What do autoimmune mouth sores look like

Autoimmune mouth sores, also known as aphthous ulcers, are a common and painful condition that affects many people. They can be caused by a variety of factors, including stress, certain foods, and medications. While autoimmune mouth sores are not contagious, they can be very uncomfortable and interfere with daily activities.
What Do Autoimmune Mouth Sores Look Like?
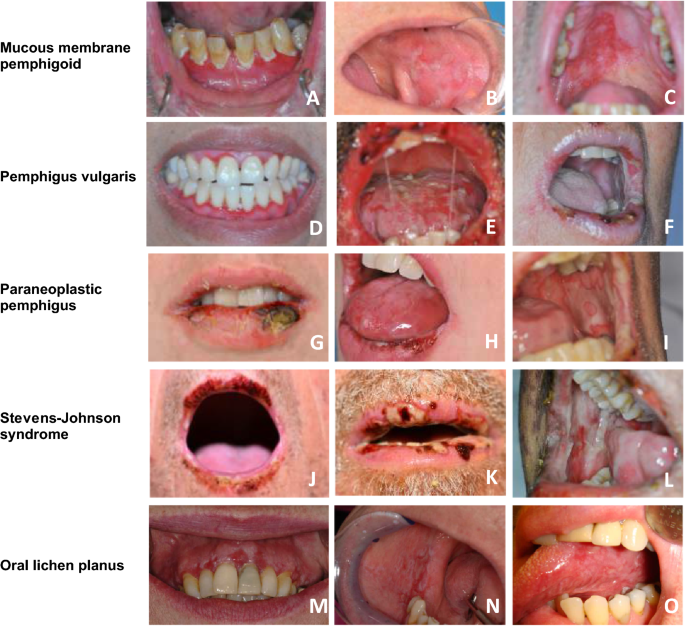
Autoimmune mouth sores, often linked to conditions like Behçet's disease, lupus, or Crohn's disease, can manifest in various ways. They don't have a single, definitive appearance, but rather a range of potential presentations. The key is to recognize the patterns and characteristics that distinguish them from other types of mouth sores, such as canker sores or cold sores (herpes simplex). It's crucial to consult a doctor or dentist for proper diagnosis and treatment, as autoimmune mouth sores can indicate underlying health issues.
Appearance and Location of Autoimmune Mouth Sores
Autoimmune mouth sores can vary significantly in appearance. They can be small and pinpoint-sized, or large and ulcerated, often appearing as shallow or deep lesions. Their location can also vary. While they might appear on the tongue, gums, inner cheeks, or lips, they can also present on the palate (roof of the mouth) or even deeper within the mouth. Unlike canker sores, which often appear singly, autoimmune mouth sores can occur individually or in clusters. Their edges may be well-defined or irregular, and they can be surrounded by redness or swelling.
Color and Texture of Autoimmune Mouth Sores
The color of autoimmune mouth sores can range from pale pink to bright red, and even yellowish or greyish-white in some cases. The texture of the sores is also variable. Some may be smooth and flat, while others may be raised and bumpy, or even covered with a yellowish-white membrane. The sores often feel tender or painful to the touch, and some individuals report a burning sensation. The texture and color can help distinguish them from other types of mouth sores.
Pain and Discomfort Associated with Autoimmune Mouth Sores
Pain is a common symptom associated with autoimmune mouth sores. The intensity of pain can vary significantly depending on the size, location, and severity of the sores. Some people experience mild discomfort, while others have severe pain that can make eating, drinking, and speaking difficult. The pain may be accompanied by burning, tingling, or itching sensations. In cases of severe pain, over-the-counter pain relievers or prescription medications may be necessary.
Healing Time and Recurrence of Autoimmune Mouth Sores
The healing time for autoimmune mouth sores varies greatly, depending on the underlying condition and the severity of the sores. Some sores may heal within a few days, while others may persist for several weeks or even months. A concerning characteristic of these sores is their tendency to recur. This recurring nature is a key distinguishing feature from other types of mouth sores. Regular follow-up with a healthcare provider is essential to monitor healing and manage potential recurrences.
