Vitamin B12 | Fatigue, weakness, numbness, tingling, pale skin | Meat, poultry, fish, dairy, eggs (supplements for vegans/vegetarians) |
| Folate | Fatigue, weakness, pale skin, shortness of breath | Leafy green vegetables, legumes, citrus fruits |
| Vitamin C | Fatigue, weakness, bleeding gums, easy bruising | Citrus fruits, berries, tomatoes, peppers |
| Zinc | Slow wound healing, hair loss, diarrhea, loss of appetite | Oysters, red meat, poultry, beans, nuts |
What am I lacking if I get mouth ulcers?

Mouth ulcers, also known as aphthous ulcers or canker sores, can be caused by a variety of factors, and while a deficiency in specific nutrients isn't always the sole cause, several deficiencies are frequently associated with their development or increased frequency. The exact reason why someone gets mouth ulcers is often complex and multifactorial, meaning it involves a combination of different contributing elements. It's not simply a matter of lacking one specific thing. However, certain deficiencies are more frequently implicated than others. If you experience frequent or severe mouth ulcers, it's crucial to consult a doctor or dentist to rule out underlying medical conditions and to determine if dietary changes or supplementation might be beneficial.
Vitamin B12 Deficiency
Vitamin B12 plays a crucial role in cell growth and development, including the cells lining the mouth. A deficiency can lead to various health problems, and mouth ulcers are a common symptom. Insufficient B12 can impair the body's ability to repair damaged tissues, potentially leading to the formation and persistence of ulcers. It's important to note that a B12 deficiency often presents with other symptoms beyond mouth ulcers, such as fatigue, anemia, and neurological problems.
- Symptoms of B12 deficiency: Fatigue, weakness, pale skin, shortness of breath, heart palpitations, constipation, neurological issues like tingling or numbness in extremities.
- Sources of B12: Animal products such as meat, poultry, fish, eggs, and dairy products.
- Treatment: B12 supplements, often administered via injection or sublingual tablets, are commonly used to address deficiencies.
Iron Deficiency
Iron is essential for red blood cell production and oxygen transport. An iron deficiency, leading to anemia, can weaken the immune system and make you more susceptible to infections and inflammation, which can contribute to the development of mouth ulcers. Iron deficiency can also slow down the healing process, leading to longer-lasting ulcers. However, iron deficiency often manifests with other symptoms before mouth ulcers become prominent.
- Symptoms of iron deficiency: Fatigue, weakness, pale skin, shortness of breath, dizziness, cold hands and feet, brittle nails.
- Sources of iron: Red meat, spinach, beans, lentils, fortified cereals.
- Treatment: Iron supplements are often prescribed to treat iron deficiency anemia, but their use should be guided by a healthcare professional.
Folic Acid Deficiency
Folic acid, a B vitamin, is vital for cell growth and DNA synthesis. A deficiency can hinder the body's ability to repair damaged tissues and maintain healthy oral mucosa. Similar to B12 deficiency, a lack of folic acid can lead to impaired cell regeneration in the mouth, potentially increasing susceptibility to mouth ulcers. It's often seen in combination with other deficiencies.
- Symptoms of folic acid deficiency: Fatigue, weakness, pale skin, headaches, shortness of breath, mouth sores, diarrhea.
- Sources of folic acid: Leafy green vegetables, legumes, citrus fruits, fortified grains.
- Treatment: Folic acid supplements are readily available, but consulting a doctor is advised before starting any supplementation.
Zinc Deficiency
Zinc plays a critical role in immune function and wound healing. A zinc deficiency can impair the body's ability to fight off infections and repair damaged tissues, potentially making you more prone to developing mouth ulcers and slowing down the healing process. It is also often associated with other immune-related issues.
- Symptoms of zinc deficiency: Impaired immune function, slow wound healing, loss of appetite, diarrhea, hair loss.
- Sources of zinc: Oysters, red meat, poultry, beans, nuts, seeds.
- Treatment: Zinc supplements are available but should be taken under the guidance of a healthcare professional to avoid potential side effects.
