What is COVID mouth sores

COVID-19 is not only a respiratory illness. It can also affect the mouth, causing a range of symptoms, including mouth sores. These sores can be painful and uncomfortable, and they can make it difficult to eat, drink, and speak. In this article, we will discuss what COVID mouth sores are, what causes them, and how to treat them.
What are COVID-19 Mouth Sores?
COVID-19, caused by the SARS-CoV-2 virus, can manifest in a variety of ways, and oral manifestations are increasingly recognized. While not a classic symptom, mouth sores, or oral lesions, can occur in some individuals infected with COVID-19. These sores aren't unique to COVID-19; many viral and bacterial infections can cause similar symptoms. However, their presence alongside other COVID-19 symptoms might suggest a connection. It's crucial to understand that mouth sores alone aren't diagnostic for COVID-19; further testing is needed for confirmation.
Types of Mouth Sores Associated with COVID-19
Several types of oral lesions can be associated with COVID-19. These include aphthous ulcers (canker sores), herpes simplex virus (HSV) reactivations, and less commonly, gingivitis (gum inflammation) and oral thrush (candidiasis). The exact mechanism by which COVID-19 triggers these oral manifestations isn't fully understood, but it might be related to the virus's impact on the immune system or direct viral involvement in the oral mucosa. The appearance of these sores can vary greatly depending on the underlying cause.
Frequency and Prevalence of COVID-19 Mouth Sores
The exact prevalence of mouth sores in COVID-19 patients is difficult to pinpoint due to variations in reporting and diagnostic methods. Studies suggest that while not a common primary symptom, oral manifestations can occur in a significant minority of infected individuals. This suggests that while not everyone with COVID-19 will experience mouth sores, it's certainly a possibility, and their presence shouldn't be entirely disregarded.
Distinguishing COVID-19 Mouth Sores from Other Oral Conditions
Differentiating COVID-19-related mouth sores from other oral conditions requires a comprehensive assessment. The presence of other COVID-19 symptoms, such as fever, cough, or loss of taste and smell, can be indicative. However, many other conditions, including stress, nutritional deficiencies, or other viral infections, can also cause mouth sores. A thorough medical history and physical examination by a healthcare professional are necessary for accurate diagnosis.
Treatment and Management of COVID-19 Mouth Sores
Treatment for COVID-19 mouth sores focuses primarily on managing the symptoms. Pain relief can be achieved with over-the-counter medications like topical anesthetics or analgesics. For specific conditions like oral thrush or herpes simplex, antifungal or antiviral medications may be prescribed. Maintaining good oral hygiene, including regular brushing and rinsing, can help prevent secondary infections and promote healing. If the sores are severe or persistent, consulting a dentist or doctor is advised. Remember, treating the underlying COVID-19 infection itself is crucial for overall recovery.
When to Seek Medical Attention for COVID-19 Mouth Sores
While many mouth sores resolve on their own, it's essential to seek medical attention if you experience:
- Severe pain
- Persistent sores that don't heal within a few weeks
- Signs of infection, such as increased swelling, redness, or pus
- Difficulty swallowing or eating
- Other concerning COVID-19 symptoms
| Symptom | Possible Cause | Treatment |
|---|---|---|
| Aphthous Ulcers (Canker Sores) | COVID-19, stress, nutritional deficiencies | Topical anesthetics, pain relievers |
| Herpes Simplex Virus Reactivation | COVID-19 (weakened immune system), stress | Antiviral medication |
| Oral Thrush (Candidiasis) | COVID-19 (weakened immune system), antibiotic use | Antifungal medication |
What are COVID-19 Mouth Sores?
COVID-19, caused by the SARS-CoV-2 virus, can manifest in a variety of ways, and oral manifestations are increasingly recognized. While not a classic symptom, mouth sores, or oral lesions, can occur in some individuals infected with COVID-19. These sores aren't unique to COVID-19; many viral and bacterial infections can cause similar symptoms. However, their presence alongside other COVID-19 symptoms might suggest a connection. It's crucial to understand that mouth sores alone aren't diagnostic for COVID-19; further testing is needed for confirmation.
Types of Mouth Sores Associated with COVID-19
Several types of oral lesions can be associated with COVID-19. These include aphthous ulcers (canker sores), herpes simplex virus (HSV) reactivations, and less commonly, gingivitis (gum inflammation) and oral thrush (candidiasis). The exact mechanism by which COVID-19 triggers these oral manifestations isn't fully understood, but it might be related to the virus's impact on the immune system or direct viral involvement in the oral mucosa. The appearance of these sores can vary greatly depending on the underlying cause.