Distinguishing Autoimmune Mouth Sores from Other Mouth Sores
It is vital to distinguish autoimmune mouth sores from other, more common types of mouth sores. Canker sores are usually smaller, shallower, and heal faster. Cold sores (herpes simplex) are typically clustered blisters that appear on the lips or surrounding area and are caused by a virus. Oral thrush (candidiasis) appears as white patches. The duration, recurrence, location, and associated symptoms are crucial for differentiating autoimmune mouth sores from other types of mouth lesions. A healthcare professional can make the correct diagnosis.
| Characteristic | Autoimmune Mouth Sore | Other Mouth Sores (e.g., Canker Sore, Cold Sore) |
|---|---|---|
| Appearance | Variable; shallow or deep ulcers, various sizes, may cluster | Usually smaller, more defined; blisters for cold sores, white patches for thrush |
| Location | Tongue, gums, cheeks, lips, palate | Typically lips (cold sores), inner cheeks (canker sores) |
| Pain | Variable; can be severe | Mild to moderate; usually less intense than autoimmune sores |
| Recurrence | Frequent recurrence common | Less frequent recurrence; cold sores may recur |
| Healing Time | Variable; can be prolonged | Usually faster healing |
What Do Autoimmune Mouth Sores Look Like?
Autoimmune mouth sores, often linked to conditions like Behçet's disease, lupus, or Crohn's disease, can manifest in various ways. They don't have a single, definitive appearance, but rather a range of potential presentations. The key is to recognize the patterns and characteristics that distinguish them from other types of mouth sores, such as canker sores or cold sores (herpes simplex). It's crucial to consult a doctor or dentist for proper diagnosis and treatment, as autoimmune mouth sores can indicate underlying health issues.
Appearance and Location of Autoimmune Mouth Sores
Autoimmune mouth sores can vary significantly in appearance. They can be small and pinpoint-sized, or large and ulcerated, often appearing as shallow or deep lesions. Their location can also vary. While they might appear on the tongue, gums, inner cheeks, or lips, they can also present on the palate (roof of the mouth) or even deeper within the mouth. Unlike canker sores, which often appear singly, autoimmune mouth sores can occur individually or in clusters. Their edges may be well-defined or irregular, and they can be surrounded by redness or swelling.
Color and Texture of Autoimmune Mouth Sores
The color of autoimmune mouth sores can range from pale pink to bright red, and even yellowish or greyish-white in some cases. The texture of the sores is also variable. Some may be smooth and flat, while others may be raised and bumpy, or even covered with a yellowish-white membrane. The sores often feel tender or painful to the touch, and some individuals report a burning sensation. The texture and color can help distinguish them from other types of mouth sores.
Pain and Discomfort Associated with Autoimmune Mouth Sores
Pain is a common symptom associated with autoimmune mouth sores. The intensity of pain can vary significantly depending on the size, location, and severity of the sores. Some people experience mild discomfort, while others have severe pain that can make eating, drinking, and speaking difficult. The pain may be accompanied by burning, tingling, or itching sensations. In cases of severe pain, over-the-counter pain relievers or prescription medications may be necessary.
Healing Time and Recurrence of Autoimmune Mouth Sores
The healing time for autoimmune mouth sores varies greatly, depending on the underlying condition and the severity of the sores. Some sores may heal within a few days, while others may persist for several weeks or even months. A concerning characteristic of these sores is their tendency to recur. This recurring nature is a key distinguishing feature from other types of mouth sores. Regular follow-up with a healthcare provider is essential to monitor healing and manage potential recurrences.