Vitamin C Deficiency
Vitamin C is an essential antioxidant crucial for collagen production, a protein vital for tissue repair. A deficiency can impair wound healing, potentially prolonging the duration and severity of mouth ulcers. While scurvy, the severe form of vitamin C deficiency, is rare, milder deficiencies can still impact the body's ability to heal effectively.
- Symptoms of Vitamin C deficiency: Fatigue, weakness, bleeding gums, easy bruising, joint pain, slow wound healing.
- Sources of Vitamin C: Citrus fruits, berries, kiwi, peppers, broccoli.
- Treatment: Vitamin C supplements are easily accessible, but it's best to consult a healthcare professional to determine the appropriate dosage.
What vitamin stops mouth ulcers?

There isn't one single vitamin that definitively "stops" mouth ulcers (also known as aphthous ulcers or canker sores). However, deficiencies in certain vitamins and minerals are linked to an increased risk of developing them, and supplementing with these can sometimes help reduce their frequency and severity. Vitamin B12 is often cited, along with folate (vitamin B9) and iron. These nutrients play crucial roles in cell growth and repair, and deficiencies can impair the body's ability to heal these sores. It's important to note that while supplementation might be beneficial for some, it's not a guaranteed cure, and the underlying cause of the ulcers needs to be addressed. Other factors like stress, hormonal changes, and injury to the mouth can also contribute.
The Role of Vitamin B12 in Mouth Ulcer Prevention
Vitamin B12 is essential for DNA synthesis and red blood cell formation. A deficiency can lead to various health problems, including mouth ulcers. Maintaining adequate B12 levels can contribute to faster healing and fewer outbreaks. Supplementation is often recommended in cases of deficiency or suspected deficiency, but it's crucial to consult a doctor before starting any supplement regime.
- B12 deficiency symptoms often include fatigue, pallor, and neurological issues alongside mouth ulcers.
- Rich sources of B12 include meat, poultry, fish, eggs, and dairy products.
- B12 supplements come in various forms, such as injections, sublingual tablets, and oral capsules.
The Importance of Folate (Vitamin B9) for Oral Health
Folate is another B vitamin vital for cell growth and repair. Insufficient folate can interfere with the body's natural healing process, making mouth ulcers more likely and persistent. Ensuring adequate intake of folate through diet or supplementation can help promote faster healing and reduce the recurrence of mouth ulcers.
- Folate deficiency can lead to anemia and other health complications.
- Good dietary sources of folate include leafy green vegetables, legumes, and citrus fruits.
- Folic acid is the synthetic form of folate used in supplements and fortified foods.
Iron's Contribution to Mouth Ulcer Healing
Iron plays a crucial role in oxygen transport throughout the body. Iron deficiency anemia can impair the healing process and increase susceptibility to mouth ulcers. While iron isn't directly involved in ulcer formation, addressing any iron deficiency can positively impact overall healing and reduce the frequency of occurrences.
- Iron deficiency anemia can manifest with fatigue, weakness, and pale skin in addition to mouth ulcers.
- Heme iron, found in animal products, is more readily absorbed than non-heme iron found in plants.
- Vitamin C enhances the absorption of non-heme iron.
Other Vitamins and Minerals Involved in Mouth Ulcer Healing
While B12, folate, and iron are most commonly associated with mouth ulcer prevention, other nutrients also play a supporting role. Zinc, vitamin C, and riboflavin (B2) are involved in various aspects of tissue repair and immune function, potentially contributing to faster healing of mouth ulcers.
- Zinc is involved in cell growth and immune function.
- Vitamin C is an antioxidant that supports tissue repair.
- Riboflavin (B2) contributes to cellular energy production.
When to Seek Professional Medical Advice
If you experience frequent, severe, or persistent mouth ulcers, it is crucial to consult a doctor or dentist. Recurring mouth ulcers might indicate an underlying medical condition that requires attention. A healthcare professional can help determine the cause of your ulcers and recommend appropriate treatment or management strategies, including possibly testing for vitamin deficiencies.
- Persistent mouth ulcers may require a biopsy to rule out more serious conditions.
- Underlying medical conditions like Crohn's disease and Behçet's disease can be linked to mouth ulcers.
- Medication side effects can sometimes cause mouth ulcers.
How do you feel if your B12 is low?
