What health issues cause mouth sores

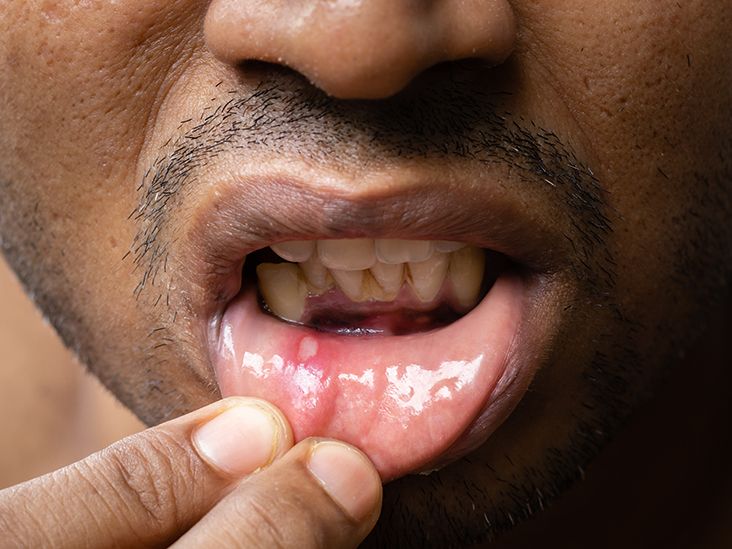
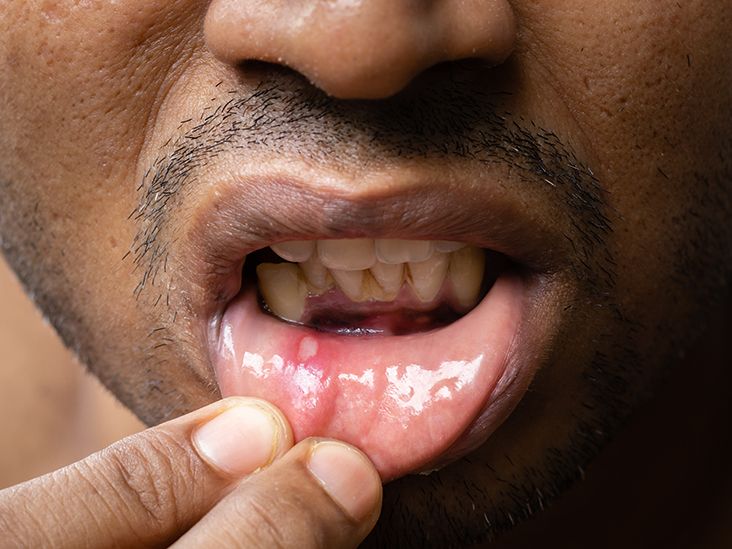
Mouth sores, also known as canker sores or aphthous ulcers, are small, painful lesions that can develop on the inside of your mouth or on your tongue. While they are not usually serious, mouth sores can be uncomfortable and make it difficult to eat, drink, or talk.
There are a number of different health issues that can cause mouth sores. Some of the most common include:
What Health Issues Cause Mouth Sores?
Viral Infections
Many viral infections can lead to mouth sores. Herpes simplex virus (HSV), commonly known as the cause of cold sores or fever blisters, is a primary culprit. These sores typically appear on the lips and around the mouth, but can sometimes occur inside the mouth. Another common viral infection is the human papillomavirus (HPV), which can cause warts in the mouth. These can appear as small, cauliflower-like growths. Hand, foot, and mouth disease, caused by coxsackieviruses, is a common childhood illness that often presents with painful sores inside the mouth.
Bacterial Infections
While less common than viral infections, bacterial infections can also cause mouth sores. Streptococcal infections can sometimes lead to the development of mouth sores, especially in individuals with weakened immune systems. Poor oral hygiene can also contribute to bacterial overgrowth, leading to the formation of sores and other oral health issues. Proper brushing, flossing, and regular dental checkups are crucial in preventing bacterial infections.