Distinguishing Autoimmune Mouth Sores from Other Mouth Sores
It is vital to distinguish autoimmune mouth sores from other, more common types of mouth sores. Canker sores are usually smaller, shallower, and heal faster. Cold sores (herpes simplex) are typically clustered blisters that appear on the lips or surrounding area and are caused by a virus. Oral thrush (candidiasis) appears as white patches. The duration, recurrence, location, and associated symptoms are crucial for differentiating autoimmune mouth sores from other types of mouth lesions. A healthcare professional can make the correct diagnosis.
| Characteristic | Autoimmune Mouth Sore | Other Mouth Sores (e.g., Canker Sore, Cold Sore) |
|---|---|---|
| Appearance | Variable; shallow or deep ulcers, various sizes, may cluster | Usually smaller, more defined; blisters for cold sores, white patches for thrush |
| Location | Tongue, gums, cheeks, lips, palate | Typically lips (cold sores), inner cheeks (canker sores) |
| Pain | Variable; can be severe | Mild to moderate; usually less intense than autoimmune sores |
| Recurrence | Frequent recurrence common | Less frequent recurrence; cold sores may recur |
| Healing Time | Variable; can be prolonged | Usually faster healing |
What do lupus mouth sores look like?

Lupus mouth sores, also known as oral ulcers or aphthous ulcers, can vary in appearance, but they often present as small, shallow lesions that are typically round or oval in shape. They can range in size from a few millimeters to a couple of centimeters. The sores usually have a yellowish-white or grayish-white center that is surrounded by a reddish border. They are often painful and may bleed easily if irritated. The appearance can differ depending on the severity and type of lupus, as well as individual responses to the disease. It is crucial to consult a doctor or dentist for proper diagnosis as other conditions can present with similar symptoms. The key is that lupus mouth sores are not unique in appearance and need professional examination to confirm diagnosis.
Types of Lupus Mouth Sores
The appearance of mouth sores associated with lupus isn't specific to lupus itself; instead, the sores are often aphthous ulcers that can arise in various conditions. These ulcers are not diagnostic of lupus alone. While the presence of these sores in conjunction with other lupus symptoms can be indicative, they are not a unique identifying characteristic. Therefore, a diagnosis requires a broader evaluation of clinical presentation.
- Minor aphthous ulcers: These are the most common, small (less than 1 cm), shallow, and heal within 1-2 weeks.
- Major aphthous ulcers: Larger (more than 1 cm), deeper ulcers that can take several weeks to heal and may leave scars.
- Herpetiform ulcers: These are small, numerous ulcers resembling cold sores, but they are not caused by the herpes virus.
Location of Lupus Mouth Sores
Lupus mouth sores can appear anywhere in the mouth, although they are more commonly located on the inner surface of the lips, cheeks, gums, or the soft palate (the soft tissue at the back of the roof of the mouth). They rarely appear on the tongue itself. The location isn't a definitive indicator of lupus, as these locations are common for other types of oral ulcers. However, the distribution pattern, when considered alongside other symptoms, might assist in the diagnostic process.
- Inner lips
- Cheeks
- Gums
- Soft palate
Symptoms Associated with Lupus Mouth Sores
While the appearance of the sores themselves can offer clues, additional symptoms accompanying them significantly increase suspicion of lupus. The mouth sores often coexist with other systemic lupus erythematosus (SLE) symptoms, which can help healthcare providers arrive at a diagnosis. The presence of mouth sores alone doesn't confirm lupus. These sores must be considered in conjunction with the overall clinical picture.
- Facial rash (malar rash): A butterfly-shaped rash across the cheeks and nose.
- Joint pain (arthralgia): Pain and stiffness in the joints.
- Fatigue: Extreme tiredness and exhaustion.
- Fever
Differentiating Lupus Mouth Sores from Other Conditions
Many conditions can cause mouth sores, making accurate differentiation crucial. Several oral health issues share similarities with lupus-related mouth sores, highlighting the importance of a thorough examination by a medical professional. Self-diagnosis should be avoided; a doctor or dentist can conduct tests and consider the patient's medical history to arrive at the correct diagnosis.