Frequency and Prevalence of COVID-19 Mouth Sores
The exact prevalence of mouth sores in COVID-19 patients is difficult to pinpoint due to variations in reporting and diagnostic methods. Studies suggest that while not a common primary symptom, oral manifestations can occur in a significant minority of infected individuals. This suggests that while not everyone with COVID-19 will experience mouth sores, it's certainly a possibility, and their presence shouldn't be entirely disregarded.
Distinguishing COVID-19 Mouth Sores from Other Oral Conditions
Differentiating COVID-19-related mouth sores from other oral conditions requires a comprehensive assessment. The presence of other COVID-19 symptoms, such as fever, cough, or loss of taste and smell, can be indicative. However, many other conditions, including stress, nutritional deficiencies, or other viral infections, can also cause mouth sores. A thorough medical history and physical examination by a healthcare professional are necessary for accurate diagnosis.
Treatment and Management of COVID-19 Mouth Sores
Treatment for COVID-19 mouth sores focuses primarily on managing the symptoms. Pain relief can be achieved with over-the-counter medications like topical anesthetics or analgesics. For specific conditions like oral thrush or herpes simplex, antifungal or antiviral medications may be prescribed. Maintaining good oral hygiene, including regular brushing and rinsing, can help prevent secondary infections and promote healing. If the sores are severe or persistent, consulting a dentist or doctor is advised. Remember, treating the underlying COVID-19 infection itself is crucial for overall recovery.
When to Seek Medical Attention for COVID-19 Mouth Sores
While many mouth sores resolve on their own, it's essential to seek medical attention if you experience:
- Severe pain
- Persistent sores that don't heal within a few weeks
- Signs of infection, such as increased swelling, redness, or pus
- Difficulty swallowing or eating
- Other concerning COVID-19 symptoms
| Symptom | Possible Cause | Treatment |
|---|---|---|
| Aphthous Ulcers (Canker Sores) | COVID-19, stress, nutritional deficiencies | Topical anesthetics, pain relievers |
| Herpes Simplex Virus Reactivation | COVID-19 (weakened immune system), stress | Antiviral medication |
| Oral Thrush (Candidiasis) | COVID-19 (weakened immune system), antibiotic use | Antifungal medication |
Are mouth sores a symptom of COVID?

Are Mouth Sores a Symptom of COVID?
While mouth sores aren't a commonly reported symptom of COVID-19, some studies have indicated a potential association. The severity and frequency of mouth sores as a COVID-19 symptom are relatively low compared to other, more prevalent symptoms like fever, cough, and loss of taste or smell. However, their presence, especially in conjunction with other COVID-19 symptoms, shouldn't be ignored. It's crucial to remember that many other conditions can cause mouth sores, making it difficult to definitively attribute them solely to COVID-19. Therefore, if you experience mouth sores alongside other COVID-19 symptoms, it's essential to consult a healthcare professional for proper diagnosis and management.
Mouth Sores and COVID-19: Prevalence and Research
Studies on the prevalence of mouth sores as a COVID-19 symptom have yielded varying results. Some studies suggest a relatively small percentage of COVID-19 patients report mouth sores, while others haven't explicitly included them in their symptom lists. This variability might be due to several factors, including the different methodologies used in studies, the varying severity of infections, and the potential for misdiagnosis. Further research is needed to clarify the exact relationship between COVID-19 and mouth sores.
- Limited data exists on the specific types of mouth sores associated with COVID-19.
- More research is needed to establish a clear correlation between mouth sores and COVID-19 infection.
- Inconsistencies in reported prevalence highlight the need for larger, more comprehensive studies.
Differentiating COVID-19 Mouth Sores from Other Oral Conditions
Many oral conditions can cause mouth sores, making it challenging to attribute them solely to COVID-19. These conditions include aphthous ulcers (canker sores), herpes simplex virus (HSV) infections, and various forms of oral thrush (candidiasis). Differentiating between these conditions and COVID-19-related mouth sores requires a thorough clinical evaluation, considering the patient's medical history and other symptoms. A healthcare professional can conduct the necessary examinations and tests to determine the underlying cause of the mouth sores.
- Canker sores are common and usually resolve on their own.
- HSV infections present with characteristic blisters and sores.
- Oral thrush is a fungal infection often associated with weakened immunity.