:max_bytes(150000):strip_icc()/vitamin-b12-deficiency-2488570_final-f6046c0de6114c14a488433ca2b19142.jpg)
Low vitamin B12 levels, also known as vitamin B12 deficiency, can manifest in a wide range of symptoms, some subtle and others quite debilitating. The severity of symptoms depends on the severity and duration of the deficiency. Many individuals with mild deficiencies might experience no noticeable symptoms at all, while others with more significant deficiencies can experience a constellation of problems. It's important to note that these symptoms can mimic other conditions, making diagnosis crucial. A blood test is the only definitive way to determine if your B12 levels are low.
Fatigue and Weakness
One of the most common symptoms of low B12 is persistent fatigue and unexplained weakness. This is because B12 plays a vital role in energy production. When your B12 levels are low, your body struggles to produce enough energy to meet its demands, leading to feelings of tiredness and a lack of strength, even after adequate rest. This fatigue can be significant, impacting daily activities and quality of life.
- Extreme tiredness: Even after a full night's sleep, you may feel excessively drained.
- Muscle weakness: You might experience weakness in your limbs or body, making everyday tasks more challenging.
- Reduced stamina: Simple activities that you could normally do with ease now seem strenuous.
Neurological Symptoms
Vitamin B12 is essential for the proper functioning of the nervous system. A deficiency can lead to a variety of neurological problems. These symptoms can range from mild to severe, and may include cognitive impairment, nerve damage, and even psychiatric issues. Early diagnosis and treatment are vital to prevent permanent neurological damage.
- Numbness and tingling: These sensations may occur in the extremities (hands and feet) or other parts of the body.
- Cognitive difficulties: This can manifest as memory loss, difficulty concentrating, confusion, and even dementia in severe cases.
- Balance problems and dizziness: Ataxia, or impaired coordination, can result from nerve damage.
Gastrointestinal Issues
While not always present, digestive problems can be associated with low B12. These problems can include loss of appetite, nausea, vomiting, diarrhea, or constipation. The gastrointestinal tract plays a significant role in B12 absorption, so issues here can contribute to or worsen a deficiency. Changes in bowel habits should be investigated by a healthcare professional.
- Loss of appetite: You might find yourself eating less than usual, without feeling particularly full.
- Diarrhea or constipation: Changes in bowel movements can be a sign of several health issues, including B12 deficiency.
- Nausea and vomiting: These symptoms can be especially noticeable in cases of severe deficiency.
Pale Skin and Shortness of Breath
Low B12 can lead to anemia, which is a deficiency in red blood cells. This can result in pale skin, as red blood cells are responsible for giving skin its color. The reduced number of red blood cells also makes it harder for your blood to carry oxygen effectively, potentially causing shortness of breath, especially during physical activity. Pernicious anemia, a specific type of B12 deficiency, often manifests with these symptoms.
- Pallor: A noticeable paleness in the skin, especially noticeable in the gums and inner eyelids.
- Shortness of breath: Difficulty breathing, especially during exertion.
- Rapid heartbeat: Your heart may beat faster than normal to try to compensate for low oxygen levels.
Paresthesia
Paresthesia refers to abnormal sensations, such as tingling, prickling, or numbness. In the context of B12 deficiency, these sensations often occur in the extremities (hands and feet), but can also affect other parts of the body. The abnormal sensations are often described as pins and needles or burning. These sensations are a result of nerve damage caused by the deficiency.
- Tingling sensations: A feeling of pins and needles in the hands, feet, or other body parts.
- Numbness: A loss of feeling or sensation in affected areas.
- Burning or prickling sensations: A burning or prickling feeling in the skin.
Can low vitamin D cause mouth sores?

While a direct causal link between low vitamin D and mouth sores hasn't been definitively established through extensive research, there's evidence suggesting a possible correlation. Low vitamin D levels are associated with a weakened immune system. A compromised immune system can increase susceptibility to various infections, including those that might manifest as mouth sores. It's important to understand that mouth sores have numerous potential causes, and low vitamin D is just one possible contributing factor among many. More research is needed to fully understand the relationship.