- Aphthous stomatitis (canker sores): Very common and often indistinguishable from lupus mouth sores.
- Herpes simplex virus (HSV): Cold sores, typically with a different distribution and accompanied by other symptoms.
- Oral thrush (candidiasis): Fungal infection often appearing as white patches.
What are autoimmune oral signs?
Autoimmune diseases can manifest in the oral cavity in various ways, often impacting the salivary glands, gums, and mucosa. These oral manifestations are not always specific to one particular autoimmune disease, and their presence does not definitively diagnose a specific condition. However, certain oral signs can be strongly suggestive of an underlying autoimmune process and warrant further investigation. These signs often reflect systemic inflammation and immune system dysfunction affecting the oral tissues. The severity and specific presentation of oral manifestations vary widely depending on the individual, the specific autoimmune disease involved, and the stage of the disease.
1. Xerostomia (Dry Mouth)
Xerostomia, or dry mouth, is a common oral sign associated with many autoimmune diseases, particularly Sjögren's syndrome. It results from reduced saliva production due to damage to the salivary glands by the body's own immune system. This decreased saliva flow impacts oral health significantly.
- Increased risk of dental caries (cavities): Saliva plays a crucial role in neutralizing acids and remineralizing tooth enamel. Reduced saliva flow makes teeth more vulnerable to decay.
- Burning sensation in the mouth: The lack of lubricating saliva can lead to discomfort and a burning feeling, making it difficult to eat and speak.
- Difficulty swallowing: Dryness can impede the smooth passage of food, leading to swallowing difficulties.
2. Sialadenitis (Inflammation of the Salivary Glands)
Sialadenitis, the inflammation of the salivary glands, is another frequent oral manifestation of autoimmune diseases. The inflammation can be acute or chronic and is characterized by swelling and pain in the salivary glands, typically the parotid glands located near the ears. The immune system's attack on these glands leads to impaired salivary function.
- Swelling of the cheeks or under the jaw: The swelling is often noticeable, particularly during exacerbations of the underlying disease.
- Pain during chewing or swallowing: The inflammation can make the act of eating uncomfortable.
- Reduced saliva production: This leads to many of the same problems as xerostomia, such as increased caries risk and oral discomfort.
3. Oral Ulcers and Mucosal Lesions
Many autoimmune diseases can cause oral ulcers and other mucosal lesions. These sores can vary in size, shape, and location, and they may be accompanied by pain and bleeding. The precise etiology of these lesions in autoimmune diseases is often complex and not fully understood but likely involves immune-mediated inflammation of the oral mucosa.
- Recurrent aphthous ulcers (canker sores): These small, painful sores are common in individuals with autoimmune diseases.
- Erythematous patches: Reddened areas of the mucosa can indicate inflammation and immune system activity.
- Unusual mucosal lesions: Some autoimmune diseases may result in unique or atypical oral lesions, which can be helpful in diagnosis.
4. Gingivitis and Periodontitis
Autoimmune diseases often increase the risk of gum disease (gingivitis and periodontitis). This heightened susceptibility is attributed to factors such as decreased salivary flow, impaired immune response, and increased susceptibility to infections. Poor oral hygiene, already a major factor in periodontal disease, is exacerbated in individuals with autoimmune conditions.
- Inflamed and bleeding gums: These are classic signs of gingivitis, the early stage of gum disease.
- Gum recession: The gums pull away from the teeth, exposing the roots and increasing the risk of tooth loss.
- Bone loss: Advanced periodontitis leads to the destruction of the bone supporting the teeth.
5. Geographic Tongue
Geographic tongue, characterized by smooth, red patches on the tongue that resemble a map, is sometimes associated with autoimmune diseases. While not diagnostic of an autoimmune condition, its presence can warrant further investigation, especially if accompanied by other oral or systemic symptoms. The exact cause of geographic tongue is unknown, but it is thought to be related to inflammation and immune responses in the tongue.