Fungal Infections
Oral thrush, a fungal infection caused by Candida albicans, is a frequent cause of mouth sores, especially in infants, older adults, and individuals with compromised immune systems. These sores appear as creamy white patches on the tongue, inner cheeks, and roof of the mouth. They can be painful and interfere with eating and swallowing. Treatment typically involves antifungal medications.
Nutritional Deficiencies
Certain nutritional deficiencies can manifest as mouth sores. Iron deficiency, vitamin B12 deficiency, and folic acid deficiency are commonly linked to the development of mouth sores. These deficiencies can impair the body's ability to repair damaged tissues, making it more susceptible to sores and other oral health problems. A balanced diet rich in essential vitamins and minerals is crucial for maintaining oral health.
Autoimmune Diseases
Autoimmune diseases, such as Behçet's disease and lupus, can cause mouth sores as a symptom. These diseases cause the body's immune system to attack its own tissues, leading to inflammation and the formation of sores in the mouth and other areas of the body. Management of these diseases often involves medication to suppress the immune system and alleviate symptoms.
| Cause | Type of Sore | Symptoms |
|---|---|---|
| Herpes Simplex Virus (HSV) | Cold sores, fever blisters | Blisters, pain, tingling |
| Human Papillomavirus (HPV) | Oral warts | Small, cauliflower-like growths |
| Candida albicans (Oral Thrush) | Creamy white patches | Pain, difficulty eating |
| Iron Deficiency | Angular cheilitis (corner of mouth) | Cracked, sore corners of mouth |
| Behçet's Disease | Recurrent aphthous ulcers | Painful sores, inflammation |
https://youtube.com/watch?v=mouth-sores
What Health Issues Cause Mouth Sores?
Viral Infections
Many viral infections can lead to mouth sores. Herpes simplex virus (HSV), commonly known as the cause of cold sores or fever blisters, is a primary culprit. These sores typically appear on the lips and around the mouth, but can sometimes occur inside the mouth. Another common viral infection is the human papillomavirus (HPV), which can cause warts in the mouth. These can appear as small, cauliflower-like growths. Hand, foot, and mouth disease, caused by coxsackieviruses, is a common childhood illness that often presents with painful sores inside the mouth.
Bacterial Infections
While less common than viral infections, bacterial infections can also cause mouth sores. Streptococcal infections can sometimes lead to the development of mouth sores, especially in individuals with weakened immune systems. Poor oral hygiene can also contribute to bacterial overgrowth, leading to the formation of sores and other oral health issues. Proper brushing, flossing, and regular dental checkups are crucial in preventing bacterial infections.
Fungal Infections
Oral thrush, a fungal infection caused by Candida albicans, is a frequent cause of mouth sores, especially in infants, older adults, and individuals with compromised immune systems. These sores appear as creamy white patches on the tongue, inner cheeks, and roof of the mouth. They can be painful and interfere with eating and swallowing. Treatment typically involves antifungal medications.
Nutritional Deficiencies
Certain nutritional deficiencies can manifest as mouth sores. Iron deficiency, vitamin B12 deficiency, and folic acid deficiency are commonly linked to the development of mouth sores. These deficiencies can impair the body's ability to repair damaged tissues, making it more susceptible to sores and other oral health problems. A balanced diet rich in essential vitamins and minerals is crucial for maintaining oral health.
Autoimmune Diseases
Autoimmune diseases, such as Behçet's disease and lupus, can cause mouth sores as a symptom. These diseases cause the body's immune system to attack its own tissues, leading to inflammation and the formation of sores in the mouth and other areas of the body. Management of these diseases often involves medication to suppress the immune system and alleviate symptoms.
| Cause | Type of Sore | Symptoms |
|---|---|---|
| Herpes Simplex Virus (HSV) | Cold sores, fever blisters | Blisters, pain, tingling |
| Human Papillomavirus (HPV) | Oral warts | Small, cauliflower-like growths |
| Candida albicans (Oral Thrush) | Creamy white patches | Pain, difficulty eating |
| Iron Deficiency | Angular cheilitis (corner of mouth) | Cracked, sore corners of mouth |
| Behçet's Disease | Recurrent aphthous ulcers | Painful sores, inflammation |
What diseases are associated with mouth sores?