Vitamin D's Role in Immune Function
Vitamin D plays a crucial role in regulating the immune system. It influences the production and activity of immune cells, including those responsible for fighting off infections in the mouth. A deficiency in vitamin D can impair immune function, potentially making individuals more vulnerable to oral infections that can lead to sores. This doesn't directly cause the sores, but it can create an environment where they're more likely to develop.
- Reduced immune response: Low vitamin D levels can suppress the activity of immune cells, hindering their ability to eliminate pathogens.
- Increased susceptibility to infections: A weaker immune system makes individuals more prone to various infections, including those affecting the oral cavity.
- Slower healing: Vitamin D is involved in the wound healing process. A deficiency could slow the healing of mouth sores.
Other Potential Causes of Mouth Sores
It's crucial to remember that mouth sores (oral ulcers) have a wide range of causes. Attributing them solely to vitamin D deficiency is often an oversimplification. Other common causes include: viral infections (like herpes simplex virus), bacterial infections, fungal infections (like thrush), trauma (e.g., biting your cheek), allergies, certain autoimmune diseases, and even stress. A proper diagnosis requires considering all potential factors.
- Viral infections: Herpes simplex virus is a common cause of cold sores.
- Bacterial infections: Certain bacteria can cause mouth infections and ulcers.
- Fungal infections: Candidiasis (thrush) is a fungal infection that can manifest as oral lesions.
The Importance of Proper Diagnosis
If you're experiencing mouth sores, it's essential to seek professional medical advice for a proper diagnosis. Self-diagnosing and treating based solely on suspected vitamin D deficiency can be risky. A healthcare professional can perform a thorough examination, consider your medical history, and order appropriate tests (including vitamin D levels) to determine the underlying cause of your mouth sores and recommend the best course of action.
- Physical examination: A doctor will visually examine the mouth sores to assess their characteristics.
- Medical history review: Your medical history can provide clues about potential causes.
- Laboratory tests: Blood tests might be necessary to determine vitamin D levels and screen for other conditions.
Treating Mouth Sores and Vitamin D Deficiency
Treatment for mouth sores depends entirely on the underlying cause. If a vitamin D deficiency is identified as a contributing factor (or if a deficiency exists independently), supplementation may be recommended. However, it's crucial to remember that vitamin D supplementation alone won't necessarily cure mouth sores caused by other factors. Treatment might involve antiviral, antibacterial, or antifungal medications, depending on the diagnosis. Proper oral hygiene is also crucial for preventing and managing mouth sores.
- Vitamin D supplementation: If a deficiency is confirmed, a doctor will determine the appropriate dosage.
- Targeted treatments: Antiviral, antibacterial, or antifungal medications might be prescribed based on the specific infection.
- Oral hygiene: Maintaining good oral hygiene practices can help prevent many oral health problems.
Further Research and Considerations
While the relationship between low vitamin D and mouth sores warrants further investigation, current evidence doesn't establish a definitive causal link. More research is needed to clarify this association. In the meantime, maintaining adequate vitamin D levels through diet, sun exposure (with appropriate protection), and/or supplementation (as advised by a healthcare professional) is essential for overall health and immune function. However, it's not a guaranteed solution for mouth sores.
- Larger-scale studies: More research is needed to confirm or refute a link between low vitamin D and mouth sores.
- Longitudinal studies: Studies tracking individuals over time could provide valuable insights.
- Mechanism of action: Future research should investigate the potential mechanisms through which vitamin D might influence the development of mouth sores.
What are the most common causes of mouth ulcers?