- Patches that change shape and location: The characteristic feature of geographic tongue is the constantly shifting pattern of red and white areas on the tongue's surface.
- Usually asymptomatic: While the appearance can be striking, geographic tongue usually causes no pain or discomfort.
- Potential link to other autoimmune conditions: A higher prevalence of geographic tongue has been observed in individuals with certain autoimmune diseases, though a direct causal relationship isn't definitively established.
What autoimmune disease causes mouth sores?

Several autoimmune diseases can cause mouth sores, but the most common association is with Behçet's disease. This condition causes inflammation throughout the body, and oral ulcers are a hallmark symptom. However, other autoimmune diseases can also manifest with mouth sores, albeit less frequently or as a less prominent symptom. The specific cause of mouth sores within the context of autoimmune diseases is complex and not fully understood, but it's believed to involve an overactive immune system attacking healthy tissues in the mouth, leading to ulceration.
Behçet's Disease and Oral Ulcers
Behçet's disease is a rare, chronic inflammatory disorder that primarily affects blood vessels. Recurrent painful mouth sores are a characteristic feature, often appearing as aphthous ulcers. These ulcers can be small or large, and may persist for days or weeks before healing. The exact mechanism linking Behçet's to oral ulcers is not fully clear, but it involves immune system dysregulation and inflammation of the mouth's mucous membranes. The severity of oral ulcers in Behçet's disease varies significantly between individuals.
- Frequent and recurrent oral ulcers are a defining characteristic.
- Ulcers can range from small and superficial to large and deep, causing significant discomfort.
- Treatment focuses on managing pain and inflammation, often involving corticosteroids or immunosuppressants.
Lupus and Oral Manifestations
Systemic lupus erythematosus (SLE), or simply lupus, is a chronic autoimmune disease that can affect many parts of the body. While oral ulcers aren't always a prominent feature of lupus, they can occur. They may appear as aphthous ulcers similar to those seen in Behçet's disease, but often in conjunction with other lupus symptoms like facial rash, joint pain, and fatigue. The immune system's attack on various tissues in lupus can incidentally involve the oral mucosa.
- Oral ulcers in lupus are often less frequent and severe compared to Behçet's.
- They may be accompanied by other characteristic lupus symptoms.
- Treatment of lupus-related oral ulcers usually involves managing the underlying lupus condition.
Pernicious Anemia and Mouth Sores
Pernicious anemia is an autoimmune disease affecting vitamin B12 absorption. While not directly causing mouth sores in the same way as Behçet's or lupus, it can lead to glossitis, an inflammation of the tongue. This can manifest as a smooth, red, and painful tongue, often with accompanying mouth sores. The underlying cause is vitamin B12 deficiency, impacting the health of the oral mucosa.
- Glossitis is a common oral manifestation of pernicious anemia.
- This manifests as a sore, red, and often shiny tongue.
- Treatment involves B12 supplementation to correct the deficiency and resolve the oral symptoms.
Inflammatory Bowel Disease (IBD) and Oral Ulcers
Inflammatory bowel diseases, such as Crohn's disease and ulcerative colitis, are chronic inflammatory conditions affecting the digestive tract. While primarily affecting the gut, IBD can sometimes have extra-intestinal manifestations, including oral ulcers. These ulcers are often similar in appearance to aphthous ulcers but are part of a broader systemic inflammatory response. The connection is not fully understood, but it likely involves immune system dysregulation.
- Oral ulcers in IBD are often associated with active intestinal inflammation.
- They are typically treated with medications aimed at managing the underlying IBD.
- The severity and frequency of oral ulcers vary greatly among individuals with IBD.