Primary Herpetic Gingivostomatitis (HSV-1)
Primary herpetic gingivostomatitis is a common infection caused by the herpes simplex virus type 1 (HSV-1). It typically presents with painful, widespread mouth sores, often accompanied by fever, swollen gums, and general malaise. The sores are usually small vesicles (blisters) that break open and leave painful ulcers. This is a highly contagious viral infection, and treatment focuses on managing symptoms until the infection resolves spontaneously.
- Highly contagious through saliva exchange.
- Symptoms include fever, swollen gums, and multiple small blisters.
- Treatment focuses on symptom management, like pain relief and antiviral medications.
Aphthous Ulcers (Canker Sores)
Aphthous ulcers, commonly known as canker sores, are small, shallow ulcers that appear on the soft tissues of the mouth. While their exact cause is unknown, stress, trauma, hormonal changes, and nutritional deficiencies are thought to be contributing factors. They typically heal within 1-3 weeks without scarring. Although not infectious, recurrent canker sores can be quite debilitating due to pain and discomfort.
- Not contagious.
- Triggered by stress, trauma, hormonal fluctuations, and nutritional deficiencies.
- Usually heal on their own within a few weeks; treatment focuses on pain relief.
Hand, Foot, and Mouth Disease (HFMD)
Hand, foot, and mouth disease, typically caused by Coxsackievirus A16, is a common viral infection mainly affecting young children. It is characterized by small, painful sores in the mouth, accompanied by a rash on the hands and feet. The sores are often accompanied by fever, fatigue, and loss of appetite. The virus spreads easily through contact with respiratory secretions or feces of an infected individual.
- Highly contagious, often affecting young children.
- Characterized by sores in the mouth, and a rash on hands and feet.
- Treatment focuses on symptom relief, as it typically resolves on its own.
Behçet's Disease
Behçet's disease is a rare, chronic inflammatory disorder that can affect many parts of the body, including the mouth. Mouth sores are a hallmark symptom, often appearing as painful, recurrent ulcers. Other symptoms can include genital ulcers, skin lesions, and eye inflammation. The cause is unknown, and treatment focuses on managing symptoms and preventing complications.
- A rare, chronic inflammatory disease.
- Recurrent mouth ulcers are a defining symptom.
- Treatment involves managing symptoms and preventing complications.
Oral Cancer
While not all mouth sores are cancerous, persistent or unusual sores that don't heal within a few weeks should be evaluated by a doctor. Oral cancer can manifest as painless ulcers, lumps, or white or red patches in the mouth. Risk factors include tobacco use, excessive alcohol consumption, and exposure to the human papillomavirus (HPV). Early detection and treatment are crucial for improving prognosis.
- Persistent sores that don't heal should be examined by a doctor.
- May present as painless ulcers, lumps, or discolored patches.
- Early diagnosis and treatment are critical.
When should I be concerned about mouth sores?
When Should I Be Concerned About Mouth Sores?
Mouth sores, also known as aphthous ulcers or canker sores, are common and usually heal on their own within a week or two. However, some mouth sores require medical attention. You should be concerned and seek professional medical advice if your mouth sores exhibit certain characteristics or persist beyond a reasonable timeframe. The severity, duration, and accompanying symptoms are crucial factors in determining whether a visit to the doctor or dentist is necessary.
1. Persistent Sores That Don't Heal
A common indicator that something might be amiss is the persistence of mouth sores. Most mouth sores heal within 10-14 days. If your sore(s) last longer than this, or show no signs of healing after a couple of weeks, it’s essential to seek evaluation. This could indicate a more serious underlying condition. This prolonged healing time should not be ignored.
- Consider seeing a doctor if sores persist for more than three weeks.
- Note the size and location of the sore(s) to help describe to the healthcare professional.
- Keep a record of any changes in the sores' appearance or symptoms over time.