The Role of Inflammation in COVID-19 and Mouth Sores
COVID-19 is known to trigger a systemic inflammatory response throughout the body. This inflammation could potentially manifest as mouth sores in some individuals. However, the exact mechanisms by which COVID-19 might cause mouth sores are not fully understood. Further research is necessary to investigate the potential inflammatory pathways linking COVID-19 to the development of oral lesions.
- Inflammation is a key feature of COVID-19 infection.
- Systemic inflammation can affect various parts of the body, including the oral mucosa.
- The precise role of inflammation in COVID-19-associated mouth sores requires further study.
When to Seek Medical Attention for Mouth Sores
While many mouth sores resolve spontaneously, it's crucial to seek medical attention if you experience persistent or severe mouth sores, especially when accompanied by other COVID-19 symptoms, such as fever, cough, shortness of breath, or loss of taste and smell. Prompt medical attention can help ensure accurate diagnosis and appropriate management of the underlying condition, regardless of whether it's COVID-19 or another oral health issue.
- Persistent or severe mouth sores warrant medical evaluation.
- Simultaneous occurrence of mouth sores with other COVID-19 symptoms necessitates immediate consultation.
- Early diagnosis and treatment are important for optimal health outcomes.
Limitations of Current Research on Mouth Sores and COVID-19
Currently, research on the relationship between mouth sores and COVID-19 is limited, with inconsistent findings across studies. This is partly due to the challenges in consistently identifying and reporting this symptom, alongside the wide range of other conditions that can cause similar oral lesions. Larger-scale, well-designed studies are needed to establish a clearer understanding of the prevalence and clinical significance of mouth sores as a potential COVID-19 symptom.
- Inconclusive research findings hamper definitive conclusions.
- The lack of standardized reporting methods complicates data analysis.
- Further research is needed to strengthen the evidence base.
What are the oral manifestations of COVID-19 patients?

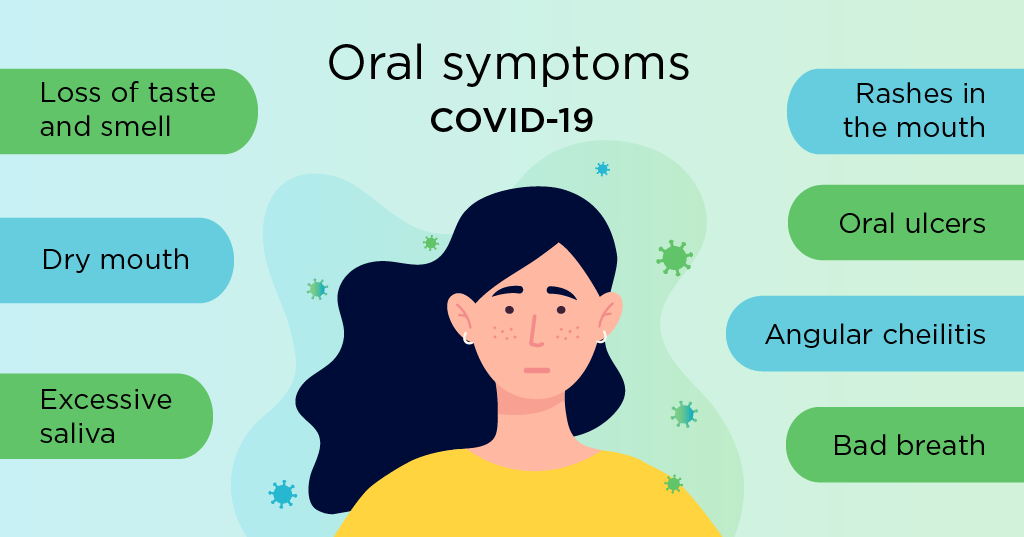
Oral manifestations in COVID-19 patients are diverse and can range from mild to severe. While not all patients experience oral symptoms, their presence can be a significant indicator, especially in early stages of the infection or in asymptomatic individuals. These manifestations are believed to be linked to the virus's direct impact on oral tissues, the body's inflammatory response, and potential side effects of medication used to treat the virus or its complications. The exact prevalence of each manifestation varies depending on the study and population examined.
Loss of Taste and Smell (Ageusia and Anosmia)
Ageusia (loss of taste) and anosmia (loss of smell) are among the most commonly reported oral manifestations of COVID-19. These symptoms are often among the first to appear and can persist for weeks or even months after the initial infection. The mechanism behind this is not fully understood, but it's likely related to the virus's impact on the olfactory and gustatory nerve cells in the nasal cavity and possibly the oral cavity. This loss of taste and smell can significantly impact a patient's quality of life, affecting their appetite and enjoyment of food.