Sjögren's Syndrome and Oral Dryness Leading to Sores
Sjögren's syndrome is an autoimmune disease that primarily affects the tear and salivary glands, leading to dry eyes and dry mouth (xerostomia). This chronic dryness can create an environment in the mouth that is more susceptible to infections and ulcerations. While not directly causing mouth sores, the lack of saliva can exacerbate existing sores or make the mouth more prone to developing them. The underlying autoimmune response damages the salivary glands, reducing saliva production.
- Xerostomia, or dry mouth, is a prominent feature of Sjögren's syndrome.
- Dryness increases susceptibility to oral infections and ulcerations.
- Treatment focuses on managing dry mouth symptoms, often with artificial saliva substitutes.
What do Behcet's sores look like?

Behçet's disease is a rare, chronic inflammatory disorder that can affect many parts of the body. One of its hallmark symptoms is the development of recurrent, painful sores. These sores, or aphthous ulcers, can appear in the mouth, genitals, and on the skin. Their appearance can vary, but some common characteristics include being round or oval-shaped, shallow, and having a yellowish-gray base surrounded by a red halo. They are typically small to medium in size, although they can sometimes coalesce to form larger lesions. The sores are often tender and can be quite painful, particularly when eating or engaging in sexual activity, depending on their location. The appearance can vary in severity and size between outbreaks, and their healing time can be several days or even weeks. The severity of the sores is not always indicative of the overall disease severity. It's important to note that the sores are not contagious.
Location of Behçet's Sores
Behçet's sores can appear in various locations throughout the body. The most common areas affected include the mouth, genitals, and skin. Oral ulcers are a hallmark of the disease and are often the first symptoms to appear. Genital ulcers can be incredibly painful and are often found on the penis, scrotum, or vulva. Skin lesions can occur anywhere on the body and may take on different forms. The frequency and severity of the sores can vary widely among individuals.
- Oral ulcers: These are typically found on the inside of the cheeks, lips, gums, and tongue.
- Genital ulcers: These can appear on the penis, scrotum, vulva, or labia.
- Skin lesions: These can manifest as papulopustular lesions, erythema nodosum, or other types of skin inflammation.
Appearance of Oral Behçet's Sores
Oral ulcers in Behçet's disease are characteristically painful and recurrent. They tend to be shallow, round or oval, and often have a yellowish-gray base with an erythematous (red) border. The size can vary, from small pinpoint ulcers to larger lesions that can be several centimeters in diameter. Multiple ulcers may appear simultaneously, and they can be extremely uncomfortable, making eating and drinking difficult. The healing process can take several days to weeks.
- Shallow depth
- Yellowish-gray base
- Red, inflamed border
Appearance of Genital Behçet's Sores
Genital ulcers are another common manifestation of Behçet's disease. Similar to oral ulcers, they are usually painful and recurrent. These ulcers can be quite large and deep, and they often bleed easily. They can be found on the penis, scrotum, vulva, or labia. The appearance may vary slightly depending on location and depth, but the underlying inflammatory process is consistent. The intense pain can impact daily life and sexual activity.
- Painful and deep ulcers
- Often bleed easily
- Can be large in size
Appearance of Skin Behçet's Lesions
Behçet's disease can also present with various skin lesions. While aphthous ulcers are characteristic, other skin manifestations can occur. These can include erythema nodosum (red, tender bumps usually on the shins), papulopustular lesions (small bumps or pustules), acneiform lesions, and others. The appearance and location of these skin lesions vary significantly. Some may be more easily treated than others.
- Erythema nodosum
- Papulopustular lesions
- Acneiform lesions
What are the common symptoms of autoimmune mouth sores?