2. Large or Unusually Painful Sores
While minor mouth sores are generally manageable with over-the-counter remedies, unusually large or excruciatingly painful sores warrant concern. The size and pain level are subjective, but if the discomfort significantly interferes with eating, drinking, or speaking, medical attention is advised. This could point towards an infection or other underlying condition needing treatment.
- Pain that is unbearable, even with pain relievers.
- Sores that are significantly larger than typical canker sores.
- Sores that are accompanied by severe swelling in the mouth or surrounding tissues.
3. Sores Accompanied by Other Symptoms
Mouth sores rarely exist in isolation. If your sores are accompanied by other symptoms, it’s crucial to seek medical advice. These accompanying symptoms might provide clues to the underlying cause. Fever, fatigue, swollen lymph nodes, or unexplained weight loss are all significant red flags that could indicate a systemic issue.
- Fever or chills suggest a possible infection.
- Swollen lymph nodes might indicate a more serious infection.
- Unexplained weight loss or fatigue could be a sign of an underlying health problem.
4. Recurring Sores With Increased Frequency or Severity
If you experience frequent outbreaks of mouth sores that become increasingly severe or persistent, it’s important to consult a healthcare professional. This pattern suggests a possible underlying medical condition or immune deficiency that needs to be addressed. Changes in the frequency and severity of sores should not be dismissed. A physician can help determine the root cause.
- Keep a record of outbreaks, noting their frequency, duration, and severity.
- Consider if there are any triggers associated with the increased frequency or severity.
- Discuss your concerns with a doctor to explore potential underlying causes and management options.
5. Sores That Bleed Easily or Don't Respond to Treatment
Mouth sores that bleed easily or fail to respond to home treatment (like rinsing with salt water or applying topical medications) require a doctor's assessment. Easy bleeding suggests a potential issue with blood clotting or an underlying condition. Resistance to home treatment indicates the need for a more specific and targeted approach.
- Excessive bleeding from the sores, even with minor trauma.
- Lack of improvement despite using over-the-counter treatments for several days.
- Unusual appearance of the sores, such as a different color, texture, or shape compared to usual canker sores.
Which deficiency disease causes sores in the mouth?

Several deficiency diseases can cause sores in the mouth, but the most commonly associated is riboflavin deficiency, also known as ariboflavinosis. This vitamin B2 deficiency leads to inflammation of the mucous membranes in the mouth, resulting in painful cracks and sores, often at the corners of the mouth (angular cheilitis). Other deficiencies, though less directly linked to mouth sores, can contribute to or exacerbate oral lesions.
Riboflavin Deficiency (Ariboflavinosis)
Ariboflavinosis, resulting from insufficient intake of riboflavin (vitamin B2), is a primary cause of mouth sores. Riboflavin plays a crucial role in maintaining healthy skin and mucous membranes. A deficiency leads to inflammation and cracking, particularly at the corners of the mouth (angular cheilitis). Symptoms often include a burning sensation in the mouth and a bright red, sore tongue (glossitis).
- Angular cheilitis: Cracks and sores at the corners of the mouth.
- Glossitis: Inflammation and soreness of the tongue.
- Cheilosis: General inflammation and cracking of the lips.
Iron Deficiency Anemia
Iron deficiency anemia, while not directly causing sores in the same way as riboflavin deficiency, can significantly weaken the immune system and make the mouth more susceptible to infections and sores. The reduced immune response means the body is less able to fight off infections that may cause oral lesions. Iron is essential for healthy mucous membranes.
- Weakened immune system: Increased vulnerability to infections.
- Pale mucous membranes: A visible sign of iron deficiency.
- Delayed wound healing: Sores may take longer to heal.
Niacin Deficiency (Pellagra)
Severe niacin (vitamin B3) deficiency leads to pellagra, characterized by the "three Ds": diarrhea, dermatitis, and dementia. Oral manifestations include a bright red, swollen, and sore tongue (glossitis) and sores in the mouth. The inflammation can be extensive and debilitating.
- Glossitis: Inflammation and soreness of the tongue.
- Oral mucosal lesions: Sores and inflammation throughout the mouth.
- Dermatitis: Skin rashes, often affecting sun-exposed areas.