- Ageusia: Complete loss of taste
- Hypogeusia: Reduced taste sensitivity
- Dysgeusia: Distorted or altered taste perception
Oral Ulcers and Lesions
Oral ulcers and lesions, including aphthous ulcers (canker sores) and other types of mucosal lesions, have been reported in COVID-19 patients. These lesions can vary in size, location, and severity. While the exact causal relationship between COVID-19 and oral ulcerations is still being investigated, it's believed that the inflammatory response triggered by the virus and the potential impact on the immune system might play a role. In some cases, these lesions may be attributed to secondary infections or medication side effects.
- Aphthous ulcers (canker sores)
- Herpetiform ulcers
- Other types of mucosal lesions
Xerostomia (Dry Mouth)
Xerostomia, or dry mouth, is another relatively common oral manifestation associated with COVID-19. This can be a direct consequence of the virus itself or an indirect effect of medications used to treat COVID-19, such as certain antiviral drugs. Dehydration, a frequent symptom of COVID-19, also contributes to dry mouth. Dry mouth increases the risk of oral infections and discomfort. Proper hydration and the use of saliva substitutes can help mitigate this symptom.
- Reduced saliva production
- Increased risk of oral infections
- Discomfort and difficulty swallowing
Gingivitis and Periodontal Problems
Gingivitis and other periodontal issues might be exacerbated in COVID-19 patients. The inflammatory nature of the disease, coupled with potential changes in the oral microbiome and reduced oral hygiene due to illness, can contribute to inflammation and bleeding gums. This heightened inflammation in the mouth could also potentially impact the progression of existing periodontal disease. Maintaining diligent oral hygiene is critical during and after recovery from COVID-19.
- Increased gingival inflammation
- Bleeding gums
- Exacerbation of pre-existing periodontal disease
Oral Manifestations and COVID-19 Severity
The presence and severity of oral manifestations in COVID-19 patients do not always correlate with the overall severity of the disease. While some studies suggest a possible link between certain oral symptoms (especially loss of taste and smell) and the risk of severe illness, this relationship needs further investigation. It is essential to remember that the presence of oral symptoms should not be used solely to predict the disease’s severity. Routine medical care and testing are crucial for accurate diagnosis and management.
- Oral manifestations can occur in both mild and severe cases
- Further research is needed to understand the correlation between oral symptoms and disease severity
- Oral symptoms should not be the sole basis for assessing disease severity
What do autoimmune mouth sores look like?

Autoimmune mouth sores, often associated with conditions like Behçet's disease, lupus, or Crohn's disease, don't have a single, definitive appearance. Their characteristics vary depending on the underlying autoimmune disease and the individual's immune response. However, some common features can help distinguish them from other types of mouth sores. They may appear as:
Recurrent aphthous ulcers (RAUs): These are the most common type of mouth sore and can be associated with autoimmune conditions. They typically present as small, shallow ulcers with a yellowish-white base and a red border. They are usually painful and can appear singly or in clusters. However, the frequency and severity of RAUs in autoimmune conditions can be significantly higher than in non-autoimmune individuals. The lack of clear, definitive triggers beyond the underlying autoimmune condition is a key difference.
Larger, deeper ulcers: In more severe autoimmune diseases, mouth sores can be significantly larger and deeper than typical canker sores. They might bleed easily and take longer to heal. The surrounding tissue may be swollen and inflamed. These ulcers can be extremely painful and interfere with eating and speaking.
Unusual location or pattern: While canker sores usually occur on the inside of the lips or cheeks, autoimmune mouth sores might appear in unusual locations, such as the back of the throat or on the gums. The pattern of sores – for instance, widespread or symmetrical distribution – can also be a clue.
Associated symptoms: Autoimmune mouth sores often occur alongside other symptoms of the underlying autoimmune disease. This could include joint pain, skin rashes, fatigue, or eye inflammation. The presence of such accompanying symptoms is a critical indicator.
Resistance to treatment: Standard treatments for canker sores might be less effective for autoimmune mouth sores, requiring more aggressive approaches. Their persistent or recurrent nature, even with treatment, is a significant sign.
Recurrent Aphthous Ulcers (RAUs) in Autoimmune Diseases
RAUs are common mouth sores, but their presentation in autoimmune conditions can differ. While they typically present as small, shallow ulcers with a yellowish-white base and a red border, in autoimmune individuals, the frequency and severity can be markedly increased. This means sores may appear more often and be significantly larger or more painful. They often lack clear triggers besides the underlying autoimmune process.