Autoimmune mouth sores, often associated with conditions like Behçet's disease or lupus, can manifest in various ways. A key feature is the recurrence of sores. Unlike canker sores that might appear once in a while, autoimmune mouth sores tend to recur frequently, sometimes with overlapping lesions. The sores themselves can vary significantly in appearance. Some individuals might experience small, shallow ulcers that are painful and easily irritated. Others may develop larger, deeper lesions that may bleed or be covered with a yellowish-white coating. The location of sores can also be indicative; while canker sores are typically found on the inner cheeks, tongue, or lips, autoimmune sores can appear anywhere in the mouth, including the gums, palate, and even the throat. Pain is a common symptom, ranging from mild discomfort to severe pain that interferes with eating and speaking. Swelling and redness surrounding the sores are also frequent occurrences. The severity and frequency of outbreaks can vary greatly, depending on the underlying autoimmune condition and its management. It's crucial to consult a doctor or dentist for proper diagnosis and treatment as these sores can be a symptom of more serious underlying medical problems. Self-treating can be dangerous and delay proper treatment of the underlying autoimmune condition.
How do autoimmune mouth sores differ from canker sores?
While both autoimmune mouth sores and canker sores present as painful oral ulcers, there are significant differences. Canker sores, also known as aphthous ulcers, are typically small, shallow, and oval-shaped. They usually heal within 7-10 days without scarring. They're often found on the non-keratinized mucous membranes of the mouth, most commonly on the inner cheeks, lips, or tongue. In contrast, autoimmune mouth sores can be more varied in size, shape, and location. They often recur frequently, sometimes with overlapping lesions, indicating a chronic rather than sporadic condition. Autoimmune sores may also be deeper and take longer to heal, potentially leaving behind scars. Their location can extend beyond the typical sites of canker sores, affecting the gums, palate, or even the throat. Another crucial difference lies in the underlying cause. Canker sores are often linked to stress, injury, or dietary deficiencies, while autoimmune mouth sores are a symptom of an underlying autoimmune disease. Therefore, a proper diagnosis by a medical professional is needed to determine the cause and guide appropriate treatment, distinguishing between simple canker sores and the more concerning symptoms of an autoimmune condition.
Are there any specific tests to diagnose autoimmune mouth sores?
There isn't a single definitive test to diagnose autoimmune mouth sores directly. The diagnosis relies heavily on a combination of factors, including a thorough medical history, a physical examination of the mouth and other body parts, and assessing the pattern of oral ulcer recurrence. The doctor will inquire about the frequency, duration, and location of the sores. They will look for other symptoms that might suggest an autoimmune disorder, such as skin rashes, joint pain, eye inflammation, or fatigue. Based on the initial assessment, various blood tests may be ordered to check for markers associated with specific autoimmune diseases. These could include tests for antinuclear antibodies (ANA) for lupus, or other disease-specific antibodies. Biopsy of the oral lesion may be considered in some cases to rule out other conditions or confirm the presence of certain inflammatory patterns. The diagnostic process is often iterative, involving the evaluation of symptoms over time and the results of various tests to build a comprehensive picture and arrive at a precise diagnosis of the underlying autoimmune disease responsible for the mouth sores.
What treatment options are available for autoimmune mouth sores?
Treatment for autoimmune mouth sores focuses on managing the underlying autoimmune condition and relieving the symptoms. There's no single cure, and the approach is tailored to the specific disease and the individual's response. Medication plays a crucial role. Corticosteroids, either topical (applied directly to the sores) or systemic (taken orally or intravenously), are often used to reduce inflammation and pain. Immunosuppressant drugs may be prescribed in more severe cases to suppress the overactive immune system. Topical anesthetics can provide temporary pain relief. Antiviral medications might be used if a viral infection is contributing to the sores. In addition to medication, lifestyle modifications can be beneficial. Maintaining good oral hygiene, including regular brushing and flossing, is important to prevent infection. Avoiding known triggers, such as spicy or acidic foods, can help reduce irritation. Managing stress through techniques like yoga or meditation can also have a positive impact. Regular follow-up appointments with a doctor or specialist are essential to monitor the condition, adjust treatment as needed, and manage any complications. The goal is to achieve long-term remission of the underlying autoimmune disease, thereby minimizing the occurrence and severity of mouth sores.
Deja una respuesta