Vitamin B12 Deficiency
Vitamin B12 deficiency can cause pernicious anemia, which can manifest with oral symptoms. While not a primary cause of mouth sores in the same manner as riboflavin deficiency, it can contribute to a general decline in oral health and increased susceptibility to infections, potentially leading to the development of sores.
- Glossitis: Smooth, sore, and possibly pale tongue.
- Increased risk of infection: Weakened immune response.
- Pernicious anemia: A type of anemia linked to B12 deficiency.
Folic Acid Deficiency
Similar to vitamin B12 deficiency, folic acid deficiency can contribute to anemia and a weakened immune system, making the mouth more prone to infections and sores. While not a direct cause of sores in the same way as riboflavin deficiency, it can indirectly contribute to oral lesions.
- Anemia: Leads to general weakness and reduced immune function.
- Impaired cell growth: Affects the repair and regeneration of tissues.
- Increased susceptibility to infection: Making the mouth more prone to sores.
What autoimmune conditions have mouth sores?

Several autoimmune conditions can manifest with mouth sores as a symptom. The presence of mouth sores alone isn't diagnostic, and further investigation is always necessary to determine the underlying cause. However, some conditions are more strongly associated with oral ulcerations than others.
Behçet's Disease and Mouth Sores
Behçet's disease is a rare, chronic inflammatory disorder that can affect blood vessels throughout the body. Mouth sores are a hallmark symptom of Behçet's disease, often appearing as recurrent, painful aphthous ulcers. These ulcers can be quite severe and may persist for extended periods. The condition can also affect the eyes, skin, and genitals, leading to a range of symptoms beyond oral manifestations.
- Recurrent oral ulcers: These are painful and can be quite large.
- Genital ulcers: Similar in appearance to the oral ulcers.
- Eye inflammation (uveitis): Can lead to vision problems.
Systemic Lupus Erythematosus (SLE) and Mouth Sores
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease that can affect many parts of the body. While not a primary symptom, oral ulcers can occur in patients with SLE, often alongside other mucocutaneous manifestations like rashes and skin lesions. The ulcers can vary in severity and frequency. It’s important to note that the presence of mouth sores alone is not diagnostic of SLE.
- Facial rash (butterfly rash): A characteristic symptom across the cheeks and nose.
- Joint pain (arthritis): Affecting multiple joints.
- Fatigue and fever: Common systemic symptoms.
Pemphigus Vulgaris and Mouth Sores
Pemphigus vulgaris is a rare, severe autoimmune blistering disorder affecting the skin and mucous membranes. Oral lesions are often the first sign of pemphigus vulgaris, presenting as painful, fragile blisters that easily rupture, leaving raw, eroded areas. These lesions can be extremely painful and interfere with eating and speaking. This condition requires urgent medical attention.
- Oral blisters and erosions: These are fragile and easily break.
- Skin blisters: Similar to oral lesions, affecting various body areas.
- Severe pain and discomfort: Significantly impacting daily life.
Crohn's Disease and Mouth Sores
Crohn's disease is a type of inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal tract. Oral manifestations in Crohn's disease are not uncommon, though not consistently present in every patient. These can include aphthous ulcers, angular cheilitis (cracking at the corners of the mouth), and other oral lesions. The oral symptoms are often associated with active intestinal inflammation.
- Abdominal pain and cramping: Often accompanied by diarrhea and weight loss.
- Rectal bleeding: A common symptom of the inflammation.
- Oral ulcers and angular cheilitis: Typically resolve with treatment of the underlying IBD.
Sjögren's Syndrome and Mouth Sores
Sjögren's syndrome is an autoimmune disorder primarily targeting the moisture-producing glands of the body. Dry mouth (xerostomia) is a hallmark symptom, which can predispose individuals to oral ulcerations and infections due to reduced saliva production. While not always directly causing ulcers, the dryness makes the mouth more vulnerable. Other symptoms relate to dry eyes and other mucosal surfaces.
- Dry mouth (xerostomia): Leading to discomfort, difficulty swallowing, and increased risk of infections.