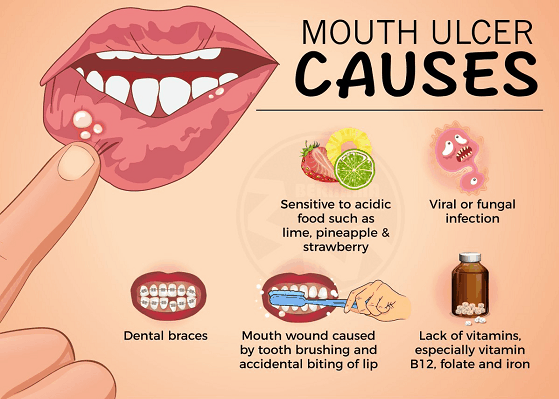
Mouth ulcers, also known as aphthous ulcers or canker sores, are small, painful sores that develop inside the mouth. While the exact cause remains unknown, several factors are strongly linked to their development. Stress is a significant trigger for many individuals, leading to a weakened immune system that makes them more susceptible to these lesions. Nutritional deficiencies, particularly in iron, vitamin B12, folate, and zinc, can also contribute to mouth ulcer formation. A deficiency in these essential nutrients can impair the body's ability to repair damaged tissues, prolonging healing time and increasing the likelihood of recurrent ulcers. Minor injuries to the mouth, such as biting your cheek accidentally, using harsh toothpastes, or ill-fitting dentures, can also initiate ulcer formation. Certain medical conditions, including inflammatory bowel disease (IBD), celiac disease, and Behçet's disease, are associated with a heightened risk of developing mouth ulcers. Finally, some people experience mouth ulcers as a side effect of certain medications. It's important to note that multiple factors can interact to trigger mouth ulcers, and what works for one person may not work for another.
Can vitamin deficiencies actually cause mouth ulcers?
Yes, deficiencies in certain vitamins and minerals are strongly linked to the development and recurrence of mouth ulcers. Vitamin B12 deficiency is a common culprit, as B12 plays a crucial role in cell growth and repair. Without adequate B12, the body struggles to heal damaged tissues, including the oral mucosa where mouth ulcers form. Similarly, a deficiency in folic acid (folate) can impair cell regeneration, leading to a higher susceptibility to ulcers. Iron deficiency is another significant factor, as iron is vital for red blood cell production and oxygen transport. Reduced oxygen delivery to the tissues can impede healing and contribute to ulcer formation. Zinc deficiency also plays a part, as zinc is essential for immune function and wound healing. A deficiency in zinc can weaken the body's defense mechanisms and prolong the healing process. While a deficiency in any of these nutrients can increase your risk, it’s often a combination of factors rather than a single deficiency that's to blame for developing mouth ulcers. Addressing nutritional deficiencies through dietary changes or supplementation, under the guidance of a healthcare professional, can significantly reduce the frequency and severity of mouth ulcers.
Are there specific foods to avoid if I have mouth ulcers?
While there's no single food guaranteed to cause mouth ulcers, certain foods can irritate existing ulcers or make them worse. Acidic foods, such as citrus fruits (oranges, lemons, limes), tomatoes, and vinegar, can cause a burning sensation and prolong healing. Spicy foods can also irritate the delicate tissues of the mouth, leading to increased pain and discomfort. Salty foods can exacerbate the pain and inflammation associated with mouth ulcers. Rough or crunchy foods that may scratch or abrade the ulcer should also be avoided, including chips, crackers, and certain nuts. It's crucial to focus on a soft, bland diet during an outbreak to minimize irritation. This might include well-cooked vegetables, mashed potatoes, yogurt, and smoothies. Staying hydrated by drinking plenty of water is also important to aid in healing. Remember that individual sensitivities vary, so keep a food diary to identify any specific triggers you might have. Consulting with a dietitian or nutritionist can offer personalized dietary recommendations to support oral health.
What should I do if I suspect a nutritional deficiency is causing my mouth ulcers?
If you suspect that a nutritional deficiency might be contributing to your mouth ulcers, it's crucial to seek professional medical advice. Don't attempt to self-diagnose or self-treat. A doctor or registered dietitian can perform a thorough evaluation, including a review of your medical history, dietary habits, and a physical examination. They may order blood tests to assess your levels of iron, vitamin B12, folate, and zinc. Based on the test results, they can determine if you have any deficiencies and recommend appropriate treatment options. This might involve dietary changes to increase your intake of nutrient-rich foods or supplementation to address specific deficiencies. Iron supplements might be prescribed for iron deficiency anemia, while vitamin B12 injections or supplements may be recommended for B12 deficiency. Remember that taking supplements without medical supervision can be harmful, so always consult a healthcare professional before starting any new supplements. A comprehensive approach that addresses both the underlying nutritional deficiencies and the management of mouth ulcers will lead to the best outcome.
Deja una respuesta