- Increased frequency compared to non-autoimmune individuals.
- Higher severity, including larger size and greater pain.
- Lack of identifiable triggers beyond the autoimmune disease.
Larger and Deeper Ulcers
In contrast to the typically small size of RAUs, autoimmune mouth sores can be considerably larger and deeper. These ulcers often penetrate deeper into the tissues and can be quite painful and slow-healing. The surrounding tissue may show signs of significant inflammation and swelling, further differentiating them from simple canker sores.
- Increased size and depth of ulceration.
- Prolonged healing time compared to typical canker sores.
- Significant surrounding inflammation and swelling.
Unusual Location and Pattern of Sores
The location and distribution of sores can offer clues. Typical canker sores appear inside the cheeks or lips. However, autoimmune mouth sores might appear in less common spots such as the back of the throat or on the gums. They might also display a characteristic pattern, such as being symmetrical or widespread across the mouth.
- Presence in unusual locations such as the throat or gums.
- Symmetrical distribution of sores across the mouth.
- Widespread pattern of multiple sores.
Associated Systemic Symptoms
Autoimmune mouth sores rarely appear in isolation. They often accompany other symptoms associated with the underlying autoimmune disease. Joint pain, skin rashes, eye inflammation, or fatigue are common examples. The presence of these systemic symptoms strongly suggests a connection to an autoimmune condition.
- Joint pain (arthritis)
- Skin rashes (lupus-like rashes)
- Eye inflammation (uveitis) or other systemic signs.
Resistance to Standard Treatment
Standard treatments used for typical canker sores, such as over-the-counter mouthwashes or topical creams, may prove ineffective against autoimmune mouth sores. This resistance to conventional therapies highlights their distinct nature and usually necessitates more specialized medical attention and potentially stronger medications.
- Ineffectiveness of standard canker sore treatments.
- Need for more aggressive and specialized medical treatment.
- Persistent or recurrent sores despite treatment.
How do you treat COVID-19 in the mouth?
How Do You Treat COVID-19 in the Mouth?
There is no specific treatment for COVID-19 in the mouthitself. COVID-19 is a viral respiratory illness, and while it can manifest in oral symptoms, treating these symptoms focuses on managing the overall infection and alleviating discomfort. Direct treatment of the mouth focuses on managing the symptoms that arise there, not the virus itself. Treatment aims to reduce pain, inflammation, and promote healing. The virus itself needs to be fought through systemic means (treating the whole body), not just the oral cavity.
Oral Hygiene Practices for COVID-19
Maintaining excellent oral hygiene is crucial during a COVID-19 infection, especially since symptoms like dry mouth and sore throat can exacerbate oral health issues. Consistent brushing and flossing help prevent secondary infections and promote healing. Avoiding aggressive brushing is recommended.
- Brush your teeth gently at least twice a day with a soft-bristled toothbrush.
- Floss daily to remove food particles and plaque.
- Use a fluoride mouthwash to strengthen tooth enamel and prevent cavities. Avoid alcohol-based mouthwashes, as they can further dry your mouth.
Managing Oral Pain and Discomfort
COVID-19 can cause oral pain, such as sore throat, mouth ulcers, or gum inflammation. Over-the-counter pain relievers, such as acetaminophen (Tylenol) or ibuprofen (Advil, Motrin), can help manage pain and reduce fever. Rinsing your mouth with warm salt water can also provide relief for sore throats and mouth ulcers.
- Take over-the-counter pain relievers as directed.
- Gently rinse your mouth with warm salt water several times a day.
- Consider using a topical anesthetic gel or spray to numb sore areas if pain is severe.
Addressing Dry Mouth (Xerostomia)
Dry mouth, a common side effect of some COVID-19 medications and the virus itself, increases the risk of oral infections. Staying hydrated is paramount. You can also use sugar-free candies or gum to stimulate saliva production and use an artificial saliva substitute. Avoiding alcohol and tobacco products is also crucial.
- Drink plenty of water throughout the day.
- Chew sugar-free gum or suck on sugar-free candies.
- Use an artificial saliva substitute, available at most pharmacies.
Treating Oral Thrush (Candidiasis)
COVID-19 can suppress the immune system, making individuals more susceptible to oral thrush, a fungal infection characterized by white patches in the mouth. If you suspect oral thrush, consult your doctor as antifungal medication will be needed. Good oral hygiene practices can help prevent and manage the condition.