- Dry eyes (keratoconjunctivitis sicca): Causing burning, itching, and blurred vision.
- Fatigue and joint pain: Common systemic symptoms.
What are the most common causes of mouth sores?
Mouth sores, also known as aphthous ulcers or canker sores, are a common ailment affecting many individuals. While the exact cause remains unknown, several factors are strongly implicated. Stress is a significant contributor, with studies showing a correlation between high stress levels and increased frequency and severity of mouth sores. Minor trauma to the mouth, such as biting your cheek or accidentally scratching the inside of your mouth with a toothbrush, can also trigger their development. Certain foods, particularly acidic or spicy foods, can irritate the mouth lining and lead to sore formation. Hormonal changes, particularly in women, are also associated with mouth sores, often flaring up during menstruation. Nutritional deficiencies, especially in iron, vitamin B12, and folic acid, can sometimes play a role. Finally, certain medical conditions such as inflammatory bowel disease (IBD), celiac disease, and Behçet's disease can be associated with recurrent and severe mouth sores. It's important to note that often, the exact trigger remains elusive, and sores may appear spontaneously without any discernible cause. If you are experiencing persistent or severe mouth sores, it is recommended to consult a dentist or doctor to rule out any underlying medical issues.
Can mouth sores be a symptom of a more serious condition?
While most mouth sores are benign and resolve on their own within a week or two, they can sometimes be a symptom of a more serious underlying medical condition. Conditions like Behçet's disease, a rare inflammatory disorder affecting blood vessels, often manifests with recurrent and painful mouth ulcers. Inflammatory bowel disease (IBD), encompassing Crohn's disease and ulcerative colitis, can also be associated with mouth sores as part of its systemic inflammation. Celiac disease, an autoimmune disorder triggered by gluten consumption, may present with mouth sores alongside other gastrointestinal symptoms. HIV/AIDS can also cause oral ulcers, often as one of the early symptoms. Leukemia and other blood cancers can sometimes manifest with oral lesions. Autoimmune diseases in general can sometimes be associated with mouth ulcers. Therefore, if you experience frequent, severe, or unusual mouth sores, particularly those that don't heal within a reasonable timeframe, it is crucial to seek medical attention for a proper diagnosis and to rule out any underlying health issues. A thorough medical history, physical examination, and potentially further investigations may be necessary.
How can I treat mouth sores at home?
For most common mouth sores, several home remedies can provide relief and promote healing. Rinsing your mouth with warm salt water several times a day can help to clean the area and reduce inflammation. Applying a topical anesthetic, such as an over-the-counter oral pain relief gel, can numb the sore and alleviate pain. Avoiding acidic, spicy, and hard-to-chew foods can prevent further irritation. Maintaining good oral hygiene, including brushing and flossing gently, is crucial to prevent infection. Using a soft-bristled toothbrush will minimize further trauma to the affected area. Some individuals find relief from applying a mixture of baking soda and water to the sores. However, it is important to note that these are only temporary solutions, and more persistent or severe sores might require professional medical attention. If home remedies are not effective or the sores persist for longer than two weeks, consulting a dentist or doctor is highly recommended.
When should I see a doctor about my mouth sores?
While many mouth sores heal on their own, there are certain circumstances where seeking medical attention is crucial. You should consult a doctor or dentist if your mouth sores are extremely painful and interfere with eating, drinking, or sleeping. If the sores are unusually large or do not heal within two weeks, professional evaluation is necessary. Recurrent mouth sores that appear frequently or persist for extended periods also warrant medical attention. If the sores are accompanied by other symptoms, such as fever, fatigue, swollen lymph nodes, or unexplained weight loss, you should seek immediate medical advice, as this could indicate a more serious underlying condition. Mouth sores that bleed excessively or show signs of infection (e.g., increased redness, swelling, pus) require prompt medical attention. Finally, if you have concerns about the appearance or nature of your mouth sores, don't hesitate to consult a healthcare professional for peace of mind and proper diagnosis. Early detection and treatment can be crucial in managing underlying medical conditions that might be contributing to the problem.
Deja una respuesta