- Maintain meticulous oral hygiene.
- Avoid sharing eating utensils or drinking glasses.
- Seek medical attention for diagnosis and treatment if you suspect oral thrush.
When to Seek Professional Medical Attention
While many oral symptoms associated with COVID-19 can be managed at home, it's essential to seek professional medical attention if symptoms worsen or persist. Severe pain, persistent bleeding gums, difficulty swallowing, or significant changes in oral appearance warrant a consultation with a doctor or dentist. Timely intervention can help prevent serious complications.
- Contact your physician immediately if you experience severe or persistent oral pain.
- Seek dental attention if you have concerns about bleeding gums, or significant oral changes.
- Consult a medical professional if swallowing becomes difficult or if you have significant concerns about your oral health.
What are COVID mouth sores?
COVID-19, caused by the SARS-CoV-2 virus, can manifest in a variety of ways, and while respiratory symptoms are common, it can also affect other parts of the body. One less frequently discussed symptom is the development of mouth sores, sometimes referred to as COVID mouth sores or COVID-related oral lesions. These sores aren't a defining characteristic of the infection, meaning not everyone with COVID-19 will experience them, but their presence can be another indication of the virus. These sores can take different forms, ranging from small, painful ulcers (aphthous ulcers) to more significant lesions or blisters. The exact mechanism by which the virus causes these oral manifestations isn't fully understood, but it's believed to be related to the virus's impact on the immune system and its ability to directly or indirectly damage oral tissues. Some theories suggest a potential link to inflammation and immune responses within the mouth, leading to the formation of these sores. It's important to remember that while mouth sores can occur alongside COVID-19, they can also be caused by numerous other factors, making it crucial to consult a healthcare professional for accurate diagnosis and treatment.
How common are COVID mouth sores?
The prevalence of mouth sores as a symptom of COVID-19 is not definitively established, and varies greatly depending on the research study. Several studies have reported a significant association between COVID-19 infection and the development of oral lesions, but the frequency varies widely. This variability might be attributed to factors like the specific viral variant, the severity of the infection, the individual's overall health, and even the methodologies employed in data collection. Some studies suggest that mouth sores are relatively uncommon, occurring in only a small percentage of infected individuals, whereas others have observed a higher prevalence, particularly among individuals experiencing more severe symptoms. Additionally, the challenges in accurately identifying COVID-related mouth sores as opposed to other types of oral lesions complicate the estimation of their overall frequency. In short, while a connection exists, pinning down an exact percentage of COVID-19 cases that present with mouth sores remains a challenge, highlighting the need for more comprehensive and standardized research.
What do COVID mouth sores look like?
There isn't a single definitive appearance for COVID-related mouth sores. Their presentation can vary significantly from person to person. They might appear as small, shallow ulcers (aphthous ulcers), which are often painful and white or yellowish in color, surrounded by a reddish halo. Others might experience vesicles (small fluid-filled blisters) or more extensive ulcerative lesions. The location within the mouth can also differ, with some individuals reporting sores on their tongue, gums, inner cheeks, or palate. The size and number of sores can also vary, ranging from a few isolated lesions to multiple widespread ones. Crucially, these oral manifestations are often not easily distinguishable from other causes of mouth sores, making a definitive visual diagnosis without further investigation impossible. Therefore, any persistent or concerning mouth sores, especially in the context of suspected or confirmed COVID-19 infection, should be assessed by a healthcare professional.
Should I be concerned if I develop mouth sores during a COVID-19 infection?
While mouth sores are not necessarily a cause for significant alarm in themselves, their appearance during a COVID-19 infection warrants attention. The presence of mouth sores, alongside other symptoms, can contribute to a more complete clinical picture, aiding in the diagnosis and management of the infection. The severity of the sores and other associated symptoms should guide the level of concern. Minor sores that resolve quickly might not require specific treatment beyond over-the-counter pain relief and good oral hygiene. However, if the sores are particularly painful, persistent, extensive, or accompanied by other concerning symptoms like difficulty swallowing or breathing, it's crucial to seek medical advice. Furthermore, if you develop mouth sores and suspect you have COVID-19, reporting this to your healthcare provider can help them assess the overall severity of your infection and ensure appropriate care. In short, while not automatically indicative of a serious complication, unexpected mouth sores during a COVID-19 infection shouldn't be ignored; proper evaluation by a medical professional is recommended to ensure timely and effective management.
Deja una respuesta